Healthline.com
· Draining is sometimes the treatment for a large, symptomatic pancreatic cyst, particularly in older patients who may not be physically healthy enough for surgery. This is typically done by running an endoscope, which is a flexible tube that can be equipped with a needle for draining, into the mouth and down to the abdomen. There, the needle will be …
Trueremedies.com
How are pancreatic cysts and pseudocysts treated? Most pseudocysts resolve on their own without treatment, over time. However, when symptoms become persistent, complications emerge or a cyst become larger than 6 centimeters in size, it should be drained. There are three methods of cyst drainage: Endoscopic drainage.
Homeremedyshop.com
· In fact, larger and more recent studies estimate a morbidity of 30–46% and a mortality of 4% following pancreatic surgery. 13,73,74 In recent years, there have been emerging data for EUS-guided pancreatic cyst ablation (in the form of injection of ethanol or antitumor agents or through radiofrequency ablation) in patients unable or unwilling to undergo surgery.
How does one get rid of pancreatic cysts?
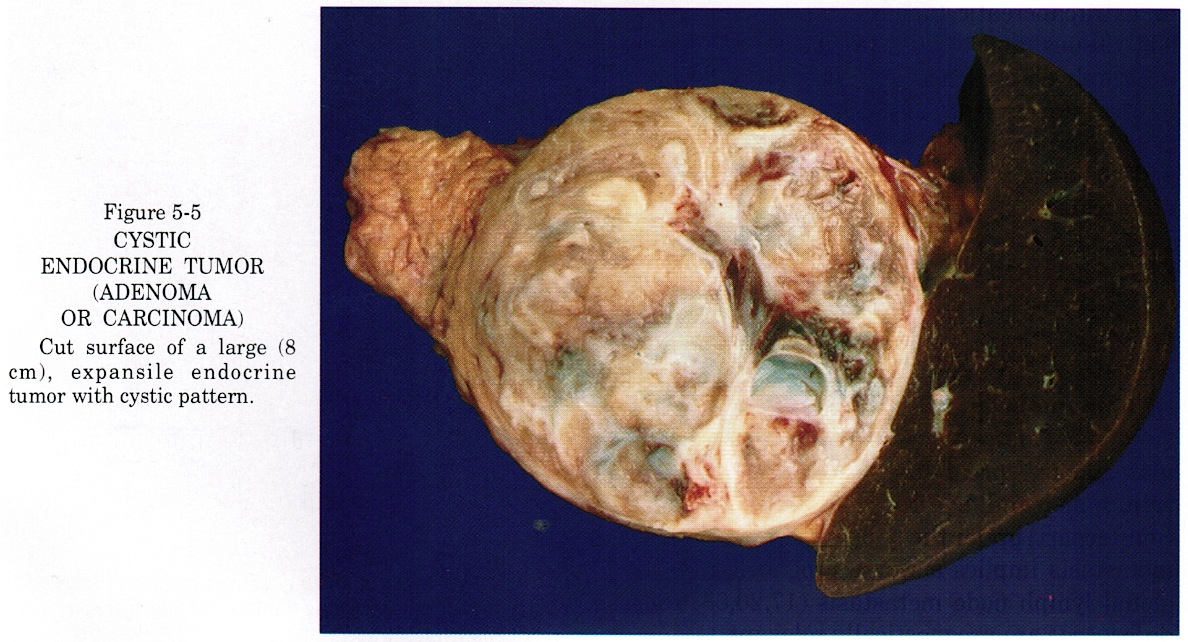
· Specimen of resection leading to splenectomy due to infiltration of the splenic vein by the cystic mass. Cysts located in the head of the pancreas are resected with standard or pylorus-preserving...
How do you drain a pancreatic cyst?
· In a Whipple Procedure, Del Chiaro removed half of Page’s pancreas; the distal bile duct, which runs through the pancreas into the small intestine; the gallbladder; and the first part of the small intestine. He then reconnected the remaining pancreas to Page’s digestive organs.
Is surgery necessary for cysts in pancreas?
Small (<4 cm) pseudocysts in the head and the uncinate process of the pancreas are eligible for pseudocystoduodenostomy and pseudocystojejunostomy can be performed for all other cysts including extremely large (>15 cm) cysts 3,42. There is controversy as to whether pseudocystogastrostomy and pseudocystoduodenostomy are equivalent in their outcome: …
What is the treatment for a cyst on the pancreas?

What is considered a large pancreatic cyst?
Worrisome features are defined as a cyst larger than 3 cm, a thick cyst wall or one that “lights up” with contrast when a CT scan is done, size of the main duct of the pancreas measuring 5 to 9 mm, a nodule on the wall of the cyst that does not light up with CT contrast, or a sudden change in the diameter of the ...
How is a pancreatic cyst treated?
How are pancreatic cysts and pseudocysts treated?Endoscopic drainage.Percutaneous catheter drainage, which uses hollow tube inserted into the body to remove fluid.Surgical drainage, either via open surgery or laparoscopic surgery (using a laparoscope, a surgical tool that only requires a small incision).
At what size should a pancreatic cyst be removed?
Guidelines set in 2012 by the International Cancer of the Pancreas Screening Consortium call for surgical removal of these cysts when there are one or more and when dilation of the duct is at or greater than 10 millimeters.
Can pancreatic cyst be treated without surgery?
Pancreatic cysts and pseudocysts had to be treated by surgery until 15 years ago. Nowadays they can be aspirated (or drained) either endoscopically or by ultrasonic and computed tomographic guided punctures.
Should I be worried about a pancreatic cyst?
Pancreatic cysts are a condition you should take very seriously. Some common types of cysts in the pancreas can become cancerous, and for this reason even some cysts that are benign are still treated as precancerous since the likelihood they will become cancerous later is so high.
How long is recovery from pancreatic surgery?
As with all major operations, recovering from pancreatic surgery takes time. Full recovery requires an average of two months.
How serious is pancreatic surgery?
It carries a relatively high risk of complications that can be life threatening. When the operation is done in small hospitals or by doctors with less experience, as many as 15% of patients may die as a result of surgical complications.
How quickly do pancreatic cysts grow?
For cysts that increased in size, the median growth rate was 2.3 mm per year ( IQR , 1.5–4.4 mm/year), with a median overall increase of 4.8 mm ( IQR , 3.4–7.9 mm) in the largest dimension during the study period.
How long can you live with pancreatic cysts?
RESULTS. In total, 64 patients were identified as having neoplastic pancreatic cysts from 1994 to 2003 at the five institutions. The median overall patient survival time was 86 months. The median age at diagnosis for the patient population was 73 years, with 40 patients being women.
How long does it take for a pancreatic cyst to become cancerous?
After the first cancer cell appears, it takes an average of nearly seven years for that cell to turn into the billions that make up a cancerous tumor the size of a plum, after which at least one of the cells within the tumor has the potential and ability to spread to other organs.
Are pancreatic cysts curable?
In medical centers experienced in performing pancreatic surgery, surgical removal of precancerous or cancerous cysts results in a high rate of cure. Very small cysts can be followed to detect an increase in size that may indicate cancer or an increased risk of developing cancer.
What doctor treats pancreatic cysts?
Gastroenterologists (digestive health physicians) who specialize in medically treating all kinds of pancreatic diseases, including cysts. Interventional gastroenterologists who specialize in nonsurgical approaches to diagnosing pancreatic cysts and other problems.
What is the best treatment for a pancreatic cyst?
In some cases, drainage through a needle in your skin may be the only viable option. Pancreatic cyst surgery. This surgical option is primarily used for enlarged, painful, or cancerous pancreatic cysts. There are several steps you can take to prevent a pancreatic cyst from occurring again, including:
What is a cyst in the pancreas?
What is a pancreatic cyst? The pancreas is a large organ behind the stomach that’s a crucial component of the digestive process. It creates hormones, like insulin, to help control blood sugar, as well as enzymes that help break down food in the small intestine. Pancreatic cysts are pockets of fluid that are on — or in — your pancreas.
What causes pancreatitis after gallstones?
Hypertriglyceridemia is the third most common cause. Trusted Source. for acute pancreatitis after gallstones and alcohol. Hypertriglyceridemia can be genetic (primary) or due to other causes (secondary) such as diabetes, medications, alcohol, or pregnancy.
Can alcohol cause pancreatic cysts?
Gallstones and heavy alcohol use. These are both risk factors for pancreatitis, so in turn, they’re risk factors for pancreatic cysts.
How to treat cysts in the small intestine?
The more invasive treatment options include: Drainage. In this procedure, an endoscope (small tube) is placed in your mouth and directed to your small intestine. The small tube contains an endoscopic ultrasound, along with a needle to drain fluid from the cyst.
Can pancreatic cysts be treated?
There are few noninvasive treatments for pancreatic cysts, with the only real option being watchful waiting. This is because a benign cyst, even a large one, does not need any type of treatment as long as it does not bother you. However, you should still watch closely for any signs or symptoms that arise.
Is a pancreatic cyst benign?
The majority of pancreatic cysts are noncancerous (benign), however, there are several mucinous cysts that can be more concerning. This includes: Mucinous cystic neoplasm (MCN) are mainly found in women and contain ovarian tissue.
How to treat pancreatic cysts?
If they do not clear up without treatment, a doctor should monitor them to see if they continue to grow or show any signs of turning cancerous, in which case a biopsy may be needed. Large cysts, or ones that grow larger over time and which cause issues for the patient, may need to be drained with a needle. They may also require surgical removal, particularly if there are signs that they might turn to cancer.
What is the best way to drain a cyst from the pancreas?
An endoscope may be used to drain symptomatic pancreatic cysts.
How to know if a cyst is cancerous?
Removing a sample of the tissue and examining it under a microscope is the best way to ensure a cyst isn't cancerous.
Can pancreatic cysts be treated?
A pancreatic cyst that persists after a normal period of watchful waiting may still not require treatment, but typically requires monitoring. Cysts in the pancreas can grow over time, and once they get bigger than 2 centimeters they can cause back or abdominal pain, jaundice, or even become infected. They may also turn pre-cancerous or cancerous. Ongoing cysts should be checked regularly by a doctor to ensure they are not causing a problem.
How long does it take for a pancreatic cyst to go away?
Often, a benign cyst will resolve within six weeks and no intervention is required.
Can pancreas problems be detected?
Problems with the pancreas may be detected via ultrasound.
Is a pancreatic cyst benign?
For the most part, serous cysts tend to be benign (non-cancerous). Most of the mucinous cysts are benign as well ...
Can MRI be used for cyst characterization?
Otherwise, MRI can be especially useful for further characterization. If potentially concerning features are detected on imaging studies or if there remains significant uncertainty related to the nature of the cyst, additional information can be gained by an endoscopic ultrasound.
Is pancreas surgery curative?
At present, the only curative treatment is surgery. As any surgery on the pancreas is a major undertaking. Therefore, it is best to reserve resection for cases in which there is a significant concern for cancer. This represents a minority of cases. In the vast majority of cases, surveillance with periodic imaging tests is all that is needed.
What is a cyst in the pancreas?
The pancreas is a large organ behind the stomach that produces hormones and enzymes that help digest food. Pancreatic cysts are typically found during imaging testing for another problem.
What is the condition that causes a cyst in the pancreas?
Some cysts are associated with rare illnesses, including polycystic kidney disease or von Hippel-Lindau disease, a genetic disorder that can affect the pancreas and other organs. Pseudocysts often follow a bout of a painful condition in which digestive enzymes become prematurely active and irritate the pancreas (pancreatitis).
What are the two types of pancreatic cysts?
The main categories of pancreatic cysts can be divided into two groups, nonneoplastic or neoplastic cysts. Each group includes many different subtypes of cysts, such as pseudocysts, serous cystadenomas and mucinous cystic neoplasms. Most aren't cancerous, and many don't cause symptoms.
Can a ruptured pancreatic cyst cause abdominal pain?
Rarely, cysts can become infected. See a doctor if you have a fever and persistent abdominal pain. A ruptured pancreatic cyst can be a medical emergency, but fortunately is rare. A ruptured cyst can also cause infection of the abdominal cavity (peritonitis).
What is a cyst in the pancreas?
A pancreatic cyst is a closed sac lined with epithelium and located on or in your pancreas (see below). Pancreatic cysts contain fluid. They can range from benign pseudocysts to malignant cysts (cancerous and spreading). There are several different types of pancreatic cysts.
What are the symptoms of a pancreatic cyst?
Pancreatic cysts and pseudocysts are growths in the pancreas. Symptoms may include nausea, abdominal bloating and pain. Cysts and pseudocysts should be treated to avoid complications such as rupture or infection.
What is the term for inflammation of the pancreas?
An inflammation of the pancreas is called pancreatitis . Pancreatitis can either be acute (a sudden, sharp, and/or severe attack) or chronic (recurring and/or lasting for a long period of time). When the pancreas is inflamed, digestive enzymes become activated while still inside the pancreas, which can cause the pancreas to begin "digesting" its own tissues.
Where is the pancreas located?
Your pancreas is a 6-inch gland located below your liver, between your stomach and your spine. The pancreas is made up of three parts: a "head" that is tucked into the duodenum (the upper part of the small intestine); a flattened, longer "body;" and a "tail" that is connected to the spleen.
How to drain cysts?
There are three methods of cyst drainage: Endoscopic drainage. Percutaneous catheter drainage, which uses hollow tube inserted into the body to remove fluid. Surgical drainage, either via open surgery or laparoscopic surgery (using a laparoscope, a surgical tool that only requires a small incision).
How big is a pseudocyst?
However, when symptoms become persistent, complications emerge or a cyst become larger than 6 centimeters in size, it should be drained. There are three methods of cyst drainage: Endoscopic drainage.
How long does it take for a pancreatic cyst to show symptoms?
Symptoms may occur within days to months following a pancreatitis attack. The most common symptoms include: Severe, persistent pain in the abdomen and sometimes the back. Nausea.
How are pancreatic cysts diagnosed?
Pancreatic cystic lesions are being diagnosed with increasing frequency in asymptomatic patients or incidentally through investigation of an unrelated presenting symptom. With the standard use of cross-sectional imaging, such as computed tomography (CT) or magnetic resonance imaging (MRI), pancreatic cystic lesions are found more commonly than previously reported. Furthermore, through expanding expertise at tertiary care centers as well as in the community setting, endoscopic ultrasound (EUS) evaluation and classification of pancreatic cystic lesions has become possible without the need for surgical extirpation. These imaging modalities allow the treatment algorithm used by most gastroenterologists and pancreatic surgeons to focus on the differentiation of benign cysts from those cysts that are malignant or have malignant potential.
What is the procedure for cyst excision?
For the rare cyst of the neck of the pancreas, a central pancreatectomy may be employed as the procedure for cyst excision. The benefits of central pancreatectomy focus on pancreatic parenchymal preservation. Caution must be used when recommending and performing central pancreatectomy.
Why is it important to have a pancreatic lesion?
First, it is of utmost importance to ensure the benign or low malignant potential nature of the lesion due to the oncologic limitations of central pancreatectomy. Second, several high-volume pancreatic centers have documented a high morbidity rate associated with central pancreatectomy.
What is the decision to operate on a tail or head cyst?
The decision to operate on a tail or head cyst is multifactorial and must account for patient-presenting symptoms, CT and EUS findings, and cyst fluid analysis. In my mind, I do not necessarily change my diagnostic algorithm based on cyst location alone. At high-volume centers, pancreaticoduodenectomy and distal pancreatectomy are able to be performed with very low morbidity and mortality rates. More importantly, both patient and cyst factors must play a role. Patient fitness must be accounted for but in suitable operative candidates, operative resection should be performed in the symptomatic patient. For borderline candidates or those that are asymptomatic, further investigation to determine the nature of the cystic neoplasm is warranted. CT may reliably differentiate a serous from MCN or IPMN. EUS may be used to evaluate the cystic neoplasm and obtain fluid for cytology, carcinoembryonic antigen (CEA) level analysis, and mucin stain. The presence of mucin or a high CEA level (>192) suggests a mucin-producing or premalignant tumor that warrants resection. EUS also allows evaluation of the cyst wall for the presence of papillary projections or mural nodules, both of which should lead one toward operative excision.
Can a cyst be resected?
Cysts located in the head of the pancreas are resected with standard or pylorus-preserving pancreaticoduodenectomy. Patients presenting with pain or jaundice warrant resection. For the asymptomatic patient, investigation is similar to that for the asymptomatic lesion of the body/tail described above. For patients found to have mucinous cysts of the head of the pancreas, I feel that pylorus preservation provides better gastric function and long-term quality of life without infringing on the oncologic principles of the resection.
Can a cystic lesion be excision?
In summary, once a cystic lesion is identified in the pancreas, operative excision should be recommended for the symptomatic patient. In patients who are asymptomatic, further investigation should be performed in order to differentiate a serous (benign) from a mucinous (malignant or premalignant) cystic neoplasm.
What is a pancreas specific meeting?
The multidisciplinary team holds weekly pancreas-specific meetings to discuss all cases and arrive at a mutually agreed-upon treatment plan tailored to each patient’s needs. “Each team member has a role to play in taking care of the patient,” said Dr. Richard Schulick, chairman of CU’s Department of Surgery and director of the Cancer Center.
What to do if cancer has not spread?
If the cancer has not spread, surgery could still be an option. Patients in that situation could consider seeking a second opinion, he maintained. “If you can control the disease, you can be more aggressive in removing the source of the cancer cells, which is the primary tumor,” Del Chiaro said.
Is there a reliable test for pancreatic cancer?
Pancreatic cancer is a stubborn opponent. It’s situated deep in the body and is therefore difficult to reach. As yet there is no reliable test for it. But experience helps to level the playing field, Del Chiaro said, noting the Cancer Center performed some 200 procedures for pancreatic disease last year.
What organs did Del Chiaro remove?
In a Whipple Procedure, Del Chiaro removed half of Page’s pancreas; the distal bile duct, which runs through the pancreas into the small intestine; the gallbladder; and the first part of the small intestine. He then reconnected the remaining pancreas to Page’s digestive organs.
Is the University of Colorado Cancer Center a pancreas center?
University of Colorado Cancer Center was recently named a Center of Excellence by the National Pancreas Foundation. The designation reflects the Cancer Center’s broad range of medical, educational and social services as well as its commitment to research.
Can a surgeon operate on pancreatic cancer?
One such difference is the willingness of the Cancer Center to more often consider surgery for patients with pancreatic cancer, Schulick said. He noted, for example, that many surgical oncologists will not operate on pancreas cancer that has invaded the main arteries and vein that feed the organ.
What are the diagnostic tools for pancreatic pseudocysts?
A variety of diagnostic tools including CT scanning, transcutaneous and endoscopic ultrasound, ERCP and cyst aspiration, chemistry and cytology are used for the diagnostics of pancreatic pseudocysts. According to the Atlanta classification a pseudocyst is characterized by presence of a defined wall of fibrous or granulomatous tissue whereas the acute fluid collection lacks that boundary. However, a late pancreatic necrosis may also have a partly organized encapsulated morphology and differentiation becomes more difficult 20. On CT imaging the capsule or wall of a pseudocyst shows evidence of contrast enhancement. A necrosis, particularly an infected one, can be presumed by non-enhancing zones or a heterogeneous pancreas seen on CT. However, the final diagnosis should correlate with the clinical condition of the patient 21.
What is a pseudocyst in the pancreas?
From a histopathological viewpoint, pancreatic pseudocysts can be described as fluid-filled cavities arising from the pancreas and surrounded by a wall of fibrous or inflammatory tissue, but lacking an epithelial cover 1. The cyst can be filled with pancreatic juice containing amylase, lipase and zymogens or, if no communication with the pancreatic ducts exists, with protease-free serous fluid.
How many cases of pseudoaneurysms have to be ruled out?
Neoplasm and pseudoaneurysm have to be ruled out 42
How long does a pseudocyst last?
According to Warshaw and Rattner, a pseudocyst is unlikely to resolve spontaneously if: a) it persists for more than 6 weeks, b) chronic pancreatitis is evident, c) there is a pancreatic duct anomaly (except for a communication with the pseudocyst) or d) the pseudocyst is surrounded by a thick wall 43. Studying 92 patients with chronic alcoholic pancreatitis, Gouyon and co-workers reported a spontaneous regression rate of 25.7%. However, pseudocysts >4 cm and those localized extrapancreatically were found to represent predictive factors for persistent symptoms and/or complications 40.
How long does it take for a pseudocyst to resolve?
Indications for immediate or elective interventions are summarized in Table I2,40. The management of pseudocysts also depends on the aetiology. Cystic pancreatic lesions, arising after an episode of acute pancreatitis, may resolve without treatment over a period of 4–6 weeks, whereas in chronic pancreatitis spontaneous pseudocyst resolution occurs rarely as maturation of the cyst wall is already complete 41,42. The probability of spontaneous resolution ranges widely from 8% to 85% 43, depending on the aetiology, the localization and, predominantly, the size.
What is ERCP in pancreatic duct?
Endoscopic retrograde cholangiopancreaticography (ERCP) is of major importance regarding the management of pseudocysts not only as a diagnostic tool, but also for endoscopic therapy. Although ERCP provides less information regarding the size and surrounding visceral structures than CT and ultrasound, it provides important information on the anatomy of the pancreatic and biliary ductal system and helps categorize pancreatic pseudocysts according to the classification systems by Nealon and Walser 5or D'Egidio and Schein 4. Communication of pancreatic pseudocysts with the pancreatic duct can be identified in 40–69% and this suggests therapy by transpapillary drainage. It is noteworthy that in the case of a suspected pancreatic pseudocyst with a communication to the pancreatic duct system, antibiotic prophylaxis before the examination is required to prevent secondary infection of the cystic lesion. Studies have demonstrated that 62–80% of patients show retrograde filling of the pseudocyst with contrast material proving the presence of a duct–pseudocyst communication 16,34,35. Common bile duct stricture is a frequent complication in chronic pancreatitis with a reported incidence of 3–23% and sometimes caused by a pancreatic pseudocyst in the head of the organ. Nealon et al. 36have shown that, as a result of ERCP findings, the initially planned operative strategy was altered in 24 of 41 patients (22 of 26 chronic pancreatitis patients). Evaluating the pancreatogram of 24 patients, originally classified as acute pancreatitis, ERCP even led to a change in diagnosis in 9 patients and patients were classified as suffering from chronic pancreatitis instead. Even more impressively, Laxson et al. 16reported that ERCP changed the surgical management in 8 of 25 patients (32%).
Is pancreatic cystic lesion heterogeneous?
Since pancreati c cystic lesions are pathologically a heterogeneous group, high-resolution EUS imaging helps to detect the majority of cystic lesions and, for small lesions <2 cm in diameter, EUS appears to be of particular high diagnostic sensitivity 25,26. Endoscopic ultrasound was reported to be superior to CT regarding small lesions (<2 cm in diameter) because of better spatial resolution 24. There has been some discussion about higher sensitivity of EUS in identification of debris within a pseudocyst 27but literature regarding solid material within a cyst is not sufficient to give a final answer on that issue yet. Whether EUS-guided fine-needle aspiration (FNA) is clearly helpful for distinguishing between benign or malignant cystic lesion is not clear yet, as the success rate and sensitivity of this technique vary greatly in different studies. Data from 123 patients with pancreatic cystic lesions of unknown origin indicated that the combination of EUS with FNA allowed for the correct diagnosis in 97%, whereas EUS alone yielded only 73% correct diagnoses 28. A second study on 96 patients compared data from EUS-FNA with the results based on surgery and histology. The sensitivity of FNA was calculated with only 50% in patients with a cystic pancreatic lesion 29. The Cooperative Pancreatic Cyst Study in 2004 reported 341 patients with cystic lesions >1 cm on EUS. They performed EUS + FNA with CEA, CA 72-4, CA 125, CA 19-9, CA 15-3, as well as cytology. The major finding of this large multicentre study in favour of FNA is that when CEA is found to be >192 ng/ml in the cystic fluid, a malignant pancreatic lesion can be assumed with a sensitivity of 73% and a specificity of 84% (p<0.001) 23.
I Have A Cyst in My Pancreas…Now What?
Where to Begin?
A Bit of Background
- In general, there are two main varieties of pancreatic cysts based on the type of fluid they contain. The most common cysts are either serous (containing a thin type of fluid) or mucinous (containing a thicker, more viscous fluid). For the most part, serous cysts tend to be benign (non-cancerous). Most of the mucinous cysts are benign as well although there are a few subtypes th…
What’s Next?
- In many cases, your doctor may be able to get a sense of what type of cyst you have based on the already available imaging tests. Otherwise, MRI can be especially useful for further characterization. If potentially concerning features are detected on imaging studies or if there remains significant uncertainty related to the nature of the cyst, additional information can be ga…
What Treatment Is available?
- At present, the only curative treatment is surgery. As any surgery on the pancreas is a major undertaking. Therefore, it is best to reserve resection for cases in which there is a significant concern for cancer. This represents a minority of cases. In the vast majority of cases, surveillance with periodic imaging tests is all that is needed.
What Approach Is Going to Work Best For Me?
- You should be aware that the management of these cysts continues to evolve. Researchers in the field are working diligently to identify more accurate early markers of malignancy. Further research is being conducted to determine the best surveillance interval to monitor these cysts. In the meantime, it is important that you work together with your healthcare provider to arrive at th…