
How long does it take for lymphedema to develop?
The onset of the patient's swelling is ascertained because it is an important factor in the diagnosis of lymphedema. Primary lymphedema almost always affects the pediatric population, adult-onset is uncommon. Boys are more likely to present in infancy, while girls commonly develop the disease during adolescence. 2Secondary lymphedema following lymphadenectomy and/or radiation typically begins 12 to 18 months following the injury to lymph vessels. Three-fourths of patients develop swelling within 3 years after the injury and the risk of lymphedema is 1% each year thereafter. 8Edema that forms immediately following an injury to an extremity is not consistent with lymphedema.
What is the most sensitive sign of lymphedema?
A fairly sensitive and specific sign for lymphedema is the Stemmer sign. 14If the examiner is unable to pinch the skin on the dorsum of the hand or foot (positive Stemmer sign), it is likely the patient has lymphedema. Swelling, inflammation, and adipose deposition cause the skin to thicken, which reduces the ability to lift and pinch the integument of the distal extremity. The Stemmer sign is more sensitive than specific. If the test is positive, it is likely the patient has lymphedema. However, if the examination is negative, the patient may still have lymphedema depending on the severity of their condition and the length of time they have had the disease.
Is lymphedema a generalized condition?
If a patient complains of swelling outside of the limbs or genitalia, lymphedema likely is not the cause. However, primary generalized lymphedema (including the face and trunk) can occur rarely. Primary lymphedema affects the lower extremities in 92% of cases, and 50% have bilateral disease. 2Sixteen percent of children with idiopathic lymphedema have upper extremity disease. 2
Is lymphedema a musculoskeletal condition?
Lymphedema typically is painless; if a patient complains of significant pain, it is unlikely he/she has the condition. As the size of the extremity enlarges, however, secondary musculoskeletal discom fort can occur. A markedly enlarged lower extremity can inhibit ambulation. Lymphatic vesicles may bleed or leak lymph fluid (lymphorrhea). Cutaneous ulceration is not typical for lymphedema and should suggest an alternate diagnosis (e.g., venous insufficiency).
Does lymphedema improve or worsen?
56Lymphedema is a chronic condition that does not improve and slowly worsens . Lymphedema progresses through four stages. 7Stage 0 indicates a normal extremity clinically, but with abnormal lymph transport (i.e., illustrated by lymphoscintigraphy). Stage 1 is early edema, which improves with limb elevation. Stage 2 represents pitting edema that does not resolve with elevation. Stage 3 describes fibroadipose deposition and skin changes. 7
Can lymphedema be diagnosed with enlargement?
Lymphedema often is confused with other causes of extremity edema and enlargement. Understanding the risk factors and physical examination signs of lymphedema can enable the health care practitioner to accurately diagnose patients ∼90% of the time. Confirmatory diagnosis of the disease is made using lymphoscintigraphy. It is important to correctly diagnose patients with lymphedema so that they can be managed appropriately.
Can lymphedema be diagnosed by histopathology?
These tests are not sensitive or specific for lymphedema and only may show skin thickening or subcutaneous edema. Lymphedema cannot be diagnosed by histopathology; biopsy specimens may show non-specific skin and adipose inflammation.
How to treat lymphedema?
Treatment focuses on reducing the swelling and controlling the pain. Lymphedema treatments include: Exercises. Light exercises in which you move your affected limb may encourage lymph fluid drainage and help prepare you for everyday tasks, such as carrying groceries.
How to reduce the risk of complications from lymphedema?
To reduce the risk of complications from lymphedema, avoid injuring the affected limb. Cuts, scrapes and burns can invite infection. Protect yourself from sharp objects . For example, shave with an electric razor, wear gloves when you garden or cook, and use a thimble when you sew.
How to help lymphedema in arm?
A certified lymphedema therapist can teach you exercises that may help. Wrapping your arm or leg. Bandaging your entire limb encourages lymph fluid to flow back toward the trunk of your body.
How to treat swollen limbs?
The swelling from lymphedema might dull pain from an injury or burn, so don't use heating pads on the affected limb. Moisturize your skin daily.
How to find obstructions in lymphatic system?
Ultrasound can help find obstructions. Radionuclide imaging of your lymphatic system (lymphoscintigraphy). During this test you're injected with a radioactive dye and then scanned by a machine. The resulting images show the dye moving through your lymph vessels, highlighting blockages.
What tests can be done to check lymphedema?
If the cause of your lymphedema isn't as obvious, your doctor may order imaging tests to get a look at your lymph system. Tests may include: MRI scan. Using a magnetic field and radio waves, an MRI produces 3-D, high-resolution images. CT scan.
What is the best way to see lymphatic blockages?
CT scan. This X-ray technique produces detailed, cross-sectional images of the body's structures. CT scans can reveal blockages in the lymphatic system.
How long does lymphedema treatment last?
Lymphedema treatment with CDT lasts anywhere from two weeks to three months, depending on severity and how the body responds to the treatment.
How long do you have to wrap your body for lymphatic drainage?
Affected body parts usually need to stay wrapped up 24 hours a day — except during bathing.
What is primary lymphedema?
Primary lymphedema is lymphedema that happens on its own, not caused by another condition or injury. It can occur in children born with impaired or missing lymph nodes. Globally, a common cause of lymphedema is an infection by Wuchereria bancrofti roundworms. This is known as lymphatic filariasis.
What is lymphatic drainage?
Manual lymphatic drainage, which is targeted massage or manipulation of soft tissue, can aid in draining lymphatic fluid. Your CDT provider will likely massage you and also show you some techniques that you can perform on yourself to promote drainage.
What is the difference between primary and secondary lymphedema?
For example, up to 40 percent of those who undergo surgery for breast cancer will experience it, as this surgery usually involves a sentinel lymph node biopsy. This type of lymphedema is called secondary lymphedema. Primary lymphedema is lymphedema that happens on its own, not caused by another condition or injury.
How many people have lymphedema?
According to the World Health Organization. Trusted Source. , it’s responsible for causing lymphedema in over 15 million people worldwide. Lymphatic filariasis is one of the world’s leading causes of disability. Trusted Source. . No matter the origin, everyone with lymphedema experiences pain and discomfort.
Is there a cure for lymphedema?
Outlook for lymphedema therapy. Although there is no cure for lymphedema, the condition can be managed to reduce discomfort. Depending on the nature of your lymphedema, your doctor may begin with a treatment such as wrapping, and then move on to physical therapy. Some people see benefits from ongoing physical therapy alone.
How many stages of lymphedema are there?
Lymphedema tends to progress in the absence of treatments, but the rate of progression can vary dramatically. There are four stages that are marked by tissue characteristics observable during physical exam.
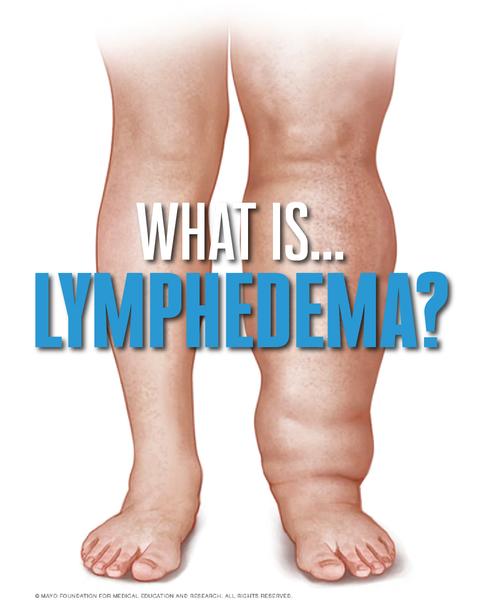
What is lymphedema in the lymphatic system?
Lymphedema: Diagnosis and treatment. Lymphedema is an abnormal accumulation of protein-rich fluid due to mechanical insufficiency of the lymphatic system. The veins and lymph vessels are both charged with removing liquid and solid debris from tissue. The veins remove most of the fluid, from 90 to 95 percent, and some small protein molecules such as ...
What is CDT treatment?
CDT is still considered the international standard of care for lymphedema treatment and consists of two phases: reductive and maintenance. CDT strives to increase lymph drainage; to decrease swelling, discomfort, fibrosis and risk of cellulitis; and to improve functional status and quality of life. The reductive phase includes the use of a massage technique known as manual lymphatic draining (MLD), short stretch bandaging, exercises to create and augment an internal pumping mechanism, skin care and education in self-management. Skin care is necessary to prevent infection and includes controlling bacterial and fungal colonization, eliminating microbial overgrowth in skin crevices, and hydrating the skin to control dryness and fissuring.
What is the effect of collagen matrix on lymphatic outflow?
The accumulation of a disorganized collagen matrix is exogenously compressive and disrupts lymphatic outflow tracts , leading to progressive over-dilation of lymph vessels, one-way valve incompetence and retrograde flow.
What is the function of the lymphatic system?
The lymphatic system moves some fluid, but its primary job is to remove solid macromolecular debris from the tissue — large molecules, including long-chain fatty acids and large proteins.
What do you use for maintenance phase?
During the maintenance phase practitioners use batting and foam in a number of different ways to distribute the compression. "We are not squeezing the fluid out of the affected tissue," explains Dr. Cheville. "We create a soft cast with bandages, and within that we try to create a pumping mechanism with exercises. One thing we often miss as we treat lymphedema in this country — we don't put enough emphasis on the critical role of exercise."
What is stage 3 of lymphostatic elephantiasis?
Stage 3 (lymphostatic elephantiasis): This stage is marked by the presence of dermal metaplasia. Some of the proteins present are pro-inflammatory and can lead to skin changes. Typically, these skin changes include dermal keratinization (thickening) and papilloma formation.
Stage 0 (Latent Stage)
No swelling or changes to the body can be seen, but you may feel a mild tingling or slight tightness or heaviness to the skin. Stage 0 may last for months or even years before more obvious symptoms develop.
Stage 1 (Mild Stage)
The arm, leg, hand, foot, or other area looks slightly swollen as lymph fluid builds up. Pressing the skin will cause a temporary dent (or pit) to form. Elevating the affected limb can help to reduce the swelling, and wearing compression garments will help keep fluid from pooling.
Stage 2 (Moderate Stage)
Elevating the limb alone no longer helps to reduce the swelling, and it continues to worsen. Pressing on the skin doesn’t leave a pit, as the skin thickens and hardens. The swelling is managed with the daily wearing of compression garments, both during the day and at night.
Stage 3 (Severe Stage)
The affected limb becomes large and misshapen, and the hardened skin takes on a leathery, wrinkled appearance. Lymph fluid may leak from breaks or folds in the skin and should be kept clean and dry to avoid infection. Special or customized compression garments and pumps can still help to manage symptoms.
What is the treatment for lymphedema?
A treatment for lymphedema is complete decongestive therapy (CDT).
How to get rid of lymphedema?
Exercises: With compression, special exercises will help to pump lymph out of the swollen area. Skin Care: Keeping the skin clean and moisturized will help prevent infections that often can happen with lymphedema. Self-Care Management and Training: Learning how to manage your lymphedema at home.
Why does lymphedema occur?
Lymphedema occurs as a result of damage to the lymph nodes or lymph vessels. The lymph vessels run very close to the blood vessels in our bodies and move fluid from the body through the lymph nodes and then into the blood. Lymph nodes work as filters to fight infection and help regulate swelling.
How to treat lymphatic drainage?
How long does treatment last? 1 In order to prevent the area from swelling constant attention is needed. 2 Elastic compression garments that fit like a second skin are worn during the day. 3 Often bandages with foam are worn at night to decrease daily daytime swelling. 4 Exercises are done while wearing compression. 5 Self manual lymphatic drainage is done for 20 minutes per day.
Why do lymph nodes work?
Lymph nodes work as filters to fight infection and help regulate swelling. Lymphedema is chronic swelling that happens when the lymph is not moving properly. This can happen when lymph nodes are removed due to cancer. Lymph nodes can also be removed in other non-cancer surgeries.
How long does it take for a decongestive to work?
The number of weeks depends on the amount of swelling and tissue firmness. Complete decongestive therapy for one-hour sessions, 4 to 5 days per week. Bandages with foam are worn about 23 hours per day and often only removed to bathe.
Why does lymphedema cause swelling?
Lymphedema results in chronic swelling that leads to tissue inflammation and scarring. The swollen body part feels harder to touch and is heavier than the non-swollen side.
How long does it take for lymphedema to progress?
Primary lymphedema usually doesn’t progress and is stable after few years of being active. Those patients who suffer from lymphedema for more than 10 years have a 10% chance of developing lymphangiosarcoma, which is the most fatal complication of this disease with a prognosis of a few months to 2 years.
What is the treatment for lymphedema?
Other possible treatments include lymphatic vessel grafting where lymph vessels can be used as grafts and low-level laser therapy where lasers are used to treat the lymphedema and there are still some studies being done on procedures to help better quality of life.
How to treat lymphendema?
If the lymphendema is treated well and with the proper treatment such as complete decongestive therapy that includes manual manipulation of the lymphatic ducts with massage, applying short-stretched compression bandages, therapeutic exercises and proper skin care, then the life expectancy is with good prognosis.
What causes lymphedema in the lymphatic system?
Primary lymphedema is caused by developmental lymphatic vascular anomalies and secondary lymphedema is caused by an underlying disease, trauma or surgery. The most frequent cause is the secondary type that is a result from insufficient ...
What is lymphedema in the subcutaneous?
Lymphedema is a condition which is characterized by localized swelling and protein-filled fluid retention in the subcutaneous tissues. It is caused by a compromised lymphatic system.
What happens when lymphatic fluids cannot be transported?
When the lymphatic fluids cannot be transported by the lymphatic system, the pressure in the lymphatic vessels gradually increases and the transportation slows down significantly. When the pressure becomes too much for the walls of the lymphatic vessels, they eventually leak the fluid into the surrounding tissues causing lymphedema.
What is the rarest cancer that can develop in a person with long standing lymphedema?
In some rare cases of long-standing lymphedema, it can develop into a rare form of cancer called lymphangiosarcoma which has a poor life expectancy.
What is the goal of lymphedema?
Once lymphedema is diagnosed, the goal is to delay or even prevent the progression of the disease.
Does elevation of the limb reduce swelling?
Limb elevation alone rarely reduces swelling and pitting may or may not occur as tissue fibrosis develops.
Is lymphedema a progressive disease?
Lymphedema is a progressive disease and develops in stages which can be categorized according to severity.
How long does lymphedema last?
How long lymphedema lasts depends on what is causing it and how much your lymphatic system is damaged. Mild lymphedema may get better with treatment in a week. Sometimes the lymph ducts have been damaged to the point that even with treatment the lymphedema never completely goes away.
How long does it take for lymphedema to go away after surgery?
Temporary lymphedema is quite common immediately after surgery. It is usually mild, and goes away within a few weeks or months. It is difficult to predict which women will develop lymphedema and whether it will get worse later on or become permanent.
How long does decongestive therapy last?
Complete decongestive therapy for one-hour sessions, 4 to 5 days per week. Bandages with foam are worn about 23 hours per day and often only removed to bathe.
Can lymphedema go away?
For others, the condition does worsen. The later stages of lymphedema often can't be completely reversed because the tissue under the skin has been damaged.
Diagnosis
- If you're at risk of lymphedema — for instance, if you've recently had cancer surgery involving your lymph nodes — your doctor may diagnose lymphedema based on your signs and symptoms. If the cause of your lymphedema isn't as obvious, your doctor may order imaging tests to get a look at your lymph system. Tests may include: 1. MRI scan.Using a magn...
Treatment
- There's no cure for lymphedema. Treatment focuses on reducing the swelling and preventing complications.
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- To reduce the risk of complications from lymphedema, avoid injuring the affected limb. Cuts, scrapes and burns can invite infection. Protect yourself from sharp objects. For example, shave with an electric razor, wear gloves when you garden or cook, and use a thimble when you sew.
Coping and Support
- It can be frustrating to know there's no cure for lymphedema. However, you can control some aspects of lymphedema. To help you cope, try to: 1. Find out all you can about lymphedema.Knowing what lymphedema is and what causes it can help communication with the doctor or physical therapist. 2. Take care of the affected limb.Clean your skin daily, looking over …