Common tests & procedures
- Preference for cool temperature
- Weight loss with increased appetite
- Prominence of eyes, puffiness of lids
- Pain or irritation of eyes
- Blurred or double vision, decreasing acuity, decreased motility
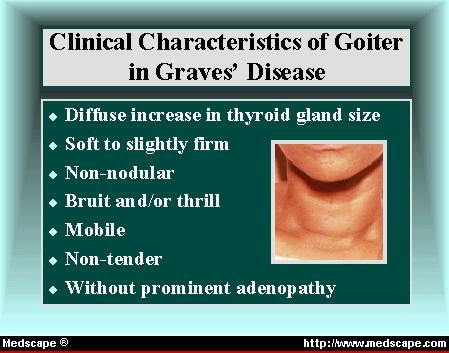
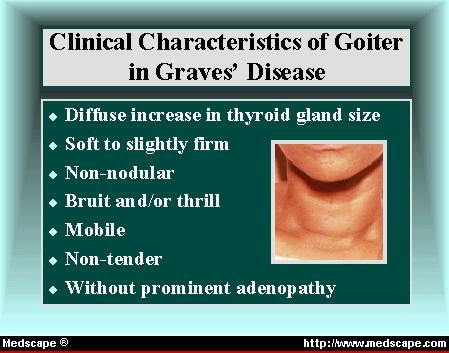
- Goiter
- Dyspnea
- Palpitations or pounding of the heart
- Ankle edema (without cardiac disease)
How to diagnosis Graves disease?
- Weight loss
- Hyperkinetic behavior, thought, and speech
- Restlessness
- Lymphadenopathy and occasional splenomegaly
- Eyes
- Prominence of eyes, lid lag, globe lag
- Exophthalmos, lid edema, chemosis, extraocular muscle weakness
- Decreased visual acuity, scotomata, papilledema, retinal hemorrhage, and edema
- Goiter
- Sometimes enlarged cervical nodes
What is the diagnosis of Graves disease?
- If your lids cannot close completely over your eyes, use eye patches at night and don't sleep with a ceiling fan on. ...
- Use over-the-counter or prescription artificial tears to moisten eyes whenever they feel dry.
- If your eyes are red and swollen in the morning, sleep with your head elevated.
How do you cure Graves disease?
Untreated, Graves’ disease can cause serious health problems, including a rapid and irregular heartbeat that can lead to blood clots, stroke , heart failure , and other heart-related problems thinning bones, osteoporosis , and muscle problems
How serious is Graves disease?
Why are T3 and T4 levels ordered for Graves disease?
Normal ranges of T3 and T4 are needed to regulate your body's metabolism at the cellular level, so in the blood test, your doctor will be looking for abnormal levels. People with Graves' disease will usually have too much T3 and T4 in their blood.
What additional tests would confirm the diagnosis of Graves disease?
How do doctors diagnose Graves' disease?Blood tests. These tests can measure the levels of your thyroid hormones and also check for TSI.Radioactive iodine uptake test. ... Thyroid scan. ... Doppler blood flow measurement link.
What are the three main methods used to manage a patient with Graves disease?
Graves' disease is treated with any of three effective and relatively safe initial treatment options: antithyroid drugs (ATDs), radioactive iodine ablation (RAIU), and surgery.
Can T3 and T4 be normal in Graves disease?
Graves' disease may present only with subclinical hyperthyroidism (normal total and free T3 and T4 with suppressed TSH levels).
What is TSI test for thyroid?
TSI stands for thyroid stimulating immunoglobulin. TSIs are antibodies that tell the thyroid gland to become more active and release excess amounts of thyroid hormone into the blood. A TSI test measures the amount of thyroid stimulating immunoglobulin in your blood.
What does TRAb test for?
The TRAb test detects the autoantibody that's associated with Graves' disease. An antibody is a specialized protein made by your immune system. Antibodies are custom made to kill pathogens in your body, such as viruses or bacteria.
What blood test shows Graves disease?
Radioactive iodine uptake. The amount of radioactive iodine taken up by the thyroid gland helps determine if Graves' disease or another condition is the cause of the hyperthyroidism. This test may be combined with a radioactive iodine scan to show a visual image of the uptake pattern.
Can you have a normal TSH with Graves disease?
Some patients with Graves' disease may have subclinical (mild) hyperthyroidism without symptoms but with a goiter, suppressed TSH, TSH receptor antibodies, but with normal T4 and T3.
What is the best test for hyperthyroidism?
Blood tests that measure thyroxine and thyroid-stimulating hormone (TSH) can confirm the diagnosis. High levels of thyroxine and low or nonexistent amounts of TSH indicate an overactive thyroid. The amount of TSH is important because it's the hormone that signals your thyroid gland to produce more thyroxine.
What does high FT3 and FT4 mean?
Free triiodothyronine (FT3) and free thyroxine (FT4): High levels of free thyroid hormones in the blood may be a sign of an overactive thyroid, and low levels could be a sign of an underactive thyroid.
What if T3 and T4 are low and TSH is normal?
What's the outlook? Subclinical hyperthyroidism is when you have low levels of TSH but have normal levels of T3 and T4. If you're experiencing symptoms of subclinical hyperthyroidism, your doctor can use a series of blood tests to come to a diagnosis.
What to do if TSH is high but T3 and T4 are normal?
When TSH level is borderline high, most of the times T3, T4 levels are normal, especially in the early stages of Hypothyroidism. You should do Anti TPO antibody and then you may have to start thyroxine tablet. Was this answer helpful?
How to treat Graves disease?
Treatment of Graves’ disease cannot yet be aimed at the cause because it is still unknown. One seeks to control thyrotoxicosis when that seems to be the major indication, or the ophthalmopathy when that aspect of the disease appears to be more urgent. The available forms of treatment, including surgery, drugs, and 131-Itherapy, are reviewed. There is a difference of opinion as to which of these modalities is best, but to a large degree guidelines governing choice of therapy can be drawn. Antithyroid drugs are widely used for treatment on a long- term basis. About one-third of the patients undergoing long-term antithyroid therapy achieve permanent euthyroidism. Drugs are the preferred initial therapy in children and young adults. Subtotal thyroidectomy is a satisfactory form of therapy, if an excellent surgeon is available, but is less used in 2016. The combined use of antithyroid drugs and iodine makes it possible to prepare patients adequately before surgery, and operative mortality is approaching the vanishing point. Many young adults, are treated by surgery if antithyroid drug treatment fails.
How many guidelines are there for Graves disease?
We note that there are currently available 2 very extensive Guidelines on Diagnosis and Treatment of Graves’ Disease—The 2016 ATA guideline --- http://online.liebertpub.com/doi/pdfplus/10.1089/thy.2016.0229(270 pages), and the AACE 2011 version on Hyperthyroidism and other Causes of Thyrotoxicosis (65 pages)--https://www.aace.com/files/hyperguidelinesapril2013.pdf.
How long does it take for a thyroid isotope to be uptake?
Thyroid Isotope uptake-In patients with thyrotoxicosis the RAIU (Radioactive Iodine Uptake) at 24 hours is characteristically above normal. In the United States, which has had an increasing iodine supply in recent years, the upper limit of normal is now about 25% of the administered dose. This value is higher in areas of iodine deficiency and endemic goiter. The uptake value at a shorter time interval, for example 6 hours, is as valid a test and may be more useful in the infrequent cases having such a rapid isotope turnover that "uptake" has fallen to normal by 24 hours. If there is reason to suspect that thyroid isotope turnover is rapid, it is wise to do both a 6- and a 24-hour RAIU determination during the initial laboratory study. As noted below, rapid turnover of 131-I can seriously reduce the effectiveness of 131-I therapy. Similar studies can be done with 123-I and also technetium. Because of convenience, and since serum assays of thyroid hormones and TSH are reliable and readily available, the RAIU is now infrequently determined unless 131-I therapy is planned.. It is however useful in patients who are mildly thyrotoxic for factitia thyrotoxicosis, subacute thyroiditis and painless thyroiditis in whom RAIU is low, thus confirming thyrotoxicosis in the absence of elevated RAIU. This may include patients with brief symptom duration, small goiter, or lacking eye signs, absent family history, or negative antibody test result. Obviously other causes of a low RAIU test need to be considered and excluded. Tests measuring suppressibility of RAIU are of historical interest(13-15)
What is the TSH level for thyroid?
As an initial single test, a sensitive TSH assay may be most cost-effective and specific. TSH should be 0 - .1 µU/ml in significant thyrotoxicosis, although values of .1 - .3 are seen in patients with mild illness, especially with smoldering toxic multinodular goiter in older patients(1.1). TSH can be low in some elderly patients without evidence of thyroid disease. TSH can be normal -- or elevated -- only if there are spurious test results from heterophile antibodies or other cause, or the thyrotoxicosis is TSH-driven, as in a pituitary TSH-secreting adenoma or pituitary resistance to thyroid hormone.
What are some examples of Graves disease?
Examples are certain cases of pheochromocytoma, polycythemia, lymphoma, and the leukemias. Pulmonary disease, infection, parkinsonism, pregnancy, or nephritis may stimulate certain features of thyrotoxicosis. Diagnosis of the classic form of Graves’ disease is easy and depends on the recognition of the cardinal features ...
Does propranolol help with thyrotoxicosis?
This drug prevents the concentration of iodide by the thyroid. Beta adrenergic blockers such as propranolol have a place in the treatment of thyrotoxicosis. These drugs alleviate some of the signs and symptoms of the disease but have little or no direct effect on the metabolic abnormality itself.
Can T3 be elevated?
In patients with severe illness and thyrotoxicosis, especially those with liver disease or malnutrition or who are taking steroids or propranolol, the serum T3 level may not be elevated, since peripheral deiodination of T4 to T3 is suppressed ("T4 toxicosis").
What test is used to confirm Graves disease?
If this test is negative (which can also occur in some patients with Graves’ disease), or if this test is not available, then your doctor should refer you to have a radioactive iodine uptake test (RAIU) to confirm the diagnosis.
HOW IS THE DIAGNOSIS OF GRAVES' DISEASE MADE?
The diagnosis of hyperthyroidism is made on the basis of your symptoms and findings during a physical exam and it is confirmed by laboratory tests that measure the amount of thyroid hormones (thyroxine, or T4, and triiodothyronine, or T3) and thyroid-stimulating hormone (TSH) in your blood (see the Hyperthyroidism brochure ). Clues that your hyperthyroidism is caused by Graves’ disease are the presence of Graves’ eye disease and/or dermopathy (see above), a symmetrically enlarged thyroid gland and a history of other family members with thyroid or other autoimmune problems, including type 1 diabetes, rheumatoid arthritis, pernicious anemia (due to lack of vitamin B12) or painless white patches on the skin known as vitiligo.
WHAT CAUSES GRAVES' DISEASE?
Graves’ disease is triggered by a process in the body’s immune system, which normally protects us from foreign invaders such as bacteria and viruses. The immune system destroys foreign invaders with substances called antibodies produced by blood cells known as lymphocytes. Sometimes the immune system can be tricked into making antibodies that cross-react with proteins on our own cells. In many cases these antibodies can cause destruction of those cells. In Graves’ disease these antibodies (called the thyrotropin receptor antibodies (TRAb) or thyroid stimulating immunoglobulins (TSI) do the opposite – they cause the cells to work overtime. The antibodies in Graves’ disease bind to receptors on the surface of thyroid cells and stimulate those cells to overproduce and release thyroid hormones. This results in an overactive thyroid ( hyperthyroidism ).
WHAT IS THE THYROID GLAND?
The thyroid gland is a butterfly-shaped endocrine gland that is located in the lower front of the neck. The thyroid makes thyroid hormones, which are secreted into the blood and then carried to every tissue in the body. Thyroid hormones help the body use energy, stay warm and keep the brain, heart, muscles, and other organs working appropriately.
How long does Graves disease last?
If your hyperthyroidism due to Graves’ disease persists after 6 months, then your doctor may recommend definitive treatment with either radioactive iodine or surgery.
How long does it take for eye symptoms to show after Graves disease?
Eye symptoms most often begin about six months before or after the diagnosis of Graves’ disease has been made. Seldom do eye problems occur long after the disease has been treated. In some patients with eye symptoms, hyperthyroidism never develops and, rarely, patients may be hypothyroid. The severity of the eye symptoms is not related to the severity of the hyperthyroidism.
Can you measure thyroid blood flow with ultrasonography?
Also, in some patients, measurement of thyroidal blood flow with ultrasonography may be useful to establish the diagnosis if the above tests are not readily available.
What test is used to diagnose Graves disease?
You may also have these tests to confirm a Graves’ disease diagnosis: Blood test: Thyroid blood tests measure TSI, an antibody that stimulates thyroid hormone production. Blood tests also check amounts of thyroid-stimulating hormones (TSH). A low TSH level indicates that the thyroid gland is producing too much hormone.
What is Graves disease?
Graves’ disease is an autoimmune disease that affects the thyroid gland. The gland produces too much thyroid hormone, a condition known as hyperthyroidism. Thyroid hormones regulate body temperature, heart rate and metabolism. An overactive thyroid causes problems with organs like the heart, as well as bones and muscles. Treatments can help.
What is the butterfly gland in the neck?
This butterfly-shaped gland in the neck produces hormones that regulate how your body uses energy (metabolism). Graves’ disease is the most common cause of hyperthyroidism (overactive thyroid gland). People with Graves’ disease make too much thyroid hormone, which can damage the heart and other organs. The condition gets its name ...
What age does Graves disease occur?
It typically occurs in people between the ages of 30 and 50. The condition tends to run in families. Your risk of developing Graves’ disease increases if you have: Family history of thyroid disease. Another autoimmune disease, such as rheumatoid arthritis, lupus or Type 1 diabetes. Celiac disease.
What are the diseases that cause autoimmune disease?
Another autoimmune disease, such as rheumatoid arthritis, lupus or Type 1 diabetes. Celiac disease. Hormone disorder, such as Addison’s disease. Pernicious anemia (iron deficiency caused by a lack of vitamin B12). Vitiligo, a skin disorder that changes skin coloration.
How many people have Graves disease?
Graves’ disease affects one out of every 200 Americans, making it the top cause of hyperthyroidism.
Does Graves disease go away?
Graves’ disease is a lifelong condition. However, treatments can keep the thyroid gland in check. Medical care may even make the disease temporarily go away (remission): Beta-blockers: Beta-blockers, such as propranolol and metoprolol, are often the first line of treatment. These medications regulate your heart rate and protect your heart ...
WHAT ARE THE BENEFITS OF THYROIDECTOMY FOR GRAVES' DISEASE?
Thyroidectomy provides those with GD a rapid cure of hyperthyroidism and a transition from anti-thyroid medications to full thyroid hormone supplementation during the perioperative period (pre-surgery through postsurgery). Patients should continue all their anti-thyroid medications and beta blockers until the day of surgery, at which time patients should discontinue taking. Beta blockers may be continued for a few days after surgery and then may be tapered or stopped. Thyroid hormone supplementation is often started the following day, or a few days later in those patients with poor hormone control during the pre-operative period.
WHAT IS THE THYROID GLAND?
The thyroid gland is a butterfly-shaped endocrine gland that is normally located in the lower front of the neck. The thyroid’s job is to make thyroid hormones, which are secreted into the blood and then carried to every tissue in the body. Thyroid hormone helps the body use energy, stay warm and keep the brain, heart, muscles, and other organs working as they should.
WHAT ARE THE RISKS OF THYROIDECTOMY?
Risk of permanent injury is very low in experienced thyroid surgeon’s hands.
What supplements should I take before thyroid surgery?
Ensure you are taking your anti-thyroid medications, and any beta blockers as prescribed to provide optimal control of your thyroid hormone levels before surgery. Your surgeon may talk to you about starting a calcium supplement leading up to surgery, and a vitamin D supplement if you are deficient.
What happens after thyroid surgery?
Once the thyroid is removed, the surgeon closes up all the layers, and may or may not leave behind a small drain to remove any fluid that might build up in the space where the thyroid was previously . You will be observed for a period of time after surgery to ensure you are recovering well.
How long after thyroid surgery do you feel hyperthyroid?
The first few days after surgery you may feel a little hyperthyroid if some excess hormone was released during surgery. This will pass as your body uses up the extra hormone.
How long should I take beta blockers after thyroid surgery?
Beta blockers may be continued for a few days after surgery and then may be tapered or stopped.
Who should perform Graves disease surgery?
Graves' disease surgery should only be performed by highly expert thyroid surgeons. An occastional thyroid surgeon should not do this surgery.
What is Graves disease?
Graves' disease is the most common cause of overproduction of thyroid hormone within the body (hyperthyroidism). It is named after the physician that originally described the condition in 1835. Graves' disease is an autoimmune condition where the body, for some reason, recognizes itself as being abnormal and produces an antibody against itself. In Graves' disease, this antibody is produced against the thyroid gland itself. Today, Graves' disease can be diagnosed with a blood test that actually measures the anti-self directed antibody which is called thyroid stimulating immunoglobulin (TSI) There are several different approaches in the management of Graves' disease. These include medical managment with anti-thyroid medication, radioactive iodine therapy as well as surgery. Comprehensive evaluation and personalized care is necessary in the managment and cure of this disease. Surgery, has once again, evolved as a frequently sought curactive treatment for Graves' disease. Graves' disease requires total removal of the thyroid gland and should only be performed by expert thyroid surgeons and managed by an expert thyroid surgery team. This expert and focused thyroid surgery patient team makes all the difference to you as a patient. Written by Gary L. Clayman, DMD, MD, FACS. Dr. Clayman has published extensively in peer reviewed publications and books for more than three decades. Last updated April 11, 2021.
What Are the Symptoms Of Graves' Disease?
Early in the course of Graves' Disease, the symptoms may be similar to other conditions and may delay or confuse the diagnosis.
What Are The Physical Signs and Symptoms of Graves' Disease?
Untreated and undiagnosed Graves' disease may develop the following findings which will be readily appreciated by your skilled endocrinologist:
How big is a thyroid nodule?
This means that they are larger than about 1 centimeter (about 1/2 inch) across. If you are already planning a thyroid surgery for Graves' disease, then biopsy of a nodule would not necessarily be indicated unless it would change the approach for your thyroid surgery.
What antibody is produced in Graves disease?
In Graves' disease, this antibody is produced against the thyroid gland itself. Today, Graves' disease can be diagnosed with a blood test that actually measures the anti-self directed antibody which is called thyroid stimulating immunoglobulin (TSI) There are several different approaches in the management of Graves' disease.
Why do you have to repeat a FNA biopsy?
Sometimes an FNA biopsy will need to be repeated because the samples didn't contain enough cells. Most ultrasounds for Graves' disease will show that the Graves' diseased thyroid glands are benign. Rarely, the FNA biopsy may come back as benign even though a diagnosis of a thyroid cancer is actually present.
What kind of imaging is used to diagnose Graves disease?
Depending on your symptoms (e.g., exophthalmos), other tests may include a CT scan, MRI, or ultrasound (echography) of the eyes and eye sockets (called orbital imaging) in order to define the exact impact of Graves’ disease on the eyes and surrounding structures (e.g., muscles). The doctor combines your medical history, symptoms, ...
What is the test to see if thyroid is overactive?
A radioactive iodine uptake test and scan will measure the amount of iodine your thyroid absorbs and also determine if all or only part of the thyroid is overactive. This test is usually performed in a hospital or medical center’s nuclear imaging department.
Why do you take a RAIU before a thyroid scan?
Iodine is used because your thyroid gland naturally absorbs iodine through your bloodstream from foods that contain the element in order to make thyroid hormone. It’s a specific test because the thyroid absorbs iodine much better than other parts of the body, especially if your thyroid is overactive.
What does a high thyroid tracer mean?
A high uptake of iodine tracer may mean you have hyperthyroidism or Graves’ disease. Other Tests. Depending on your symptoms (e.g., exophthalmos), other tests may include a CT scan, MRI, or ultrasound ...
Why is my TSH low?
If you have Graves’ disease, your thyroid-stimulating hormone (TSH) level will probably be very low because the pituitary gland will try to compensate for the excess T3 and T4 hormones in the blood. It’ll stop producing TSH in an attempt to stop production of the thyroid hormones. Testing Total T3 and T4 Hormone Levels.
What is Tsi test?
Testing Thyroid-stimulating Immunoglobulin ( TSI) Levels. Thyroid-stimulating immunoglobulin (TSI) is a type of antibody (immunoglobulin) measured from drawn blood. TSIs can bind to tissues in the eyeballs and beneath the skin and contribute to the development of exophthalmos (bulging eyes) and pretibial myxedema ...
What hormones are tested by a doctor?
He or she may want to measure the thyroid-stimulating hormone (TSH), T3 (triiodothyronine), and T4 (thyroxine) hormone levels. T3 and T4 are the major hormones produced by your thyroid. TSH, which is released by the pituitary gland, ...
What is Graves disease?
Graves disease is an autoimmune disorder characterized by goitre, hyperthyroidism and, in 25% of patients , Graves ophthalmopathy. The hyperthyroidism is caused by thyroid hypertrophy and stimulation of function, resulting from interaction of anti-TSH-receptor antibodies (TRAb) with the TSH receptor ….
What is the cause of hyperthyroidism?
The hyperthyroidism is caused by thyroid hypertrophy and stimulation of function , resulting from interaction of anti-TSH-receptor antibodies (TRAb) with the TSH receptor on thyroid follicular cells.
Is Graves disease an autoimmune disease?
Graves disease is an autoimmune disorder characterized by goit re, hyperthyroidism and, in 25% of patients, Graves ophthalmopathy. The hyperthyroidism is caused by thyroid hypertrophy and stimulation of function, resulting from interaction of anti-TSH-receptor antibodies (TRAb) with the TSH receptor …. Graves disease is an autoimmune disorder ...

Treatment
Clinical Trials
Lifestyle and Home Remedies
Preparing For Your Appointment