Medication
In general, guidelines recommend ablation for patients with recurrent SVT despite treatment or poorly tolerated SVT, although recommendations vary based on the category of SVT and known success rates (Table).27,33Most SVT ablation is performed under conscious sedation.
Procedures
Coughing can help in managing an SVT episode. However, you have to cough hard – the harder you can cough, the better your ability to manage an SVT episode. Coughing has a similar effect to the Valsalva maneuver. It increases the pressure in your chest and throat.
Therapy
There are two major types of SVT medications. Rate control medications return the heart to a normal pace. Rhythm control medications (arrhythmic drugs) restore an organized heartbeat. Either will be used depending on the type and severity of the patient’s condition.
Nutrition
EPIDEMIOLOGY OF SVT SVT is a common entity in clinical practice and a relatively common occurrence in the emergency department.
See more
What are the guidelines for the treatment of SVT?
How to manage an SVT episode?
What are the different types of SVT medications?
How common is SVT in the emergency department?

How long can a patient stay in SVT?
The main symptom of supraventricular tachycardia (SVT) is a very fast heartbeat (100 beats a minute or more) that may last for a few minutes to a few days.
How often do SVT episodes happen?
The estimated frequency of SVT episodes ranged from 2–4 times a year to greater than 3 times a day (mean four times per week).
How do I permanently get rid of SVT?
catheter ablation – a treatment where thin tubes are placed through a vein or artery into your heart to correct the problem with the electrical system; this permanently cures the problem in most patients.
How is recurrent SVT treated?
If you have recurring episodes of SVT, you may need to take medicines, either on an as-needed basis or daily. Medicine treatment may include beta-blockers, calcium channel blockers, or other antiarrhythmic medicines. In people who have frequent episodes, treatment with medicines can decrease how often these occur.
Is SVT ablation worth it?
Catheter ablation works well to stop supraventricular tachycardia (SVT) and the symptoms it causes. How well it works can depend on the type of SVT. These success rates cover the more common SVT types called AVNRT (atrioventricular nodal re-entrant tachycardia) and AVRT (atrioventricular reciprocating tachycardia).
How do you prevent SVT episodes?
Lifestyle changes to help prevent SVT episodesHave less alcohol and caffeine.Don't smoke.Lower your stress.Eat foods that are healthy for your heart.Don't take recreational drugs, especially stimulants that can over-excite the heart muscle. ... Stay well hydrated and get enough sleep.
How many times can adenosine be given?
In light of this adenosine should be administered by RAPID intravenous bolus so that a significant bolus of adenosine reaches the heart before it is metabolized. A change from the 2010 guidelines now has adenosine given up to two times rather than three.
How many times can you have heart ablation?
Does Ablation Cure AFib? AFib may go away for a long time, but it can return. It's rare, but if you have persistent or chronic AFib, you might need a second ablation within 1 year. If you've had AFib for more than a year, you may need one or more treatments to fix the problem.
Does SVT shorten your life?
In the vast majority of cases SVT is a benign condition. This means that it will not cause sudden death, will not damage the heart or cause a heart attack and will not shorten life expectancy.
Do beta-blockers stop SVT?
Medications typically used to treat SVT are: Beta Blockers: A beta blocker is a very safe medication that works by reducing the effect adrenalin has on the heart. Beta blockers are commonly used to treat high blood pressure and other common heart problems. Calcium Channel Blockers.
Can SVT be cured with ablation?
Heart ablation can be very effective at treating SVT. Overall, it's estimated that over 80 percent of people are cured of SVT after having a heart ablation procedure.
How much metoprolol should I take for SVT?
Table 2. Acute Treatment of SVTIV diltiazem5 mg to 20 mg IV pushEffective Easy to administer IV drip can be continuedIV metoprolol5 mg IV pushEffective Repeat dosing can be doneIV digoxin0.125 mg to 1.0 mg IV pushIV esmolol50 to 300 micrograms/kg/min6 more rows•Nov 1, 2020
How to stop SVT?
You may be able to stop an episode of SVT by using particular movements such as holding your breath and straining as you would during a bowel movement, dunking your face in ice water, or coughing.
What is the test for SVT?
Tests to diagnosis SVT include: Electrocardiogram (ECG). During an ECG, sensors (electrodes) that can detect the electrical activity of your heart are attached to your chest and sometimes to your limbs. An ECG measures the timing and duration of each electrical phase in your heartbeat. Holter monitor.
What is a supraventricular tachycardia test?
This device detects abnormal heart rhythms and is implanted under the skin in the chest area. If your doctor doesn't find a heart rhythm problem during those tests, you may need other tests, such as: Stress test. For some people, supraventricular tachycardia is triggered or worsened by stress or exercise.
How to diagnose supraventricular tachycardia?
To diagnose supraventricular tachycardia, your doctor will ask questions about your symptoms and your medical history and perform a physical exam. Blood tests are usually done to check for other health conditions that could cause your symptoms, such as thyroid disease.
How does cardioversion work?
Cardioversion may be done using medications or during a heart procedure. In the procedure, a shock is delivered to your heart through paddles or patches on your chest. The current affects the electrical signals in your heart and can restore a normal rhythm. Medications.
How to prevent SVT?
Your healthcare provider might suggest other ways to help prevent SVT, such as the following: 1 Have less alcohol and caffeine 2 Don't smoke 3 Lower your stress 4 Eat foods that are healthy for your heart 5 Don't take recreational drugs, especially stimulants that can over-excite the heart muscle. Some herbs and supplements can have this same effect. Always check with your healthcare team before you take any non-prescribed medicines. 6 Stay well hydrated and get enough sleep
What medicine can be given to prevent SVT?
For emergent cases, calcium channel or beta blockers can be given through IV (intravenously) for more rapid correction of the heart rhythm. Adenosine is another medicince that can be given through IV as well that can work in a matter of seconds.
How fast does a ventricular rate vary in SVT?
Understanding the underlying mechanism is useful in understanding the clues on ECG. Ventricular rates in SVT may vary from 150 to 250 beats/min. However, the rate may be slower in older patients and in patients taking AV nodal blocking medications (i.e., calcium-channel blockers, β-blockers and digoxin).7
What level of evidence is needed for SVT?
Patients with SVT should be educated on how to perform vagal manoeuvres for ongoing management of SVT (class I recommendation, level C-LD evidence)
What is a supraventricular tachycardia?
Supraventricular tachycardias are usually narrow-complex tachycardias with a QRS interval of 100 ms or less on an electrocardiogram (ECG). Occasionally, they may show a wide QRS complex in the case of a pre-existing conduction delay, an aberrancy due to rate-related conduction delay or a bundle branch block.
When is synchronized cardioversion recommended?
Synchronized cardioversion is recommended for acute treatment in patients with hemodynamically stable SVT when pharmacologic treatment is ineffective or contraindicated ( class I recommendation, level B-NR evidence)
Is verapamil a class IIA drug?
Intravenous administration of diltiazem or verapamil can be effective for acute treatment in patients with hemodynamically stable SVT (class IIa recommendation, level B- R evidence)
Is AVNRT a sinus rhythm?
A narrow-complex tachycardia with a regular rhythm is likely to be sinus tachycardia, AVRT, AVNRT, atrial flutter or atrial tachycardia.
What is SVT?
Supraventricular tachycardia occurs when the heart occasionally beats too fast for no identifiable reason. A glitch in nerve signals rather than a problem with heart muscles causes the heart to beat too fast (tachycardia).
How is SVT diagnosed?
Supraventricular tachycardia is diagnosed from the patient’s symptoms and an electrocardiogram (ECG), a device that measures the heart’s electrical activity. The most common symptoms of supraventricular tachycardia include:
What is the best medication for SVT?
The mechanism and symptoms of supraventricular tachycardia can vary widely between patients, so there is no “best” medication for SVT. The management of supraventricular tachycardia will depend on the type of SVT, the symptoms, and the patient’s overall medical situation and tolerance for side effects.
What is the best home remedy for SVT?
In most people, lifestyle changes and home remedies are enough to manage and prevent supraventricular tachycardia. However, if symptoms persist or breathing becomes difficult, immediate medical help is needed.
What is AVRT in heart?
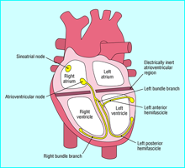
Atrioventricular reciprocating tachycardia (AVRT) happens when the nerve signal passes to the ventricles through the AV node but also an extra electrical connection exists that bridges the atrium and ventricle which can conduct electricity - known as an accessory pathway. The heart can get caught up in a looping circuit where electricity either goes down the AV node and returns back to the atrium through the accessory pathway, or the reverse happens with the signal traveling down the accessory pathway and returns through the AV node. Again, one heartbeat can produce two or more additional heartbeats as the electrical signal cycles back on itself. This is the most common form of SVT found in infants and children.
What is the name of the tachycardia that happens when you have two channels through the AV no?
Atrioventricular nodal reentrant tachycardia (AVNRT), also called paroxysmal supraventricular tachycardia (PSVT), happens when you have two channels through the AV node so that the nerve signal not only passes through the AV node to the lower chambers but simultaneously circles around the AV node back to the atria, causing the upper chambers to contract a second time. Round and round the signal can go, making the upper chambers beat very quickly with a rapid and regular ventricular responseAVNRT is the most common form of SVT among adults, particularly in women and older adults.
What is the best diet for supraventricular tachycardia?
There is no magic diet for supraventricular tachycardia. It’s enough to say that many minerals and vitamins are necessary for nerves and muscles to function properly. In particular, potassium, magnesium, calcium, and even sodium play an outsized role in nerve conduction and muscle contraction. Too little or too much of these minerals will cause problems. Eat a healthy diet sufficient in nutrients and minerals without overdoing it.
What is the most common SVT?
Of the remaining subtypes of SVT, atrioventricular nodal reentrant tachycardia (AVNRT) is the most common, accounting for approximately 60% of cases. The subtypes atrioventricular reentrant tachycardia (AVRT) and atrial tachycardia account for approximately 30% and 10% of SVT cases, respectively. AVNRT is more common in women and has a bimodal age distribution with one peak in the third decade and another that begins in the sixth decade and extends to very old age. AVRT is more common in men and has a mean onset age of 23 years. The incidence of atrial tachycardia increases with age and is more common in patients with structural heart disease.2
What is AVNRT in SVT?
AVNRT is the most commonly encountered paroxysmal SVT. Patients with AVNRT demonstrate dual atrioventricular nodal inputs with differing electrophysiologic properties, the fast and slow pathways that act as the 2 limbs of the reentrant circuit. An estimated 32%-40% of the normal population have dual atrioventricular nodal physiology, although only a minority of these develop AVNRT.7The fast pathway inputs into the apex of the triangle of Koch near the compact atrioventricular node. The slow pathway inputs near the os of the coronary sinus at the base of the triangle. In the typical form (slow-fast AVNRT), conduction occurs antegrade via the slow pathway and retrograde via the fast pathway. Atypical forms of AVNRT such as fast-slow and slow-slow are also encountered and are one of the causes of long RP tachycardia.8,9
What is reentry in a ventricular system?
Reentry involves repetitive impulse propagation around 2 pathways or limbs, separated by a zone of nonexcitability.3-6For reentry to occur, the 2 limbs should have differing electrophysiologic properties (conduction velocity and refractory period). Atrial or ventricular premature beats or runs of tachycardia (automatic or triggered in origin) result in a unidirectional block in one limb with circular repetitive reentry in the opposite direction (Figure 1). Reentry is the mechanism of all cases of AVNRT and AVRT and of some cases of atrial tachycardia.
What is supraventricular tachycardia?
Background. Supraventricular tachycardia (SVT) is a general term describing a group of arrhythmias whose mechanism involves or is above the atrioventricular node. The mechanisms of most forms of SVT have been elucidated, and pharmacologic and invasive therapies have evolved simultaneously.
Is tachycardia a reentrant?
Atrioventricular nodal reentrant tachycardia (far left) and atrioventricular reciprocating tachycardia (middle) are exclusively reentrant in mechanism. Atrial arrhythmias include atrial tachycardia, atrial flutter, and fibrillation and may be because of reentry, automaticity (star), or triggered activity (T) (far right).
Does SVT have a QRS complex?
SVT usually exhibits a narrow QRS complex tachycardia, although wide complex tachycardia may occur in the case of SVT with preexisting or rate-related bundle branch block. Rarely, wide complex tachycardia may occur in the setting of preexcited SVT because of antidromic AVRT or in cases of preexcited atrial fibrillation, atrial tachycardia, or AVNRT where the accessory pathway is not part of the reentrant circuit (ie, bystander accessory pathway participation). Irregularity during SVT occurs in cases of rapid atrial fibrillation, rapid atrial flutter with variable atrioventricular block, and multifocal atrial tachycardia. Note that atrial fibrillation in the setting of complete heart block with an escape rhythm may appear regular.
What is a supraventricular tachycardia?
Supraventricular tachycardia (SVT) is an arrhythmia initiated above the ventricles, at or above the atrioventricular (AV) node. This cardiac rhythm occurs due to improper electrical conduction within the heart that disrupts the coordination of heartbeats. Early beats occur within the atria of the heart due to improperly functioning electrical connections, resulting in a rapid heart rate such that the heart does not have enough time to fill the atria with blood before contraction of the atria. This can lead to the patient feeling dizziness or lightheadedness because the brain is not receiving adequate oxygen or blood. The onset of this dysrhythmia is typically sudden, and may be prompted by emotional or physical stress.
What should be done before cardioversion?
Before performing cardioversion, the healthcare provider should ensure the patient has IV access and equipment is at the ready for suctioning, intubation, and measuring oxygen saturation . Contingent on the severity of the patient’s symptoms and how hemodynamically unstable they may be, sedation medication should be administered before initiating cardioversion. If all elements are in place, synchronized cardioversion should then be conducted. Recommendations specific to the cardioverter being utilized should be followed when determining appropriate settings for energy levels during shock delivery. If the patient’s cardiac rhythm remains unchanged following cardioversion, the healthcare provider or team should re-evaluate any potential underlying causes contributing to the patient’s condition. The energy level should then be increased for the next attempt at cardioversion.
What Are ECG Characteristics of Supraventricular Tachycardia?
Typically characterized by having a narrow QRS complex that is less than or equal to 0.12 seconds. A wide QRS (greater than or equal to 0.12 seconds) can occur, but is less common.
Is 150 beats per minute considered a symptomatic tachycardia?
If a patient is experiencing symptomatic tachycardia with a heart rate of 150 beats per minute or more and is considered symptomatically and hemodynamically unstable, they are a candidate for cardioversion. However, patients may be symptomatic at heart rates less than 150 beats per minute, most notably if they have pre-existing cardiovascular disease or other potential risk factors or contributing causes as discussed above. Therefore, the healthcare provider must understand when cardioversion should be used, the medications indicated for cardioversion, how to properly prepare the patient for cardioversion, and how to utilize the cardioverter.
Should supraventricular tachycardia be transferred?
Patients experiencing supraventricular tachycardia should be transferred to a higher level of care for further evaluation and management.
How to stop SVT?
A person can terminate an episode in several ways such as bearing down, blowing in a syringe, immersing your face in cold water, performing a headstand, coughing or even gagging. Vagus nerve stimulation is one of the first-line treatment options for someone who wants to stop SVT at home. Performing Valsalva maneuver stimulates the vagus nerve and activates the parasympathetic nerves of the heart, which slows down the heart rate.
How long should you blow a syringe?
From a sitting position, you blow into a syringe as hard as you can for 10-15 seconds. Right after that, lay lie flat on your back and someone should lift your legs at 45 degrees and keep them in that position for another 15 seconds.
Can you cough for SVT?
Coughing can help in managing an SVT episode. However, you have to cough hard – the harder you can cough, the better your ability to manage an SVT episode . Coughing has a similar effect to the Valsalva maneuver. It increases the pressure in your chest and throat.
Is the Valsalva maneuver a good procedure?
It could be quite a disgust ing procedure (due to the vomit involved), but it works. Maybe that is why it is among the less popular methods as there are less gross methods which work better – such as the Valsalva maneuver.
Can you heal a SVT overnight?
You may already know that healing your SVT doesn’t happen overnight, so the first thing you have to learn is how to deal with an episode when it happens. The good news is you CAN convert out an SVT episode most of the time using different techniques. In the context of supraventricular tachycardia, the vagal maneuver is usually done ...

Diagnosis
Treatment
Lifestyle and Home Remedies
Alternative Medicine
Specialist to consult
Preparing For Your Appointment