Pseudomonas
Pseudomonas is a genus of Gram-negative, Gammaproteobacteria, belonging to the family Pseudomonadaceae and containing 191 validly described species. The members of the genus demonstrate a great deal of metabolic diversity and consequently are able to colonize a wide ran…
Aminoglycoside
Aminoglycoside is a medicinal and bacteriologic category of traditional Gram-negative antibacterial medications that inhibit protein synthesis and contain as a portion of the molecule an amino-modified glycoside. The term can also refer more generally to any organic molecule that contains a…
Carbapenem
Carbapenems are a class of highly effective antibiotic agents commonly used for the treatment of severe or high-risk bacterial infections. This class of antibiotics is usually reserved for known or suspected multidrug-resistant bacterial infections. Similar to penicillins and cephalospori…
What antibiotics are used to treat Pseudomonas?
Update on the treatment of Pseudomonas aeruginosa pneumonia
- Introduction. Pseudomonas aeruginosa is a Gram-negative non-fermenting bacillus that belongs to the family Pseudomonadaceae.
- Approach to treatment of P. aeruginosa pneumonia. ...
- Antipseudomonal therapy. ...
- New antipseudomonal antibiotics. ...
- Aerosolized antibiotics. ...
- Novel antibacterial agents. ...
- Conclusions. ...
- Transparency declarations. ...
What kills Pseudomonas naturally?
What kills Pseudomonas naturally? In fact, research shows oregano oil is effective against many clinical strains of bacteria, including Escherichia coli (E. coli) and Pseudomonas aeruginosa . To use oregano oil as a natural antibiotic, you can mix it with water or coconut oil.
What is the drug of choice for Pseudomonas?
Two agents from different classes should be used when the risk of antibiotic resistance is high (eg, in severe sepsis, septicemia, and inpatient neutropenia). Pseudomonas infection can be treated with a combination of an antipseudomonal beta-lactam (eg, penicillin or cephalosporin) and an aminoglycoside.
Which would be most effective against Pseudomonas?
- Wash your hands often. This is the best way to avoid getting pseudomonas.
- Rinse fruits and vegetables before eating.
- Clean your water bottles.
- Avoid unclean pools and hot tubs.
- Ask questions about your medical care.
- Take care of your health.
See more

What is the best antibiotic to treat Pseudomonas aeruginosa?
At present, the use of newer penicillins, piperacillin, azlocillin, or selected antipseudomonal cephalosporins, in combination with amikacin or tobramycin, appears to be the preferable antimicrobial therapy for serious P. aeruginosa infections.
What is the drug of choice for Pseudomonas?
Ceftazidime is the antibiotic of choice because of its high penetration into the subarachnoid space and the high susceptibility of Pseudomonas to this drug. Initial therapy in critically ill patients should include an intravenous aminoglycoside.
How Pseudomonas aeruginosa is treated?
Pseudomonas aeruginosa infections are generally treated with antibiotics. Unfortunately, in people exposed to healthcare settings like hospitals or nursing homes, Pseudomonas aeruginosa infections are becoming more difficult to treat because of increasing antibiotic resistance.
Which antibiotics is sensitive to Pseudomonas aeruginosa?
In the present study, P. aeruginosa was most susceptible to the following antibiotics, in order of decreasing effectiveness: cefepime, amikacin, ceftazidime, tobramycin, the combination of piperacillin and tazobactam, meropenem, imipenem, piperacillin, ciprofloxacin, gentamicin, and fosfomycin (Table 3).
Can Pseudomonas aeruginosa be treated with oral antibiotics?
Our Cochrane systematic review (last updated April 25, 2017) showed that nebulised antibiotics alone or in combination with oral ciprofloxacin are better than no eradication treatment for P aeruginosa.
Does ciprofloxacin treat Pseudomonas aeruginosa?
Ciprofloxacin was well tolerated. This new quinolone seems to be suitable for single drug treatment of Pseudomonas aeruginosa infections in patients with normal host defense mechanisms, while its therapeutic potential in compromised hosts requires further evaluation.
Does ceftriaxone treat Pseudomonas?
Ceftriaxone is also active against many strains of Pseudomonas aeruginosa. NOTE: Methicillin-resistant staphylococci are resistant to cephalosporins, including ceftriaxone.
Does amoxicillin treat Pseudomonas aeruginosa?
P. aeruginosa skin infection isolates were 100% resistant to ampicillin and amoxicillin, highly resistant to tetracycline (95%), amoxicillin/clavulanate (95%), cefalexin (87%) and azithromycin (84%), and susceptible to amikacin (87%), norfloxacin (71%) and meropenem (68%).
Does vancomycin treat Pseudomonas?
Vancomycin in combination with ciprofloxacin exhibited synergy against 7 of 10 strains of Pseudomonas aeruginosa. MICs for the microbial strains used in this study ranged from 0.0325 to 3.0 tig/mlfor ciprofloxacin and from 23.5 to >188 ,ug/ml for vancomycin.
Is doxycycline effective against Pseudomonas aeruginosa?
Polymyxin B–doxycycline in combination showed a synergistic effect against multi-drug-resistant Pseudomonas aeruginosa.
Is Pseudomonas aeruginosa resistant to gentamicin?
By disk diffusion antimicrobial susceptibility testing, 11% of 313 consecutive strains of Pseudomonas aeruginosa, examined during July to October 1973, were resistant to gentamicin (minimal inhibitory concentration 12.5 to >100 μg/ml), and a further 31% were moderately resistant (6.25 to 12.5 μg/ml) to gentamicin at ...
Does doxycycline treat Pseudomonas aeruginosa?
Pseudomonas aeruginosa ATCC 27853 and Escherichia coli ATCC 25922 were used as control strains. Testing against the P. aeruginosa strains revealed high MIC50 values for all the drugs except colistin. Doxycycline and colistin were both effective against the A.
Abstract
Infections with Pseudomonas aeruginosa have become a real concern in hospital-acquired infections, especially in critically ill and immunocompromised patients. The major problem leading to high mortality lies in the appearance of drug-resistant strains. Therefore, a vast number of approaches to develop novel anti-infectives is currently pursued.
Introduction
One of the most important challenges for physicians is the adequate treatment of infections due to Gram-negative pathogens because of the increasing antimicrobial resistance in the healthcare setting [ 1 ].
Risk factors for antimicrobial resistance in P. aeruginosa
Multi-drug resistance (MDR) has increased dramatically in recent years and is now recognized as a major threat worldwide [ 7 ]. Risk factors for the development of MDR strains have been evaluated in several studies.
Mechanisms of antibiotic resistance
Bacteria exhibit multiple resistance mechanisms to antibiotics including decreased permeability, expression of efflux systems, production of antibiotic inactivating enzymes and target modifications. P.
Laboratory role
Diagnostic laboratories need to implement several methodologies and procedures to identify P. aeruginosa strains and rapidly provide antibiotic susceptibility testing (AST) for the management of antibiotic regimens.
Clinical approaches to P. aeruginosa bacteremia
P. aeruginosa bloodstream infection (BSI) is a serious disease that requires prompt attention and pertinent clinical decisions in order to achieve a satisfactory outcome. Currently, Pseudomonas spp.
Management of P. aeruginosa VAP
P. aeruginosa is one of the leading causes of ventilator-associated pneumonia (VAP) in the US and Europe [ 77 – 79 ]. VAP due to P. aeruginosa is increasing in incidence and poses unique challenges for its clinical management. Risk factors for the development of P.
Why is P. aeruginosa so challenging to treat?
Treatment of P. aeruginosa infections is challenging because of the limited choices of antibiotics and the emergent resistance of the pathogen. The present review aims at addressing the management of P. aeruginosa infections and highlighting the novel antibiotics that show a future promising role.
What factors guide clinical decisions for empiric and directed P. aeruginosa therapy?
aeruginosa therapy include the epidemiology, the patient's risk factors, the site of infection, and the available treatment options.
What antibiotics are used for Pseudomonas aeruginosa?
aeruginosa infections in people with non-CF bronchiectasis. According to these guidelines, oral ciprofloxacin is a preferred treatment for a first infection, and intravenous treatment is to be considered for people who do respond. Resistant strains of this bacteria likely require combination antibiotic treatment, including ciprofloxacin, and combinations are recommended for bronchiectasis patients who “will require many subsequent antibiotic courses to reduce the development of drug resistance.”
What antibiotics are used for a thoracic infection?
The American Thoracic Society also recommends a combination antibiotic treatment that includes aminoglycosides, ticarcillin, ceftazidime, cefepime, aztreonam, ciprofloxacin and levofloxacin, with selection based on such considerations as the severity of the infection, underlying risk factors, and other (co-morbid) illnesses in a patient.
What are the most common pathogens in bronchitis?
Among the most common bacterial pathogens isolated in bronchiectasis are Haemophilus influenzae, a bacteria that can cause problems ranging from ear infections and bronchitis to pneumonia, and Pseudomonas aeruginosa, which can cause of variety of respiratory infections, including pneumonia, and severe systemic infections.
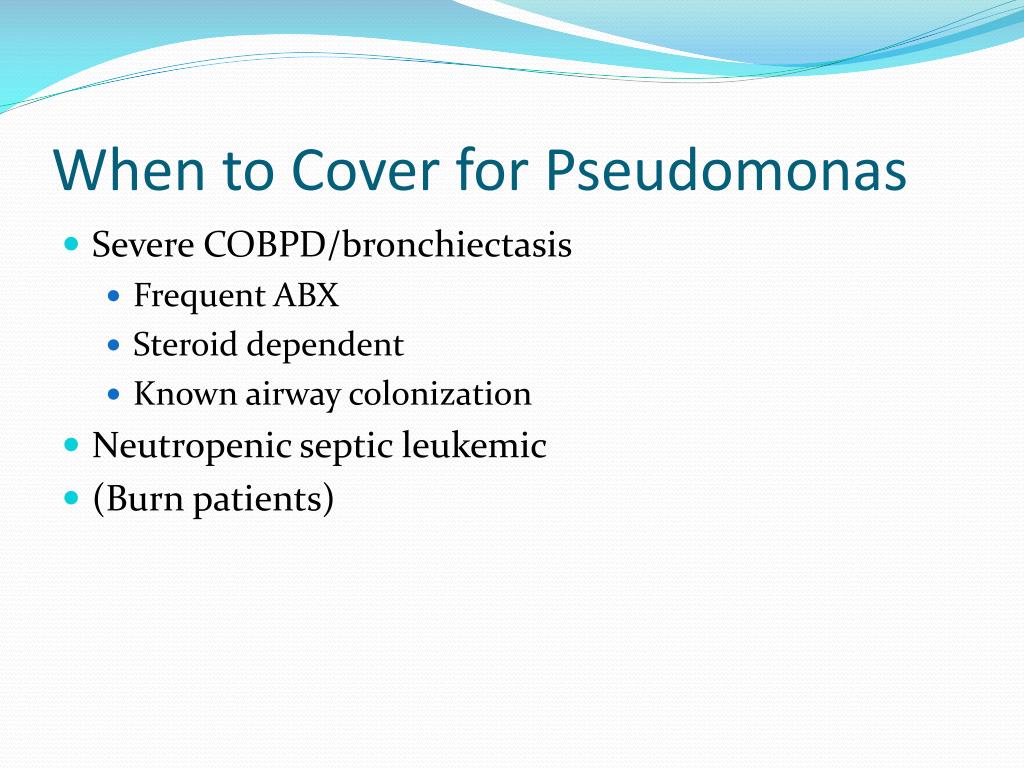
Why do bacteria persist in the airways?
The bacteria has a tendency to persist in bronchiectatic airways , due to its ability to produce virulence factors and modulate immune defences by quorum signaling and biofilm production. People with bronchiectasis and P. aeruginosa infection are known to have a lower quality of life than those with other bacterial infections, ...
Is P. aeruginosa resistant to colistin?
A retrospective study examined antibiotic resistance in 168 people with pneumonia caused by P. aeruginosa, and found the bacteria least resistant to treatment with colistin, although this bacteria is highly adaptive.
Is bronchitis a gram negative infection?
About one-third of bronchiectasis patients are known to have chronic P. aeruginosa infections. P. aeruginosa is a gram-negative bacteria, meaning that it is resistant to many medicines and increasingly resistant to available antibiotics.
Can you take ciprofloxacin for bronchiectasis?
Resistant strains of this bacteria likely require combination antibiotic treatment, including ciprofloxacin, and combinations are recommended for bronchiectasis patients who “will ...
