
TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
What is TNFi therapy?
Currently, there is no standard approach for the management of TNF inhibitor-induced psoriasis. Here, we conduct a literature review on TNF inhibitor-induced psoriasis and introduce a novel treatment algorithm for maintaining otherwise effective anti-TNF therapy versus switching to a different class as appropriate in the management of patients with IBD, RA, psoriasis, or PsA.
Are all TNF blockers given by injection?
Ustekinumab is a treatment option for moderate to severe psoriasis and PsA, which can efficiently treat TNF inhibitor-induced psoriasis. 85 Two case reports saw resolution of psoriasiform eruptions secondary to adalimumab in females with PsA treated with ustekinumab every 3 months. 86 Furthermore, ustekinumab has also been implicated in successfully …
Is psoriasis a cutaneous disease or systemic disease?
· Cases resistant to topicals alone were treated with other modalities, including phototherapy, addition/switch to traditional systemic immunomodulatory agents and discontinuation/switch to another TNFI. Forty out of 62 patients prescribed only topicals saw improvement or resolution of their TNFI-induced psoriasis.
Does psoriasis only affect the skin?
Abstract. Tumor necrosis factor α (TNF-α)-targeted therapies have expanded the therapeutic options for patients with inflammatory bowel disease (IBD), rheumatoid arthritis (RA), psoriasis, and psoriatic arthritis (PsA) and have significantly improved patients’ quality of life. Paradoxically, anti-TNF-α agents may induce psoriatic eruptions or worsen preexisting psoriatic skin disease.
Does drug induced psoriasis go away?
While some cases of drug-induced psoriasis can resolve within weeks of stopping the causative medicine, in other cases, it can take much longer to resolve or not resolve completely.
How do you control TNF?
Anti-TNFα drugs control inflammation in inflammatory skin diseases, arthritis, and bowel disease. They were among the first biologic agents on the market. Anti-TNFα monoclonal antibodies include: Infliximab....Other drugs with activity against TNF include:Thalidomide.Sulfasalazine.Pentoxifylline.Bupropion.
What drugs are used currently to block TNF?
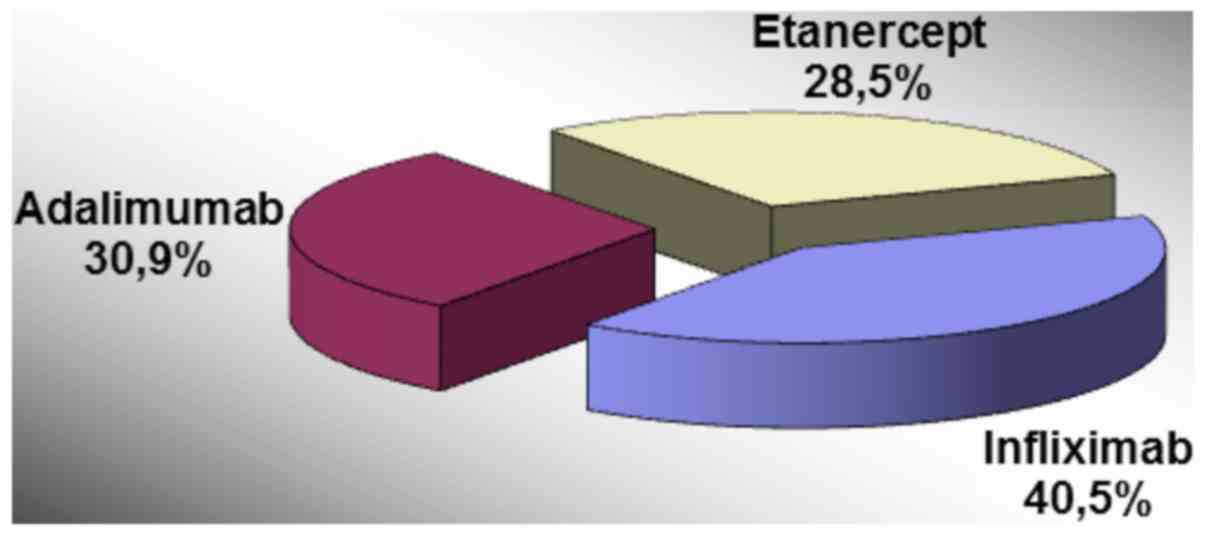
The drugs in this class include Remicade (infliximab), Enbrel (etanercept), Humira (adalimumab), Cimzia (certolizumab pegol) and Simponi (golimumab). This information reflects FDA's current analysis of data available to FDA concerning this drug.
How long does drug induced psoriasis last?
Both psoriasiform eruption and drug-induced/aggravated psoriasis from beta-blocker therapy usually appear at 1 to 18 months after initiation of therapy. In psoriasiform eruptions, lesions clear after several weeks of discontinuing the medication.
What is the best TNF blocker?
Your doctor will help find one that is available and that's best for you:Etanercept (Enbrel)Etanercept-szzs (Ereizi), a biosimilar to Enbrel.Golimumab (Simponi, Simponi Aria)Infliximab (Remicade)Infliximab-abda (Renflexis) a biosimilar to Remicade.Infliximab-dyyb (Inflectra), a biosimilar to Remicade.More items...
What is the safest TNF blocker?
Combining results from studies involving nearly 12,000 rheumatoid arthritis patients finds the fusion protein etanercept less likely than other TNF inhibitors to be discontinued due to infections.
Is rituximab an anti-TNF drug?
Rituxan Is an RA Treatment That Works Differently Overactive B-cells are believed to play a role in the symptoms and joint damage of RA. An anti-TNF, or anti-tumor necrosis factor, is usually the first biologic given upon diagnosis with RA.
Is methotrexate a TNF blocker?
Methotrexate primarily inhibits the activation and proliferation of lymphocytes. TNF inhibitors suppress monocytes and myeloid dendritic cells, and tocilizumab has a broader activity and is directed against both the lymphoid as well as the myeloid compartment.
Is Cosentyx a TNF blocker?
Humira is also used to treat Crohn's disease after other drugs have been tried without successful treatment of symptoms. Cosentyx and Humira are different types of monoclonal antibodies. Cosentyx is a monoclonal antibody to interleukin-17A and Humira is a tumor necrosis factor (TNF) blocker.
What is the first-line treatment for psoriasis?
Light therapy. Light therapy is a first-line treatment for moderate to severe psoriasis, either alone or in combination with medications. It involves exposing the skin to controlled amounts of natural or artificial light.
Can Humira make psoriasis worse?
Humira can also cause new or worsening psoriasis. * This is a skin condition that causes symptoms such as red scaly patches of skin, and raised bumps that contain pus. This side effect was not seen in clinical trials, but has been reported since the drug was approved.
What medications make psoriasis worse?
Medications That Can Trigger PsoriasisBeta-Blockers.Lithium.Antimalarials.Interferons.Terbinafine.ACE Inhibitors.TNF Blockers.Other Drugs.More items...•
Review is largest study to date of poorly understood entity
While TNF-α inhibitors (TNFIs) have revolutionized the management of several debilitating chronic inflammatory diseases, they can also cause adverse side effects including, paradoxically, de novo psoriasiform eruptions. Researchers reported the first case of TNFI-induced psoriasis in 2003, yet it remains poorly understood.
Study characteristics
Dr. Fernandez and his colleagues searched electronic medical records for patients who were diagnosed with TNFI-induced psoriasis and were managed or comanaged by a dermatologist between 2003 and 2013.
Improvement with topicals alone
Sixty-four percent of patients initially received topical medications alone. Cases resistant to topicals alone were treated with other modalities, including phototherapy, addition/switch to traditional systemic immunomodulatory agents and discontinuation/switch to another TNFI.
Cite
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click on download.
Request Permissions
Sara Jiayang Li, BS, Brigham and Women’s Hospital, Department of Dermatology, Harvard Medical School, 221 Longwood Avenue, Boston, MA 02115, USA. Email: [email protected]
