Which antibiotic is best for diabetic foot wound?
What antibiotic is used for foot infection?
How do you treat a diabetic wound infection?
Which medicine is best for foot infection?
Can a diabetic take amoxicillin?
Which antibiotic is best for wound infection?
- Amoxicillin-clavulanate (Augmentin, Augmentin-Duo)
- Cephalexin (Keflex)
- Clindamycin (Cleocin)
- Dicloxacillin.
- Doxycycline (Doryx)
- Trimethoprim-sulfamethoxazole (Bactrim, Septra)
Which ointment is best for diabetic wound?
How do you treat an open wound on a diabetic foot?
Is Betadine good for diabetic wounds?
Is amoxicillin good for a foot infection?
Are amoxicillin antibiotics?
How often should I take Flucloxacillin 500mg?
How to treat diabetic foot infection?
Surgery is the cornerstone of treatment for deep diabetic foot infection. Procedures range from simple incision and drainage to extensive multiple surgical debridements and amputation. Timely and aggressive surgical debridement or limited resection or amputation may reduce the need for more extensive amputation. 32 Emergent surgery is required for severe infection in an ischemic limb, necrotizing fasciitis, gas gangrene, and an infection associated with compartment syndrome. Surgical excision of affected bone has historically been the standard of care in patients with osteomyelitis. Nevertheless, successful therapy with a long course of antibiotics alone has been achieved in two thirds of patients with osteomyelitis. 12 As infection is controlled and the wound starts to granulate, primary closure may be successful. The wound may also be treated surgically with a flap or graft, left to heal by secondary intention, or managed with negative pressure dressings. 33
What are the most common pathogens in diabetic foot wounds?
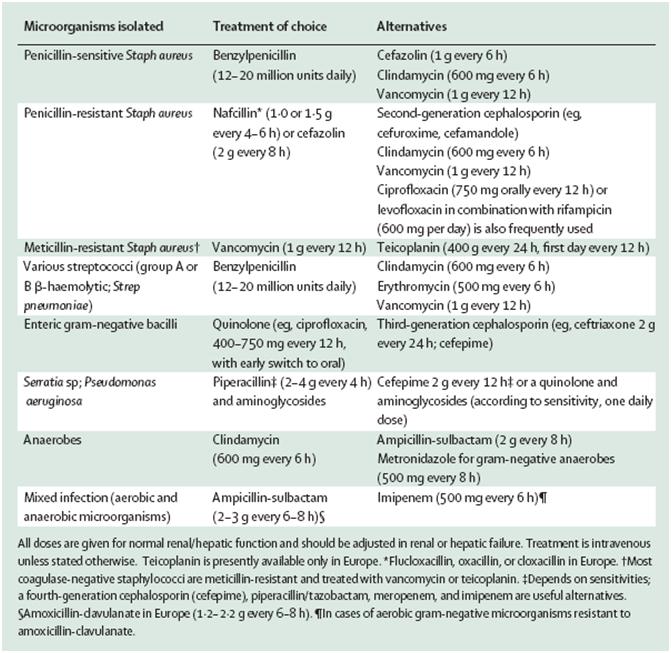
The most common pathogens in acute, previously untreated, superficial infected foot wounds in patients with diabetes are aerobic gram-positive bacteria, particularly Staphylococcus aureus and beta-hemolytic streptococci (group A, B, and others). 5 Infection in patients who have recently received antibiotics or who have deep limb-threatening infection or chronic wounds are usually caused by a mixture of aerobic gram-positive, aerobic gram-negative (e.g., Escherichia coli, Proteu s species, Klebsiella species), and anaerobic organisms (e.g., Bacteroides species, Clostridium species, Peptococcus and Peptostreptococcus species). 5 Anaerobic bacteria are usually part of mixed infections in patients with foot ischemia or gangrene. 6 Methicillin-resistant S. aureus (MRSA) is a more common pathogen in patients who have been previously hospitalized or who have recently received antibiotic therapy. MRSA infection can also occur in the absence of risk factors because of the increasing prevalence of MRSA in the community. 7, 8
Is diabetes a foot infection?
Foot infections are common in patients with diabetes and are associated with high morbidity and risk of lower extremity amputation. Diabetic foot infections are classified as mild, moderate, or severe. Gram-positive bacteria, such as Staphylococcus aureus and beta-hemolytic streptococci, are the most common pathogens in previously untreated mild ...
What antibiotics are used for soft tissue infection?
Mild soft tissue infection can be treated effectively with oral antibiotics, including dicloxacillin, cephalexin, and clindamycin. Severe soft tissue infection can be initially treated intravenously with ciprofloxacin plus clindamycin; piperacillin/tazobactam; or imipenem/cilastatin.
What are the most common complications of diabetes mellitus?
Types of infection include cellulitis, myositis, abscesses, necrotizing fasciitis, septic arthritis, tendinitis, and osteomyelitis. Foot infections are among the most common and serious complications of diabetes mellitus.
What are the factors that increase the risk of amputation?
They are associated with increased frequency and length of hospitalization and risk of lower extremity amputation. 1 Foot ulceration and infection are the leading risk factors for amputation. 2 Prevention and prompt diagnosis and treatment are necessary to prevent morbidity, especially amputation.
Can neuropathy cause ulcers on the foot?
Motor neuropathy can result in foot deformities (e.g., c law toe) that contribute to local pressure from footwear, making skin ulceration even more likely. Once the skin is broken (typically on the plantar surface), the underlying tissues are exposed to colonization by pathogenic organisms.
Abstract
Healthcare events related to diabetic foot disease carry a burden of morbidity, mortality and economic cost. Prompt identification of clinical infection with appropriate tissue sampling limits use of broad spectrum empirical antibiotics and improves antibiotic stewardship.
1 INTRODUCTION
Foot ulceration and infection continue to represent an important source of morbidity in people with diabetes mellitus. 1, 2 In an acute presentation with diabetic foot infection (DFI), there is frequently a delay in the identification of the causative organism, which may compel use of empirical antibiotic (s).
2 IDENTIFICATION OF DFI
Establishing presence of infection is an important component of ulcer care.
3 IMAGING IN THE DIAGNOSIS OF DFI
The sensitivity of plain X-ray in detecting osteomyelitis has been recorded at 54%, 29 but is much greater with serial plain X-ray. 43 The extent of deep tissue involvement including osteomyelitis may not be clinically apparent, even with the use of sterile metal probes and serial plain X-ray imaging.
4 DIAGNOSTIC MICROBIOLOGY IN DFI
Wound bioburden in the absence of clinical infection should not result in the initiation of antimicrobial therapy. 21, 25 However, it is accepted that culture results may be limited by culturing/sampling techniques and previous antibiotic exposure.
5 ANTIBIOTIC THERAPY: RISKS, BENEFITS AND COMPLICATIONS
Antibiotic therapy choice is influenced by efficacy, organism susceptibility and side effect profile. Any antibiotic may be associated with subsequent C. difficile infection (CDI), especially cephalosporins, clindamycin, co-amoxiclav, quinolones, piperacillin-tazobactam and carbapenems.
6 OUTPATIENT INTRAVENOUS ANTIBIOTIC THERAPY (OPAT)
Inevitably, a minority of patients with deep-seated diabetic foot infections will require prolonged IV therapy because of organism susceptibility or intolerance/failure of an otherwise appropriate oral regimen. In these circumstances and presuming suitability, OPAT can be considered.
Does G-CSF help with foot ulcers?
A Cochrane Database Systematic reviewupdated in 2013 concluded that treatment with G-CSF does notappear to increase the likelihood of resolution of infection or healingof the foot ulcer.177We found no relevant published studies on thistopic since this review. While G-CSF may reduce the need for surgicalinterventions, especially amputations, or the duration of hospitaliza-tion, it is not clear which patients might benefit, and G-CSF prepara-tions are not generally available and are expensive.
Can antibiotics be used for DFI?
While antibiotic therapy is necessary for DFIs, it is often not suffi-cient. Most patients with a DFI require some surgical treatment, rang-ing from minor bedside debridement or incision and drainage to majoroperative procedures, including resection of deep infected tissue,drainage of abscesses or infected compartments, resection of necroticor infected bone, or revascularization. While some of these proce-dures can be scheduled for convenience, a few require immediate sur-gery. The presence or severity of deep infection is often difficult toassess and may only be identified during surgery. While there is littlepublished evidence addressing this issue, we strongly believe the non-surgeon should consider when and how urgently to consult with asurgeon for most DFIs.
What are the principles of antimicrobial stewardship?
Principles of antimicrobial stewardship include limiting the duration ofantibiotic therapy for treating wounds to the minimum number ofdays needed for good results.139,140More prolonged antibiotic ther-apy is associated with increased risks of adverse events, greater dis-ruption of host microbiomes, higher costs, and more patient
What is the target of empiric antibiotic ther-apy?
For patients who have not recently received antibiotic therapy andwho reside in a temperate climate area, target empiric antibiotic ther-apy at just aerobic gram-positive pathogens (beta-haemolyticstrepto-cocciandS aureus) in cases of a mild DFI. (Strong; low)
What is empiric therapy for DFI?
Initial antibiotic therapy for most patients with a DFI will be empiric;the goal is to cover the likely pathogens without prescribing an unnec-essarily broad-spectrum regimen. Definitive therapy should then betailored to the clinical response to empiric therapy and the results ofproperly collected specimens. For decades, studies (almost exclusivelyfrom temperate climates in North America and Europe) consistentlydemonstrated that the most common pathogens in DFIs are aerobicgram-positivecocci, especiallyS aureus, and to a lesser extent strepto-cocciand coagulase-negative staphylococci. More recent studies ofDFIs from patients in tropical/subtropical climates (mainly Asia andnorthern Africa) have shown that aerobic gram-negativebacilli areoften isolated, either alone or in combination with gram-positivecocci.These considerations, along with whether or not the patient hasrecently received antibiotic therapy, has had gram-negative bacilli iso-lated from a recent previous culture, has had frequent exposure towater (a source forP aeruginosa), or comes from an environment inwhich pathogens are often resistant to commonly used antibiotics, arekey in selecting an empiric antibiotic regimen. Empiric treatmentaimed atP aeruginosa, which usually requires either an additional orbroader-spectrum agent, is generally unnecessary in temperate cli-mates. It should, however, be considered in tropical/subtropical cli-mates or ifP aeruginosahas been isolated from previous cultures ofthe affected patient. Of course, clinicians should reassess the regimenbased on the clinical response and culture and sensitivity results andconsider changing to more appropriate, safer, more convenient, or lessexpensive agent(s).
How long does it take for a diabetic foot to respond to parenteral therapy?
For diabetic foot osteomyelitis cases that initially require parenteraltherapy, consider switching to an oral antibiotic regimen that has highbioavailability after perhaps 5 to 7 days if the likely or proven patho-gens are susceptible to an available oral agent and the patient has noclinical condition precluding oral therapy. (Weak; moderate)
What test is used to diagnose osteomyelitis?
In a person with diabetes and suspected osteomyelitis of the foot, werecommend using a combination of the probe-to-bone (PTB) test, theESR (or CRP and/or PCT), and plain X-rays as the initial studies todiagnose osteomyelitis. (Strong; moderate)
Diagnosis
Pathophysiology
- Patients with diabetes are particularly susceptible to foot infection primarily because of neuropathy, vascular insufficiency, and diminished neutrophil function.3 Peripheral neuropathy has a central role in the development of a foot infection and it occurs in about 30 to 50 percent of patients with diabetes. Patients with diabetes lose the protective sensations for temperature an…
Cause
- Although most diabetic foot infections begin with an ulcer, localized cellulitis and necrotizing fasciitis can develop in the absence of an ulcer or traumatic injury. The most common pathogens in acute, previously untreated, superficial infected foot wounds in patients with diabetes are aerobic gram-positive bacteria, particularly Staphylococcus aureus and beta-hemolytic streptoc…
Treatment
- Early recognition of the area of involved tissue can facilitate appropriate management and prevent progression of the infection (Figure 3). The wound should be cleansed and debrided carefully to remove foreign bodies or necrotic material and should be probed with a sterile metal instrument to identify any sinus tracts, abscesses, or involvement of ...
Preparation
- Before an infected wound is cultured, any overlying necrotic debris should be removed by scrubbing the wound with saline-moistened sterile gauze to eliminate surface contamination.3,17 For wound culture, tissue specimens should be obtained by scraping the base of the ulcer with a scalpel or curette, or by a biopsy of the wound or bone. Needle aspiration of the pus or tissue flu…
Safety
- Touch, vibration, and pressure sensations should be checked routinely using cotton wool, tuning fork, and 10-g nylon monofilament, respectively.
Prevention
- Prevention of diabetic foot ulcers begins with identifying patients at risk. All patients with diabetes should have an annual foot examination that includes assessment for anatomic deformities, skin breaks, nail disorders, loss of protection sensation, diminished arterial supply, and inappropriate footwear. Patients at higher risk of foot ulceration should have examinations more often.39 Edu…
Literature
- 1. Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366(9498):17191724....