Therapy
Treatment for hyponatremia depends on the underlying cause and the severity of your symptoms. If you have mild symptoms, your doctor makes small adjustments to your therapy to correct the problem. This usually involves restricting water intake, adjusting medications and removing or treating the causes.
Self-care
- Hyponatremia is common and can be challenging to manage.
- Evaluation of the patient’s fluid status is important in determining the type of hyponatremia, which will direct the type of management required.
- Limited evidence exists for many of the interventions commonly used to treat hyponatremia.
Nutrition
So if someone with a fever drinks more water than necessary, water intoxication – or hyponatremia, a potentially fatal medical condition in which a patient’s blood sodium levels are too low – could follow. One study found that nearly a quarter of ...
Which specialist treats hyponatremia?
● Water restriction and salt replacement are the most important treatment modalities in hyponatremia. Mild hyponatremia does not require specific treatment. In patients with chronic hyponatremia, water restriction alone is usually effective.
What are the treatment guidelines for hyponatremia?
When to treat hyponatremia?
How to treat hyponatremia naturally?
What is the best treatment for hyponatremia?
TreatmentIntravenous fluids. Your doctor may recommend IV sodium solution to slowly raise the sodium levels in your blood. ... Medications. You may take medications to manage the signs and symptoms of hyponatremia, such as headaches, nausea and seizures.
What is the immediate treatment of hyponatremia?
Patients with chronic hyponatremia and severe symptoms (eg, severe confusion, coma, seizures) should receive hypertonic saline, but only enough to raise the serum sodium level by 4-6 mEq/L and to arrest seizure activity. After this, we recommend no further correction of the sodium for the first 24 hours.
What is the medication of choice for hyponatremia?
Medication Summary The primary treatments used in the management of hyponatremic patients rely on the use of intravenous sodium-containing fluids (normal saline or hypertonic saline) and fluid restriction. Less commonly, loop diuretics (eg, furosemide) or demeclocycline are used.
How do medical professionals treat a person with hyponatremia?
Treatment for hyponatremia depends on the underlying cause and the severity of your symptoms. If you have mild symptoms, your doctor makes small adjustments to your therapy to correct the problem. This usually involves restricting water intake, adjusting medications and removing or treating the causes.
What IV fluid is best for hyponatremia?
For serious symptomatic hyponatremia, the first line of treatment is prompt intravenous infusion of hypertonic saline, with a target increase of 6 mmol/L over 24 hours (not exceeding 12 mmol/L) and an additional 8 mmol/L during every 24 hours thereafter until the patient's serum sodium concentration reaches 130 mmol/L.
Do you treat hyponatremia with normal saline?
Our review did not reveal any head-to-head comparison trials of different methods or types of intravenous fluids for the treatment of hypovolemic hyponatremia. In practice, infusion with normal saline (9% sodium) is recommended to restore ECF volume by replacing both salt and free water.
Are diuretics used to treat hyponatremia?
In patients with hypervolemic hyponatremia, fluid and sodium restriction is the preferred treatment. Loop diuretics can be used in severe cases.
What medications increase sodium levels?
Drug Induced HypernatraemiaDiuretics.Sodium bicarbonate.Sodium chloride.Corticosteroids.Anabolic steroids.Adrenocorticotrophic steroids.Androgens.Oestrogens.
Do diuretics help hyponatremia?
Indeed, loop diuretics generally cause hypotonic renal losses and are used to treat euvolemic and hypervolemic hyponatremia.
How does D5W treat hyponatremia?
A brief infusion of 5 % dextrose in water (D5W) re-lowers the serum sodium to a more acceptable level, representing a 10-mmol / l increase in 24 h.
How do you treat low sodium in elderly?
Hyponatremia treatments may include changing a medication that affects your sodium level, treating the underlying disease, changing the amount of water you drink or changing the amount of salt in your diet.
What fluid order do you expect for the treatment of hyponatremia in a patient who is Normovolemic?
Acute normovolemic hyponatremia is treated by the intravenous administration of 3% NaCl and with the simultaneous use of loop diuretics (20- 40 mg Furosemide/ 24 hrs) and restriction of fluid intake.
How to treat hyponatremia?
If you have mild symptoms, your doctor makes small adjustments to your therapy to correct the problem. This usually involves restricting water intake, adjusting medications and removing or treating the causes.
What is the best medication for hyponatremia?
Certain newer medications, like tolvaptan (Samsca®), may be used to correct blood sodium levels. Treatment to correct any underlying medical problems – like congestive heart failure (when poor heart function causes fluid to build up in the body) – is also used to improve hyponatremia.
What is hyponatremia in labs?
What is hyponatremia? Hyponatremia is usually discovered on laboratory tests as a lower than normal sodium level in the blood. It will appear as sodium or Na+ in your lab results. Actually, the main problem in the vast number of situations is too much water that dilutes the Na+ value rather than too much sodium.
Why is hyponatremia a problem?
What causes hyponatremia? In general, too much water in your body is usually the main problem and this dilutes the sodium levels. Much less frequently, hyponatremia is due to significant sodium loss from your body. Too much water in your body causes your blood to become “watered down.”.
What happens if you have hyponatremia?
In many cases, hyponatremia causes extra water to move out of the bloodstream and into body cells, including brain cells. Severe hyponatremia causes this to occur quickly, resulting in swollen brain tissue. If left untreated, complications can include: 1 Mental status changes 2 Seizures 3 Coma 4 Death
Can you get hyponatremia after surgery?
Anyone can develop hyponatremia. Hyponatremia is more likely in people living with certain diseases, like kidney failure, congestive heart failure, and diseases affecting the lungs, liver or brain. It often occurs with pain after surgery.
Can you have hyponatremia if you have kidney disease?
If you have certain underlying medical conditions, particularly involving the kidneys, heart, lung, liver or brain, hyponatremia is more likely. You can lower your risk for hyponatremia by following your treatment plan and restricting your water intake to levels recommended by your doctor.
What is the first decision when faced with a patient with hyponatremia?
Intravenous fluids and water restriction. When faced with a patient with hyponatremia, the first decision is what type of fluid, if any, should be given. The treatment of hypertonic and pseudohyponatremia is directed at the underlying disorder in the absence of symptoms.
What is the first line of treatment for SIADH?
First-line treatment for patients with SIADH and moderate or profound hyponatremia should be fluid restriction; second-line treatments include increasing solute intake with 0.25–0.50 g/kg per day of urea or combined treatment with low-dose loop diuretics and oral sodium chloride.
What is isotonic saline used for?
Hypovolemic hyponatremia: Administer isotonic saline to patients who are hypovolemic to replace the contracted intravascular volume (thereby treating the cause of vasopressin release). Patients with hypovolemia secondary to diuretics may also need potassium repletion, which, like sodium, is osmotically active.
Is hyponatremia more likely to be corrected?
Acute hyponatremia (duration < 48 h) can be safely corrected more quickly than chronic hyponatremia. A severely symptomatic patient with acute hyponatremia is in danger from brain edema. In contrast, a symptomatic patient with chronic hyponatremia is more at risk from rapid correction of hyponatremia.
Does conivaptan help with heart failure?
It is effective in raising serum sodium levels; however, conivaptan has not been shown to improve heart failure per se. Close monitoring of the rate of correction is needed.
Is V2 antagonist used for normovolemic patients?
The use of a V2 receptor antagonist may be considered (see below). For normovolemic (euvolemic), asymptomatic hyponatremic patients, free water restriction (< 1 L/d) is generally the treatment of choice. There is no role for hypertonic saline in these patients.
Can aquaretics be treated with saline?
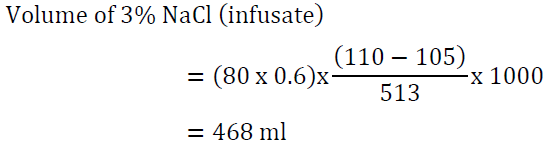
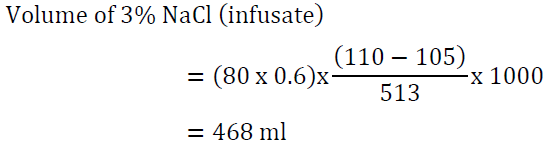
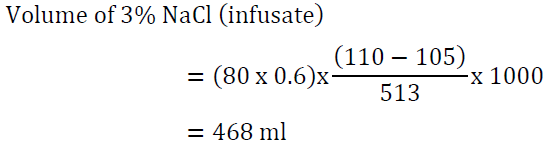
There is no place in the initial treatment for aquaretics (see below). Note that normal saline can exacerbate hyponatremia in patients with SIADH, who may excrete the sodium and retain the water. A liter of normal (0.9%) saline contains 154 mEq sodium chloride (NaCl) and 3% saline has 513 mEq NaCl.
How to treat hyponatremia?
7 Treatment of severe hyponatremia should take place in a critical care setting with isotonic or hypertonic fluids and frequent monitoring of serum sodium in order to ensure a safe rate of sodium correction. 1,7 Treatment of mild-to-moderate hyponatremia should focus on treating the underlying cause, and further therapy considerations are dependent on the etiology.
What is the first line of treatment for hypervolemic hyponatremia?
Hypervolemic Hyponatremia: In the treatment of hypervolemic hyponatremia, water restriction is recommended as first-line therapy. Other therapies include diuretic therapy with furosemide, sodium restriction, or initiation of vaptan therapy.
What is the role of pharmacists in SIADH?
Pharmacists also play an important role in recognizing which drugs cause euvolemic hyponatremia induced by SIADH (see TABLE 1 ). 14-17 Management of drug-induced SIADH involves removal of the offending agent and providing supportive care based on the severity of hyponatremia.
How does hyponatremia affect schizophrenia?
Hyponatremia is seen in about 4% of patients with chronic schizophrenia and occasionally in patients with other psychiatric disorders. 2 Primary polydipsia is prominent in patients with psychosis, affecting nearly 7% of patients with schizophrenia. In addition to the underlying psychosis, psychotropic drugs may cause the sensation of a dry mouth, which may contribute to increased water intake. 8 Thus, causality between psychotropic agents and hyponatremia has been shown more persuasively with antidepressants and mainly with selective serotonin reuptake inhibitors (SSRIs). The incidence of hyponatremia caused by SSRIs varies widely, from 0.5% to 32%. 4 In the majority of cases, hyponatremia occurs within the first few weeks of the onset of therapy, whereas normonatremia is achieved within 2 weeks after drug withdrawal. 4
What is the treatment for psychogenic polydipsia?
Current treatment of psychogenic polydipsia includes reducing fluid intake, behavioral modification, and pharmacologic therapy in an attempt to decrease thirst. 6.
How long does it take for thiazide to cause hyponatremia?
Thiazide-induced hyponatremia occurs most frequently in elderly woman and usually develops within 2 weeks of therapy initiation. 16 Thiazide diuretics cause hyponatremia by blocking sodium reabsorption in the distal tubule and causing proportionally more sodium loss than water.
What is hypotonic hyponatremia?
Hyponatremia presents as hypertonic or hypotonic; however, only hypotonic hyponatremia is of clinical relevance. Hypertonic hyponatremia is often due to a laboratory error caused by marked elevations of lipids or plasma proteins (pseudohyponatremia) or to a marked increase in plasma glucose. 6 Hypotonic hyponatremia is categorized by severity and volume status. Severity of hyponatremia is classified as acute or chronic, differentiated by sodium levels and patient symptoms. 7 Mild-to-moderate hyponatremia is a more chronic and asymptomatic condition and is defined as a sodium concentration of 120 to 135 mEq/L. 7 Severe hyponatremia is a medical emergency and is usually defined as a sodium concentration of <120 mEq/L or hyponatremia with symptoms that may include seizures, coma, and respiratory arrest. 7
What drugs are used to treat hyponatremia?
Newer agents like tolvaptan and conivaptan, which are vasopressin receptor antagonists, block the action of vasopressin in the kidneys and help excrete water load, thus improving hyponatremia. However safety and long term effects of these drugs in older adults have not been well established, and thus should be used with caution.
What is the first step in managing hyponatremia?
The initial step in the managing hyponatremia involves elucidating the cause, and reversing that cause if possible. Isotonic saline and diuretics must be used with caution in older adults; requires careful inpatient monitoring to avoid fluid overload. Correction of serum sodium depends on how long hyponatremia has been present.
What causes hyponatremia in older adults?
If the patient is hypovolemic on exam, hyponatremia is typically caused by gastrointestinal fluid losses, pancreatitis, third spacing, or insensible losses. Intravenous fluid replacement is the mainstay of treatment, but in institutionalized older adults, where vascular access is an issue, subcutaneous infusions may be useful.
What is hypotonic hyponatremia?
Hypotonic hyponatremia with decreased urine osmolality is classically seen in patients with psychogenic polydipsia and beer potomania. But, it also occurs in older adults who have difficulty preparing foods and gradually cut back on food variety until they are eating a simple "tea and toast" diet, which contains inadequate sodium.
How long does it take for hyponatremia to be corrected?
Long-standing hyponatremia without severe symptoms must be corrected more slowly - not more than 6mEq/L in 24 hours to avoid osmotic demyelination syndrome. The diagnostic evaluation of hyponatremia in older adults ...
What causes euvolemic patients?
If the patient is euvolemic, likely causes include the syndrome of inappropriate antidiuresis (SIAD), hypothyroidism, and glucocorticoid insufficiency.
Can diuretics cause volume depletion?
Diuretics are used to correct hyponatremia in these cases, but they risk causing volume depletion in older adults - so the dose of diuretics should be carefully managed based on clinical response.
How do angiotensin-converting enzyme inhibitors help with hyponatremia?
In addition, angiotensin-converting enzyme inhibitors can improve hyponatremia in CHF by reducing ADH levels and improving cardiac output via afterload reduction. There has been recent interest in the use of vasopressin V2 receptor antagonists or “vaptans.”.
What causes hyponatremia with normal osmolarity?
Hyponatremia with normal osmolarity can be caused by pseudohyponatremia (i.e., hyperglycemia, paraproteinemia, hyperlipidemia), severe renal failure, ingestion of excess alcohol, or post-transurethral resection of prostate or bladder.
What is hypertonic saline?
Use hypertonic saline for severe symptomatic hyponatremia. Hyponatremia with high pOSM occurs as a result of elevated levels of an extra solute in the plasma that does not readily enter cells. This draws water into the extracellular fluid and lowers the sodium concentration.
What is the disorder of excess body water in relation to sodium?
Hyponatremia , a disorder of excess total body water in relation to sodium, occurs in up to 42% of hospitalized patients. 1,2 Regardless of the cause, hyponatremia is usually associated with the syndrome of inappropriate antidiuretic hormone secretion (SIADH) or with the appropriate elevation of antidiuretic hormone (ADH), known as hypovolemia. ADH is produced in the hypothalamus and released in the posterior pituitary in response to increasing plasma osmolarity (pOSM) or effective circulating volume depletion. ADH acts in the cortical collecting duct to increase the number of luminal aquaporin channels, increasing water reabsorption and decreasing plasma osmolarity. When hyponatremia is severe, the movement of water into cells causes cellular brain swelling, and clinical symptoms progress from malaise, headache, and nausea to obtundation, seizures, or respiratory arrest (see Figure 1). Even mild, chronic hyponatremia (120-131 mEq/L) is associated with an increased risk of falls due to mild gait and attention impairment. 3
What is the normal sodium level?
Normal serum sodium levels are between approximately 135 and 145 mEq/L. Hyponatremia is generally defined as a serum level of less than 135 mEq/L. Shown on the left is a normal brain. On the right, serum sodium ion level is less than 130 mEq/L and water is drawn into the cells, causing the brain to swell.
How often should you check serum sodium?
The best way to avoid overly rapid correction is to check serum sodium every two hours and monitor urine output closely.
Can hyponatremia cause hypoosmolarity?
Hyponatremia with normal osmolarity can be caused by pseudohyponatremia (i.e., hyperglycemia, paraproteinemia, hyperlipidemia), severe renal failure, ingestion of excess alcohol, ...
What is hyponatremia in blood?
WHAT YOU NEED TO KNOW: Hyponatremia occurs when the amount of sodium (salt) in your blood is lower than normal. Sodium is an electrolyte (mineral) that helps your muscles, heart, and digestive system work properly. It helps control blood pressure and fluid balance.
What foods have high sodium?
Foods that are high in sodium include milk, packaged snacks such as pretzels, or processed meats (bacon, sausage, and ham). Ask your dietitian to help you create a meal plan that is right for you.
How to treat hyponatremia?
1. Treat neurologic emergencies related to hyponatremia with hypertonic saline. 2. Defend the intravascular volume. 3. Prevent worsening hyponatremia. 4. Prevent rapid overcorrection with the Rule of 100s. 5.
How long does it take to correct hyponatremia?
The rule of 6s can be helpful in guiding your correction of hyponatremia. “Six in six hours for severe symptoms and then stop” implies that if you need to rapidly increase serum sodium due to a neurologic emergency do not correct more than 6mmol.
Why do endurance athletes have hyponatremia?
EAH is most commonly seen among endurance athletes. Their hyponatremia is a result of ingesting more free water than they are able to clear by voiding. This leads to an overall excess of free water as the kidneys are not able to excrete it.
What are the symptoms of hyponatremia?
The lower the sodium and the faster the fall, the more symptomatic a patient will become. Symptoms are often vague and non-specific presenting as headache, irritability, lethargy, confusion, agitation or unstable gait leading to a fall .
What is the most common fluid and electrolyte disorder?
Hyponatremia is the most common fluid and electrolyte disorder encountered in clinical practice and is found in approximately 20% of admissions to hospital. In addition to being extremely prevalent, hyponatremia is an independent predictor of mortality.