Warfarin is taken for a period ranging from a few weeks to lifelong, depending on the individual’s diagnosis and future clot risks. It works by inhibiting the liver’s ability to make coagulation proteins that require vitamin K for their synthesis.
Full Answer
Is there a best time of day to take warfarin?
We recommend 5:00 p.m. Warfarin can be taken before or after eating. If you forget to take your dose and remember within eight hours of the time you were supposed to take your dose, take the dose. If it is past eight hours, wait until the next day and take only the prescribed dose for that day.
What time of Day should I take warfarin?
Warfarin
- When warfarin is prescribed
- Taking warfarin. It's very important that you take warfarin exactly as directed. ...
- Side effects of warfarin. Bleeding is the main side effect associated with warfarin, as it slows down the blood's normal clotting ability.
- Interactions. Warfarin can interact with many other medicines. ...
- Other useful information. ...
How long does warfarin stay in our system?
Warfarin or Coumadin (warfarin) is an oral anticoagulant which remains in the system about 72 hours or 3 days. We tell patients who are on this medic... Read More Ask U.S. doctors your own question and get educational, text answers — it's anonymous and free! Doctors typically provide answers within 24 hours.
What to know when taking warfarin?
What to Know When Taking Warfarin
- Before you start warfarin. Many medicines cause problems if you take them while you’re on warfarin. ...
- Taking your warfarin as directed. You’ll need to take the medicine exactly as directed by your doctor. ...
- Keeping certain foods steady in your diet. ...
- Preventing injury. ...
- Getting your blood tested. ...
- Important tips. ...
- Call 911. ...
- When to call your healthcare provider. ...
How long should a patient be treated with warfarin?
INR = International Normalized Ratio. *—One study 6 suggested that 4 weeks may be an adequate duration of oral anticoagulant therapy in patients without continuing risk factors. †—If oral anticoagulant therapy is elected to prevent recurrent myocardial infarction, an INR of 2.5 to 3.5 is recommended.
How long can you take warfarin?
As a general rule warfarin is prescribed to treat a blood clot for 3 – 6 months. For an irregular heart beat, recurrent blood clots or some heart valve problems, warfarin is prescribed indefinitely.
How many days does it take for warfarin to be fully anticoagulated?
As the antithrombotic effect of warfarin necessitates the inhibition of factor II, which has a very long half-life (60-72 h) as compared to other factors (6-24 h), it takes approximately 6 days for warfarin to exert its full efficacy even though the earliest changes in INR can be seen after 24 to 36 h [8,9,10,11].
When should warfarin be stopped?
For elective procedures, warfarin should be stopped for 5 to 6 days prior to the procedure to allow gradual normalization of the international normalized ratio (INR).
Can warfarin be stopped suddenly?
New research shows that while these patients benefit from their warfarin treatment, they risk getting a blood clot in their brain if they suddenly stop taking warfarin. A blood clot in the brain can result in paralysis in the body – and can be fatal.
How long should you be on blood thinners?
Blood thinner treatment for PE is usually advised for at least 3-6 months. Your healthcare provider may advise a longer course depending on why you had the blood clot. Some people at high risk of blood clots may stay on blood thinner indefinitely.
How do you titrate warfarin?
A nice "rule of thumb" for dose adjustments near the target range (generally works for INRs from the high 1s to low 4s): If you want to change the INR by 0.5-1 unit, increase or decrease the weekly dose by a daily dose. Example: Your patient has been taking warfarin 5mg daily for more than 2 weeks and INR is 1.8.
Why does warfarin take 72 hours to work?
How long does warfarin take to work? Warfarin takes about three days to build up its full anticoagulant effect. This is because it takes about this long for existing clotting factors to be used up.
What is the therapeutic range for warfarin?
The time in the therapeutic range (an international normalized ratio [INR] between 2.0 and 3.0) (TTR) has been used as a measure of warfarin (W) therapy quality.
How long does it take for INR to drop after stopping warfarin?
In 5 patients studied in detail, the INR decreased exponentially and had a half-life that ranged from 0.52 to 1.2 days; the onset of maximal decrease began 24 to 36 hours after discontinuation of warfarin therapy.
Do you need to wean off warfarin?
Stopping warfarin in and of itself is not harmful. That is, you don't have to slowly taper off your dose of warfarin before you stop taking it completely to avoid side effects, as is the case with some medications.
When is bridging therapy necessary?
The intent of bridge anticoagulant therapy is to minimize both the risk of thromboembolic events and the risk of bleeding during the peri-operative period. Bridging anticoagulant therapy is appropriate for some but not all patients undergoing medical procedures.
Usual Adult Dose for Prevention of Thromboembolism in Atrial Fibrillation
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day Target INR: 2.5 (range: 2 to 3) Duration of therapy: Indefinite Comments: -For patients with atrial fibrillation (AF) and prosthetic heart valves, target INR may be increased depending on valve type, valve position, and patient factors. -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Prophylaxis and treatment of thromboembolic complications associated with AF..
Usual Adult Dose for Thromboembolic Stroke Prophylaxis
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day Target INR: 2.5 (range: 2 to 3) Duration of therapy: Indefinite Comments: -For patients with atrial fibrillation (AF) and prosthetic heart valves, target INR may be increased depending on valve type, valve position, and patient factors. -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Prophylaxis and treatment of thromboembolic complications associated with AF..
Usual Adult Dose for Myocardial Infarction
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day INR: 2 to 3 Duration of therapy: At least 3 months after myocardial infarction Comments: -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction..
Usual Adult Dose for Myocardial Infarction - Prophylaxis
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day INR: 2 to 3 Duration of therapy: At least 3 months after myocardial infarction Comments: -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Reduction in the risk of death, recurrent myocardial infarction (MI), and thromboembolic events such as stroke or systemic embolization after myocardial infarction..
Usual Adult Dose for Deep Vein Thrombosis - Prophylaxis
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day Target INR: 2.5 (range: 2 to 3) Duration of therapy: -Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months -Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months. -Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment. Comments: -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Prophylaxis and treatment of venous thrombosis and PE..
Usual Adult Dose for Pulmonary Embolism
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day Target INR: 2.5 (range: 2 to 3) Duration of therapy: -Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months -Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months. -Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment. Comments: -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Prophylaxis and treatment of venous thrombosis and PE..
Usual Adult Dose for Deep Vein Thrombosis - First Event
Initial dose: 2 to 5 mg orally once a day Maintenance dose: 2 to 10 mg orally once a day Target INR: 2.5 (range: 2 to 3) Duration of therapy: -Deep venous thrombosis (DVT) or pulmonary embolism (PE) secondary to a reversible risk factor: 3 months -Unprovoked DVT or PE: At least 3 months; evaluate risk-benefit ratio of long-term treatment after 3 months. -Two episodes of unprovoked DVT or PE: Indefinite; periodically reassess risk-benefit ratio of continuing such treatment. Comments: -Initial dose is influenced by age, race, body weight, gender, concomitant medications, comorbidities, genetic variation, and possibly other factors. -Dosage and administration must be individualized according to the patient's INR and condition being treated. Use: Prophylaxis and treatment of venous thrombosis and PE..
How long does it take to retesting warfarin?
For patients with previously stable therapeutic INRs presenting with a single out-of-range INR of ≤ 0.3 INR units below or above the therapeutic range we suggest continuing the current warfarin dose and retesting the INR within 7–14 days. We suggest against the routine use of boost or skipped warfarin doses for unexplained slightly out of range INRs.
How to ensure patients on warfarin are not lost to follow up?
To ensure patients on warfarin are not lost to follow up we suggest use of a systematic tracking process.
What is the target INR range for APLA?
For patients with VTE associated with APLA syndrome, we suggest warfarin adjusted to a target INR range 2.0–3.0 is the best option for long-term treatment [ 43 ].
What is the best anticoagulant for CrCl?
For patients with CrCl < 30 mL/min (estimated using the Cockroft–Gault equation) we suggest warfarin is the preferred anticoagulant. We also suggest vigilant monitoring including more frequent INR testing and bleeding risk assessment in patients with CrCl < 30 mL/min.
Why is warfarin preferred over anticoagulant?
When avoiding drugs known to interact with a given anticoagulant is not an option, we suggest that warfarin is preferred because dose adjustments based on INR monitoring can facilitate titration of the anticoagulant response.
How long does it take for DOAC to start?
As a general rule, we suggest that each DOAC can be started within 30 min after stopping (iv) UFH
When determining warfarin doses during VTE treatment, do we suggest using computer-aided warfarin?
When determining warfarin doses during VTE treatment we suggest using computer-aided warfarin dosing programs or validated dosing algorithms over an ad hoc approach.
When to restart warfarin?
Omit next few warfarin doses and/or restart at lower dose when INR approaches desired range. If the INR is only minimally above range, no dosage reduction may be required.
How long does it take for warfarin to change INR?
The earliest changes in INR are typically seen 24 to 36 hours after administration of the dose. The antithrombotic effect of warfarin is not present ...
How long does it take for heparin to work with warfarin?
Another area of improvement relates to the practice of overlapping heparin with warfarin therapy. Heparin displays an anticoagulant effect within 1 day, while the anticoagulant effects of warfarin are not evident until the third day of therapy. If rapid anticoagulant effects are needed, heparin should be initiated first, and warfarin should be started within a day or two. The 2 drugs should be given concurrently until the INR value is within the therapeutic range (1–3).
What are the 4 variances in warfarin?
Overall, results identified 4 main variances related to warfarin therapy: 1) inappropriate administration of a warfarin loading dose, 2) inappropriate use of vitamin K, 3) inconsistent overlapping of heparin with warfarin, and 4) inconsistent provision of patient education.
How long does prothrombin last?
Because prothrombin has a half-life of around 50 hours, loading doses of warfarin are of limited value (4). In clinical practice, loading doses (e.g., 7.5 mg or more per day) of warfarin may increase the patient's risk of bleeding complications early in therapy by eliminating the production of functional factor VII (2, 5).
What is the treatment for venous thrombosis?
Warfarin, a vitamin K antagonist, is an oral anticoagulant indicated for the prevention and treatment of venous thrombosis and its extension and the prevention and treatment of the thromboembolic complications associated with atrial fibrillation.
How much vitamin K1by to take with prothrombin?
Replace with prothrombin complex concentrate and give 10 mg of vitamin K1by infusion. May repeat if needed.
How to reduce bleeding while taking warfarin?
Some simple changes to decrease the risk of bleeding while taking warfarin include the following: Use a soft-bristle toothbrush. Floss with waxed floss rather than unwaxed floss. Shave with an electric razor rather than a blade. Take care when using sharp objects, such as knives and scissors.
Why is warfarin called an anticoagulant?
Because warfarin interferes with the formation of blood clots, it is called an anticoagulant (PDF). Many people refer to anticoagulants as *blood thinners; however, warfarin does not thin the blood but instead causes the blood to take longer to form a clot.
How does warfarin affect blood clotting?
The goal of warfarin therapy is to decrease the clotting tendency of blood, not to prevent clotting completely. Therefore, the effect of warfarin must be monitored carefully with blood testing. On the basis of the results of the blood test, your daily dose of warfarin will be adjusted to keep your clotting time within a target range. The blood test used to measure the time it takes for blood to clot is referred to as a prothrombin time test, or protime (PT). The PT is reported as the International Normalized Ratio (INR).
What is the INR of a PT?
The INR is a standardized way of expressing the PT value. The INR ensures that PT results obtained by different laboratories can be compared. It is important to monitor the INR (at least once a month and sometimes as often as twice weekly) to make sure that the level of warfarin remains in the effective range. If the INR is too low, blood clots will not be prevented, but if the INR is too high, there is an increased risk of bleeding. This is why those who take warfarin must have their blood tested so frequently.
What to wear for warfarin?
Wear Medical Identification. Those who require long-term warfarin should wear a medical alert bracelet, necklace, or similar alert tag at all times. If an accident occurs and the person is too ill to communicate, a medical alert tag will help responders provide appropriate care.
Does warfarin help with blood clots?
Warfarin decreases the body’s ability to form blood clots by blocking the formation of vitamin K–dependent clotting factors. Vitamin K is needed to make clotting factors and prevent bleeding. Therefore, by giving a medication that blocks the clotting factors, your body can stop harmful clots from forming and prevent clots from getting larger.
Is Warfarin a foreign drug?
Foreign drugs may use identical or potentially confusing brand names for products with active ingredients that differ from U.S. drugs. Warfarin has many foreign brand names (Table 1). Patients who do fill prescriptions abroad should ensure the accuracy and quality of the medication dispensed.
How does warfarin work?
How Warfarin Works. Warfarin interferes with the hepatic synthesis of clotting factors, which are vitamin-K-dependent, thus preventing the process of coagulation and the formation of any new clots. Until it settles in, warfarin is paired with a parenteral or injectable anticoagulant like Lovenox (enoxaparin injection).
What is the normal INR level for warfarin?
In most people, normal INR levels range from 0.8 to 1.2. People on warfarin are typically maintained at an INR level between 2 and 3, meaning that these patients are significantly more anticoagulated (have thinner blood) than average people.
Who Needs Higher Doses?
Higher doses of warfarin may be required for the following populations:
How long after leaving hospital can you take anticoagulants?
Mary Choy, PharmD. Updated on October 25, 2020. If you've been treated for deep venous thrombosis, you can expect at least three months of continued anticoagulants or blood-thinning medication after you leave the hospital. Deep venous thrombosis is a dangerous condition in which your body forms a clot, ...
Does warfarin lower INR?
Because warfarin is a vitamin K antagonist, a diet rich in vitamin K can lower your INR levels. Specifically, green and leafy vegetables tend to be high in vitamin K. On the other hand, potatoes, fruits, and cereals are low in vitamin K.
Does warfarin interfere with clotting factors?
Warfarin interferes with the hepatic synthesis of clotting factors, which are vitamin K dependent. It prevents the process of coagulation and the formation of any new clots. Until it settles in and you've been on it awhile, warfarin is paired with a parenteral, or injectable, anticoagulant like Lovenox (enoxaparin injection).
Can you continue anticoagulant therapy after a stroke?
With continued anticoagulant therapy after you leave the hospital, you minimize the risk of re-forming such deadly blood clots. Note that anticoagulant therapy is not only given with deep venous thrombosis. For example, if you are currently being treated for stroke or have a condition that increases your risk for clots (a hypercoagulable condition), you can expect a lifetime of anticoagulation therapy.
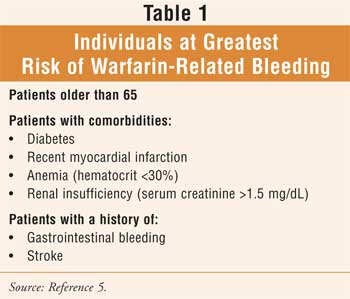
What should be assessed before initiating warfarin therapy?
Before initiating warfarin therapy the patient should be assessed for risk factors that may increase their risk for bleeding, thromboembolic events and for risk factors that may impact the sensitivity of the response to warfarin.2,3 (Class I, Level C)
How long does INR stay within goal?
12. Prior to cardioversion procedure the INR must remain within goal for 30 days.4 If an INR is trending downward consider increasing the warfarin dose to prevent a subtherapeutic INR
What should be assessed at each encounter for INR monitoring patients?
At each encounter for INR monitoring patients should be assessed for signs and symptoms of bleeding and clotting as well as any change that could affect the INR result2,3. (Class I, Level C)
What is a grade in a clinical practice guideline?
For all other recommendations a modified Grading of Recommendations Assessment, Development and Evaluation (GRADE) developed by the American Heart Association and American College of Cardiology (Figure 1.) has been used to assess the Quality and Strength of the Evidence in this Clinical Practice Guideline.1
Does vitamin K affect warfarin?
Patients on long term warfarin therapy can be sensitive to the fluctuating levels of vitamin K from both external dietary sources and internal gastrointestinal sources. Increased dietary intake of vitamin K from either food sources or nutritional supplement sources can reduce the effectiveness of warfarin and decrease the INR. Since warfarin is a high protein bound drug with up to 99% of the drug bound to plasma proteins, patients who are malnourished with low albumin levels will have higher concentrations of unbound drug and may experience faster INR response. Conversely, patients receiving enteral nutrition will have more bound drug due to the high protein concentration in these products.3,12,14-16
Is Warfarin adjusted based on INR?
Warfarin should be adjusted based on current INR measurements and assessment of any missed doses, recent INR trends, changes in diet and activity level, potential drug interactions, symptoms of bleeding or clotting and other changes that may affect INR level as described in Appendix A. Patient Assessment Tool2,3 (Class I, Level C)
Is standardization of warfarin management unrealistic?
Since standardization of warfarin management is unrealistic, clinical judgement should be used when indicated to prevent unwanted adverse events
When to use 10 mg initiation nomogram?
The 10mg initiation nomogram should only be used in relatively young and healthy patients who are likely to be insensitive to warfarin, or in patients taking concurrent medications known to induce warfarin metabolism.
Is 5 mg initiation as fast as 10 mg?
Several studies have confirmed that 5mg initiation achieves therapeutic anticoagulation as rapidly as 10mg initiation but with a lower frequency of supra-therapeutic INRs. The 10mg initiation nomogram should only be used in relatively young and healthy patients who are likely to be insensitive to warfarin, or in patients taking concurrent ...