Nutrition
You should:
- stay away from work, school or college until your TB treatment team advises you it's safe to return
- always cover your mouth – preferably with a disposable tissue – when coughing, sneezing or laughing
- carefully dispose of any used tissues in a sealed plastic bag
How long it will take to recover from TB?
You will need to have TB treatment for at least six months, to make sure all the TB bacteria are killed. If you have TB of the lungs or throat, after two weeks of treatment you should no longer be infectious. Gradually you will start to feel better. This may take weeks, but you will stop feeling sick and tired all the time.
How many months one should take treatment for tuberculosis?
Regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment). INTENSIVE PHASE. CONTINUATION PHASE. Regimen. Drugs a. Interval and Dose b. (minimum duration) Drugs. Interval and Dose b,c.
How long should the minimum TB patient be treated?
The treatment regimen is a lengthy one, but if you stick with it and take medications the way you should, you can beat the disease. Even with treatment, however, tuberculosis reinfection is becoming a problem. It's very common for people with tuberculosis to relapse during treatment.
Can TB return after treatment?

How long does treatment of tuberculosis take?
RIPE regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment).
Why TB treatment is so long?
A fundamental problem in the treatment of tuberculosis (TB) is the long duration of therapy required for cure. The recalcitrance of Mycobacterium tuberculosis (MTB) to eradication is thought to result from its achieving a nonreplicating (dormant) state in the host.
What is the minimum period of TB treatment?
Duration of treatment with the current first-line anti-TB drugs is a minimum of 6 months. Reducing the duration of the treatment from six to two months or less could result in significant increase of adherence to treatment and cost reduction.
Is 6 months TB treatment enough?
Conclusions: Cavitary tuberculosis is best treated with 6-mo regimens comprising daily IP and thrice-weekly CP, which may be extended when 2-mo culture is positive. Although extending treatment of 6-month regimens may reduce relapse of tuberculosis, the optimal approach for reducing relapse has not been determined.
How long does it take for a TB patient to recover?
After taking TB medicine for several weeks, a doctor will be able to tell TB patients when they are no longer able to spread TB germs to others. Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
Can you live a normal life with TB?
While tuberculosis (TB) is a highly contagious disease, it's also very treatable. The best way to avoid complications from the disease is to take medications regularly and complete the full course as prescribed. In the United States, people with TB can live a normal life, both during and after treatment.
Can TB be cured in 2 months?
Brief Summary: Tuberculosis (TB) is a serious infection that can affect the lungs and other parts of the body. The usual way to treat TB is to take 4 medicines by mouth every day for 2 months, then take 2 of the same medicines for 4 more months, for a total of 6 months.
What are the 3 stages of tuberculosis?
There are 3 stages of TB—exposure, latent, and active disease. A TB skin test or a TB blood test can diagnose the disease. Treatment exactly as recommended is necessary to cure the disease and prevent its spread to other people.
What is the fastest way to cure TB?
If you have an active TB disease you will probably be treated with a combination of antibacterial medications for a period of six to 12 months. The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol.
Can tuberculosis be fully cured?
Active, drug-sensitive TB disease is treated with a standard 6-month course of 4 antimicrobial drugs that are provided with information, supervision and support to the patient by a health worker or trained volunteer. The vast majority of TB cases can be cured when medicines are provided and taken properly.
What happens after TB is cured?
Once your course of treatment is finished, you may have tests to make sure you are clear of TB. You might need more treatment if tests show there is still TB bacteria in your body, but most people will get the all-clear. Your treatment will not be stopped until you are cured.
How do you know you are healed from TB?
Testing at 5 or 7 months will show if the patient has been cured of TB. It is a wonderful achievement when the patient completes the full course of medication but proof of cure must be obtained through the patient giving that final sputum.
How long do you have to take antibiotics for tuberculosis?
For active tuberculosis, you must take antibiotics for at least six to nine months. The exact drugs and length of treatment depend on your age, overall health, possible drug resistance and where the infection is in your body.
What is the test for TB?
Sputum tests. If your chest X-ray shows signs of tuberculosis, your doctor might take samples of your sputum — the mucus that comes up when you cough. The samples are tested for TB bacteria. Sputum samples can also be used to test for drug-resistant strains of TB.
How long does ethambutol last?
If you have drug-resistant TB, a combination of antibiotics called fluoroquinolones and injectable medications, such as amikacin or capreomycin (Capastat), are generally used for 20 to 30 months. Some types of TB are developing resistance to these medications as well.
What test is used to test for tuberculosis?
The most commonly used diagnostic tool for tuberculosis is a skin test, though blood tests are becoming more commonplace. A small amount of a substance called tuberculin is injected just ...
What test can confirm active tuberculosis?
Blood tests can confirm or rule out latent or active tuberculosis. These tests measure your immune system's reaction to TB bacteria.
Can a TB test be wrong?
Results can be wrong. The TB skin test isn't perfect. Sometimes, it suggests that people have TB when they don't. It can also indicate that people don't have TB when they do. You can have a false-positive result if you've been vaccinated recently with the bacille Calmette-Guerin (BCG) vaccine.
Can TB drugs cause liver damage?
Serious side effects of TB drugs aren't common but can be dangerous when they do occur. All tuberculosis medications can be toxic to your liver. When taking these medications, call your doctor immediately if you have any of the following:
Is TB a serious disease?
TB is a serious disease, and can be fatal if not treated properly. It is important to remember that all medications have risks and benefits. Learn more from CDC’s Dear Colleague letter. Not everyone infected with TB bacteria becomes sick. As a result, two TB-related conditions exist: latent TB infection and TB disease.
Can latent TB be fatal?
Without treatment latent TB infection can progress to TB disease. If not treated properly, TB disease can be fatal.
Can rifampin be used for TB?
Treatment. impurities in rifampin and rifapentine, two important anti-tuberculosis (TB) medications. People with TB disease or latent TB infection taking rifampin or rifapentine should continue taking their current medication, and should talk with their healthcare provider about any concerns.
What should a clinic decide on TB treatment?
Clinicians should choose the appropriate treatment regimen based on drug susceptibility results of the presumed source case (if known), coexisting medical conditions (e.g., HIV. ), and potential for drug-drug interactions. Consultation with a TB expert is advised if the known source of TB infection has drug-resistant TB.
What is the name of the drug that is used to treat TB?
Isoniazid (INH) Rifapentine (RPT) Rifampin (RIF) These medications are used on their own or in combination, as shown in the table below. CDC and the National Tuberculosis Controllers Association (NTCA) preferentially recommend short-course, rifamycin-based, 3- or 4-month latent TB infection treatment regimens over 6- or 9-month isoniazid ...
Is 6H a good treatment for TB?
If short-course treatment regimens are not a feasible or an available option, 6H and 9H are alternative, effective latent TB infection treatment regimens. Although effective, 6H and 9H have higher toxicity risk and lower treatment completion rates than most short-term treatment regimens.
How long does it take to cure TB?
Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
How many people with LTBI will develop TB?
While not everyone with LTBI will develop TB disease, about 5–10% will develop TB disease over their lifetimes if not treated. Progression from untreated LTBI to TB disease is estimated to account for approximately 80% of U.S. TB cases. Some people who have LTBI are more likely to develop TB disease than others.
What does a negative TB test mean?
A negative TB blood test means that your blood did not react to the test and that you likely do not have TB infection. TB blood tests are the recommended TB test for: People who have received the bacille Calmette–Guérin (BCG) TB vaccine.
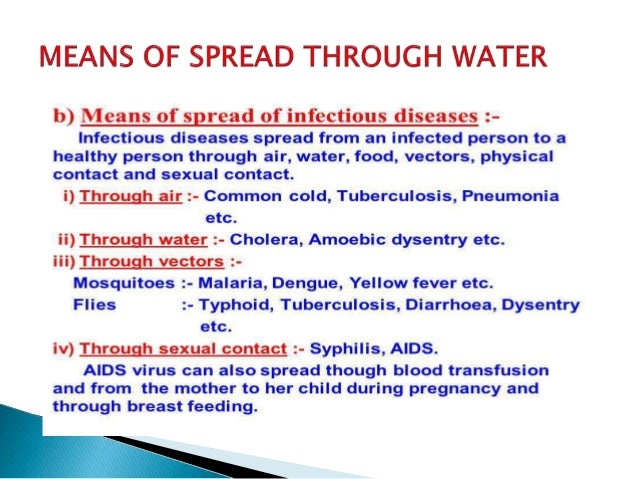
How does TB spread?
The TB germs are spread into the air when a person with infectious TB disease of the lungs or throat coughs, speaks, or sings. People nearby may breathe in these TB germs and become infected. When a person breathes in TB germs, the TB germs can settle in the lungs and begin to grow.
What is the cause of TB?
Tuberculosis (TB) is caused by bacteria called Mycobacterium tuberculosis (M. tuberculosis). The bacteria, or germ, usually attack the lungs. TB germs can attack any part of the body, such as the kidney, spine, or brain. There is good news. People with TB can be treated if they seek medical help.
What does it mean when you have a positive TB test?
May feel sick and may have symptoms such as a cough, fever, and/or weight loss. Usually has a positive TB skin test or TB blood test indicating TB infection. Usually has a positive TB skin test or TB blood test indicating TB infection. Has a normal chest x-ray and a negative sputum smear.
Where are people born with TB?
You were born in or frequently travel to countries where TB disease is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, and Guatemala, and other countries where TB is common.
How long does it take to treat TB?
The treatment for this type of TB takes much longer, 20 to 30 months to complete, and you may experience more side effects.
What is the best treatment for TB?
The most common treatment for active TB is isoniazid INH in combination with three other drugs—rifampin, pyrazinamide and ethambutol. You may begin to feel better only a few weeks after starting to take the drugs but treating TB takes much longer than other bacterial infections.
What are the side effects of TB?
While you are in treatment for active TB disease, you will need regular checkups to make sure your treatment is working. Everyone is different, but there are side effects associated with taking the medications, including: 1 Upset stomach, nausea and vomiting or loss of appetite 2 Tingling or numbness in the hands or feet 3 Itchy skin, rashes or bruising 4 Changes in your eyesight or blurred visions 5 Yellowish skin or eyes 6 Dark-colored urine 7 Weakness, fatigue or fever that for three or more days
What are the symptoms of TB?
Yellowish skin or eyes. Dark-colored urine. Weakness, fatigue or fever that for three or more days. It is important to tell your doctor or TB nurse immediately if you begin having any unusual symptoms while taking medicine for either preventive therapy or for active TB disease.
What to take for TB tingling?
If you are having trouble with tingling and numbness, your doctor may prescribe a vitamin B6 supplement while you are in treatment. It may also be possible to change TB medications if your side effects are serious.
Can you get TB from taking too much medicine?
You must finish your medicine and take the drugs exactly as prescribed. If you stop taking the drugs too soon you can become sick again and potentially spread the disease to others. Additionally, by taking the drugs incorrectly, TB germs that are still alive may become drug-resistant, making it harder for you to get better next time.
Do you need regular checkups for TB?
While you are in treatment for active TB disease, you will need regular checkups to make sure your treatment is working. Everyone is different, but there are side effects associated with taking the medications, including:
How long does it take to cure MTB?
Treatment of MTB with isoniazid (INH), a drug that targets cell wall synthesis, causes a 3-log reduction in broth culture in two hours [9,10], whereas more than 14 days of therapy are required to achieve a 3-log reduction in viable bacterial counts in the sputum during active TB [11,12] and several months of treatment are required to eradicate latent TB (Table 1). The role of pyrazinamide in shortening TB therapy to six months may also suggest the existence of a nonreplicating population in vivo, as, unlike other anti-TB drugs, pyrazinamide is more active against nonreplicating than actively replicating MTB in vitro [13,14]. Phenotypic antibiotic resistance likely accounts for the need for longer antibiotic therapy in many bacterial infections, presenting a universal obstacle to the treatment of infectious diseases ([15–17] and Table 1).
Why is TB a fundamental problem?
A fundamental problem in the treatment of tuberculosis (TB) is the long duration of therapy required for cure. The recalcitrance of Mycobacterium tuberculosis(MTB) to eradication is thought to result from its achieving a nonreplicating (dormant) state in the host. Because virtually all classes of antibiotics require bacterial replication for their action, the nonreplicating state is thought to render MTB phenotypically resistant to otherwise bactericidal antibiotics.
What is the nonreplicating state of tuberculosis?
tuberculosisin the host, that renders the bacteria phenotypically resistant to killing by both host immune mechanisms and antibiotics.
How does drug resistance affect TB?
In the absence of an effective vaccine, TB eradication is dependent on curing infected individuals who are either contagious or may become contagious after reactivation of latent infection. The relative lack of protective immunity provided by natural infection makes control all the more dependent on complete bacterial eradication from the population, since individuals who are cured of TB remain vulnerable to reinfection [18,19]. Drug resistance, and the consequent need for long-term multidrug therapy have stymied TB eradication efforts particularly in poor countries with the highest disease burden. Poor adherence to therapy also has led to an alarming increase in multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains [20], which are associated with high morbidity and mortality [21,22]. Hence the critical need for new drugs to shorten treatment of drug-sensitive TB, and to treat MDR- and XDR-TB.
Why is multidrug therapy needed?
MTB can exhibit genetic resistance that is heritable and fixed, as well as phenotypic, reversible resistance to administered antibiotics. The presence of genetic drug resistance in some or all of the infecting bacteria dictates the need for multidrug therapy [2,4]. The greater the bacterial burden, the more likely that it contains genetically resistant mutants [5]. Therapy failure due to genetic resistance is related to the frequency of preexisting resistant mutants and their enrichment by selective pressures imposed by inadequate therapy [4]. Simultaneous use of multiple anti-TB drugs makes it less likely that a mutant resistant to a single agent will survive.
Is streptomycin effective for TB?
Soon after the discovery of streptomycin it became clear that while many patients with TB treated with this drug initially improved dramatically, most developed streptomycin-resistant strains so that there was little improvement in mortality over untreated patients [1]. The development of new antibiotics led to the realization that there were two requisites for effective cure: treatment with multiple antibiotics and long therapy [2]. Indeed, the minimum length of treatment and number of drugs required for cure has been more carefully tested for TB than for most infectious diseases (see [3] and Table S1).
When should latent TB be treated?
Treatment of latent TB infection should start after excluding the possibility of TB disease.
How many people have latent TB?
In the United States, up to 13 million people may have latent TB infection. Without treatment, on average 1 in 10 people with latent TB infection will get sick with TB disease in the future. The risk is higher for people with HIV, diabetes, or other conditions that affect the immune system.
Why is latent TB important?
Treatment of latent TB infection is essential to controlling TB in the United States because it substantially reduces the risk that latent TB infection will progress to TB disease.
Can TB be treated with LTBI?
Persons with no known risk factors for TB may be considered for treatment of LTBI if they have either a positive IGRA result or if their reaction to the TST is 15 mm or larger. However, targeted TB testing programs should only be conducted among high-risk groups.
Which countries have TB?
From countries where TB is common, including Mexico, the Philippines, Vietnam, India, China, Haiti, and Guatemala, or other countries with high rates of TB. (Of note, people born in Canada, Australia, New Zealand, or Western and Northern European countries are not considered at high risk for TB infection, unless they spent time in a country with a high rate of TB.)
Can TB spread to others?
People with latent TB infection do not have symptoms, and they cannot spread TB bacteria to others. However, if latent TB bacteria become active in the body and multiply, the person will go from having latent TB infection to being sick with TB disease.