Monoclonal antibody
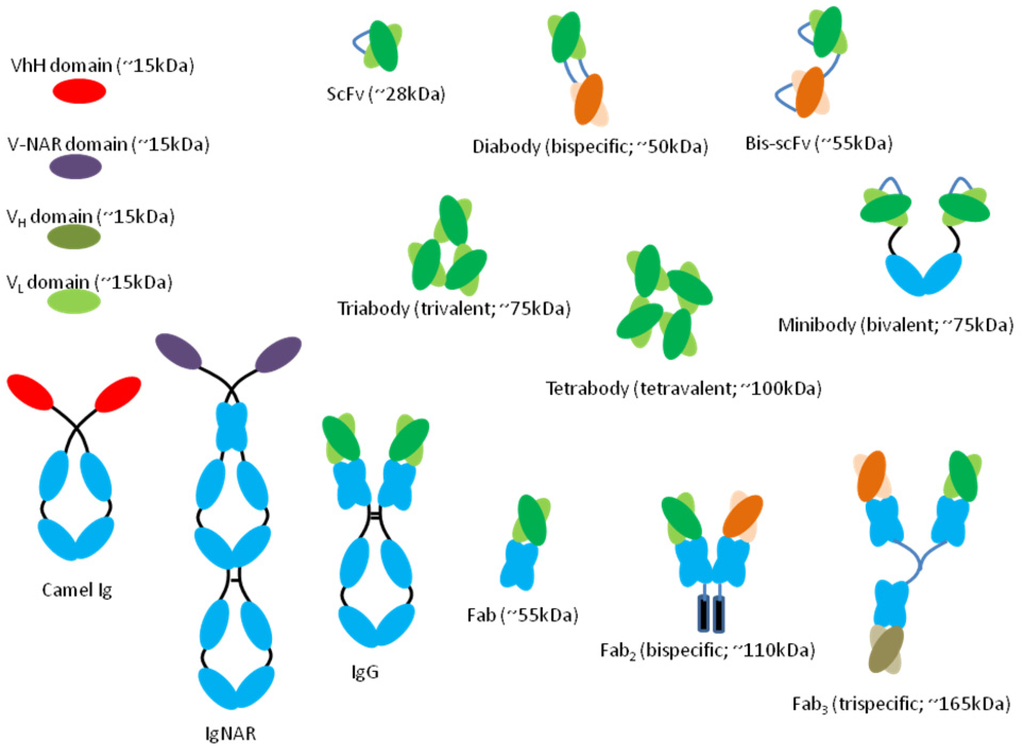
Monoclonal antibodies are antibodies that are made by identical immune cells that are all clones of a unique parent cell. Monoclonal antibodies can have monovalent affinity, in that they bind to the same epitope. In contrast, polyclonal antibodies bind to multiple epitopes and are usually made b…
Can monoclonal antibodies kill you?
Dec 28, 2021 · All of the monoclonal antibodies we give are injections, mostly intravenous (IV) infusions. This means the drug goes directly into your blood through a small needle inserted into a vein in your arm. To receive a monoclonal antibody infusion, you must have tested positive for COVID-19 and meet at least one of the following requirements: Age 65 or older
Are there side effects of monoclonal antibody treatment?
Jan 06, 2022 · Who is eligible for monoclonal antibody therapy? Given that COVID-19 vaccination provides strong protection against severe disease and need for hospitalization, monoclonal antibody therapy is an option for certain high-risk patients with COVID-19. THE FDA expanded EUA of two monoclonal antibody treatments to include patients as young as newborns. Criteria for …
Does Medicare cover monoclonal antibodies?
Dec 21, 2021 · To get the treatment administered, you’ll get antibodies either by four subcutaneous injections in areas like your arms and belly in quick succession, or the treatment will be given to you through...
Can you still get monoclonal antibodies?
Apr 07, 2022 · All monoclonal antibody (mAb) therapies are in limited supply, and not everyone will be eligible for treatment. A prescription from a healthcare provider is required to receive any mAb therapy. Variants, like Omicron, may have an impact on the effectiveness of mAb therapies.

How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
What is a monoclonal antibody for COVID-19?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells. Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
Who could benefit from monoclonal antibody therapy to prevent COVID-19?
See full answerVaccines are the best way to protect against COVID-19. But some people with weakened immune systems do not produce enough antibodies after vaccination, and others are severely allergic to the vaccine. The FDA recently authorized Evusheld, a pre-exposure prophylaxis (PrEP) monoclonal antibody therapy developed by AstraZeneca, which should help prevent COVID-19 in these populations.To be eligible for Evusheld, individuals must be 12 years or older and have a moderately to severely weakened immune system, or have a history of severe adverse reactions to the COVID-19 vaccine or its components. In addition, the therapy cannot be given to someone with a current SARS-CoV-2 infection, or who has been recently exposed to someone who is infected. Evusheld is given as two consecutive shots, and evidence suggests it can help prevent symptomatic infection for at least six months.Apr 1, 2022
Is there a monoclonal antibody therapy for post COVID-19 exposure?
FDA authorizes bamlanivimab and etesevimab monoclonal antibody therapy for post-exposure prophylaxis (prevention) for COVID-19 | FDA.Sep 16, 2021
What is a monoclonal antibody?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells.Mar 31, 2022
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
Are antibodies beneficial during the COVID-19 pandemic?
When reinfections or breakthrough infections happen, having antibodies plays an important role in helping prevent severe illness, hospitalization, and death. For many diseases, including COVID-19, antibodies are expected to decrease or “wane” over time.Nov 10, 2021
Who might benefit from dexamethasone if they have COVID-19?
Dexamethasone is a corticosteroid used in a wide range of conditions for its anti-inflammatory and immunosuppressant effects.It was tested in hospitalized patients with COVID-19 in the United Kingdom’s national clinical trial RECOVERY and was found to have benefits for critically ill patients.Oct 16, 2020
What do antibodies do to protect against COVID-19?
Antibodies are specialized proteins that are part of your immune system. They help protect against viruses, bacteria and other foreign substances. In the case of COVID-19, after you're infected with the SARS-CoV-2 virus, your immune system recognizes the virus as a foreign substance and forms antibodies against it.Nov 10, 2021
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
Is there an antibody cocktail for COVID-19?
The treatment, bamlanivimab and etesevimab administered together, was granted FDA emergency use authorization in February. Eli Lilly and the FDA stipulated that the antibody cocktail is authorized as a COVID-19 prophylaxis only for individuals who have been exposed to the virus.Sep 16, 2021
Is it possible to develop immunity to COVID-19 after being exposed?
In addition, the hope is that people who've been exposed to COVID-19 also develop an immunity to it. When you have immunity, your body can recognize and fight off the virus. It's possible that people who've had COVID-19 can get sick again -- and maybe infect other people.Jan 21, 2022
What is the function of antibodies?
Antibodies are proteins that exist in our bodies as part of our immune system to recognize and defend against harmful viruses and bacteria. Monoclonal antibodies are made in a laboratory and designed to target a specific virus or bacteria.
Does infusion cause nausea?
Some people may experience infusion-related side effects, such as nausea and dizziness, that are short-lived and go away on their own. As with any medication, there is the potential for mild or more severe allergic reactions, which are uncommon.
What is mAb treatment?
It’s called monoclonal antibody (mAb) treatment. Some early evidence suggests that mAb treatment can reduce the amount of the SARS-CoV-2 virus (the virus that causes COVID-19) in a person's system. This amount is known as viral load.
How long does it take for a virus to develop antibodies?
A vaccine triggers your body’s natural immune response, but can take weeks to develop enough antibodies and prevent some kinds of infection. Some vaccines for COVID-19 require two shots, so your body can develop its own immune response to the disease.
How long do you have to be isolated from a virus?
It’s important to know that even if you start feeling better, you could still spread the virus for a while. So, you’ll need to isolate yourself (be alone) until all of these things happen: 1 At least 10 days have passed since your first symptoms of COVID-19 2 You haven’t had a fever in at least 24 hours, without taking any medicine that reduces fever 3 Your other symptoms of COVID-19 are improving
What are the symptoms of an allergic reaction?
Tell your healthcare provider right away if you get any of the following signs and symptoms of allergic reactions: fever; chills; nausea; headache; shortness of breath; low blood pressure; wheezing; swelling of your lips, face, or throat; rash, including hives; itching; muscle aches; and/or dizziness.
What are the side effects of monoclonal antibody therapy?
One possible side effect of monoclonal antibody therapy is an allergic reaction. These reactions typically only occur during infusion or soon after, and your care team will closely monitor for any signs of an allergic reaction. However, because an infusion reaction can also be delayed, contact your doctor immediately if you notice any of the following signs of an allergic reaction: 1 Fever and/or chills 2 Nausea 3 Headache 4 Shortness of breath 5 Low blood pressure 6 Wheezing 7 Swelling of lips, face or throat 8 Muscle aches 9 Hives or itchiness
What are monoclonal antibodies?
However, monoclonal antibodies are mass-produced in a laboratory and are designed to recognize a specific component of this virus — the spike protein on its outer shell .
How long should you wait to get a second shot?
If you already received the first dose of vaccine before monoclonal antibody therapy, current CDC guidelines recommend you wait 90 days before receiving the second dose. Categories: Tips to Live By. Tags: Coronavirus, Infectious Disease.
What are the high risk people?
Those who are at high risk include people who: Are 65 years of age or older. Are at least 55 years of age and have heart disease, hypertension or a chronic respiratory disease such as COPD. Have a BMI above 35. Have chronic kidney disease.