Medication
Both types have similar signs and symptoms: Acute paronychia: Symptoms of acute paronychia appear over hours or a few days. The infection is only in the nail fold and doesn’t extend deeper inside the finger or toe. Symptoms go away with treatment and last less than six weeks.
Procedures
(Although antibiotics are commonly prescribed,most patients do not require antibiotics for a simple paronychia.) ... The initial treatment of chronic paronychia consists of the avoidance of inciting factors such as exposure to moist environments or skin irritants.
Self-care
Surgical management of chronic paronychia Surgical management is only indicated in recalcitrant cases of chronic paronychia, which does not respond to medical management and proper use of general measures.
How long does it take for paronychia to go away?
Acute paronychia. Cleocin and Augmentin also have anaerobic activity; therefore, they are useful in treating patients with paronychia due to oral anaerobes contracted through nail biting or finger sucking. Cleocin should be used instead of Augmentin in patients who are allergic to penicillin.
Do you need antibiotics for paronychia?
When is surgery indicated for the treatment of chronic paronychia?
Can Cleocin be used to treat acute paronychia?

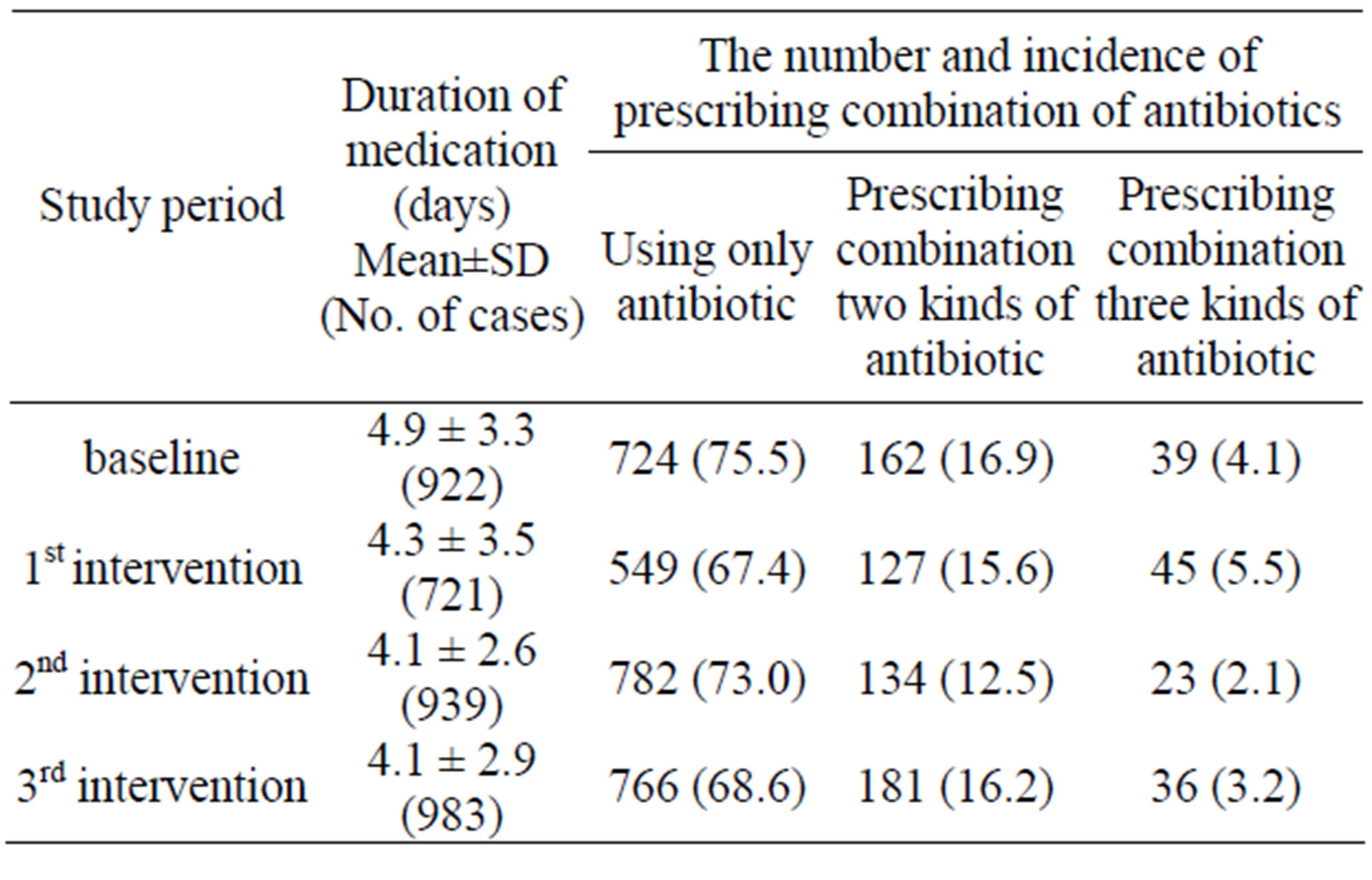
How long do you take antibiotics for paronychia?
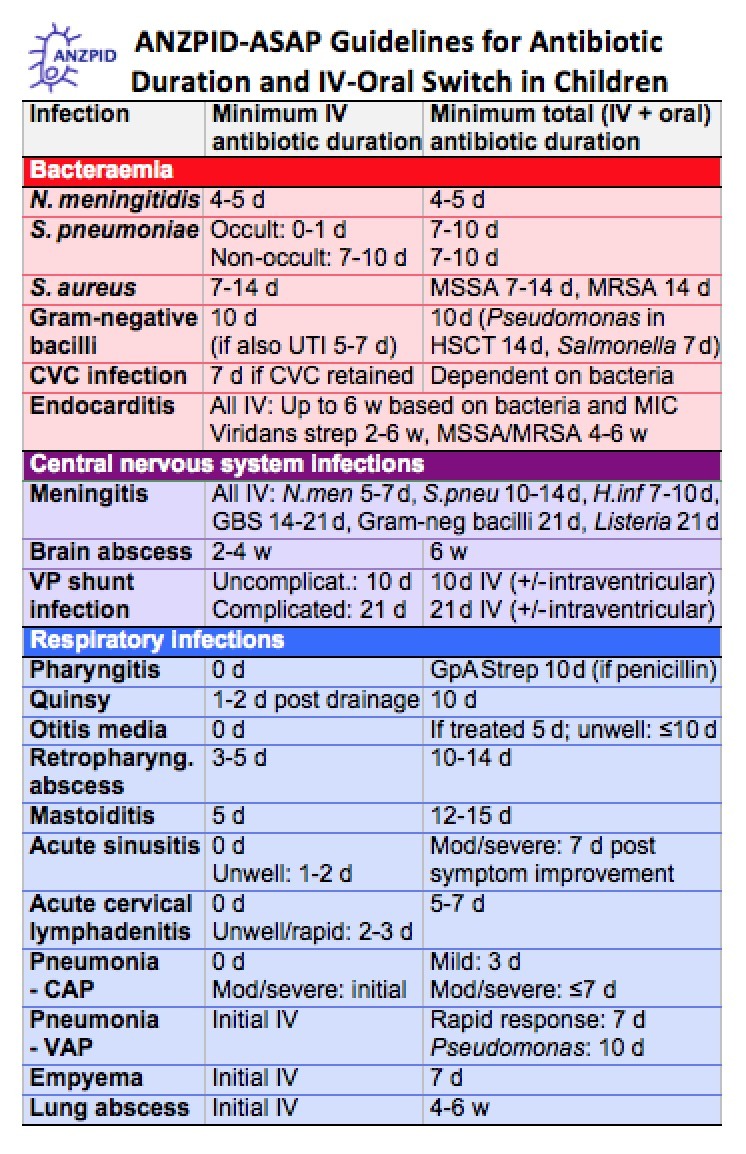
The patient should receive oral antibiotics for 5-7 days. The packing is removed after 2 days, and warm sodium chloride solution soaks are begun. The most simple and, often, least painful incision can be made without anesthesia, using only an 18-gauge needle.
Will antibiotics cure paronychia?
Paronychia is typically treated with antibiotics, although milder acute cases can often resolve on their own without treatment. The antibiotics most commonly used to treat paronychia are Bactrim (TMP/SMX) and a cephalosporin named Keflex (cephalexin).
What antibiotics are used to treat paronychia?
Oral antibiotics with gram-positive coverage against S aureus, such as amoxicillin and clavulanic acid (Augmentin), clindamycin (Cleocin), or or cephalexin, are usually administered concomitantly with warm water soaks.
How long does it take for paronychia swelling to go down?
If you have acute paronychia, soaking the infected nail in warm water 3 to 4 times a day can help reduce pain and swelling. It should heal up in a few days. If the infection is very painful, doesn't get better with home care, or has a pus-filled abscess, you may need to see your doctor.
What is the fastest way to cure paronychia?
Management and Treatment You may be able to treat mild cases of paronychia at home. Soak the infected area in warm water for about 15 minutes a few times a day. Be sure to dry the area thoroughly. Soaking the cuticle and nailbed helps pus drain from under the skin.
Which antibiotic is best for nail infection?
Penicillin and its derivatives such as ampicillin are the most effective antibiotics in nail infection, especially if caused by biting the nails or sucking the fingers.
How do I know if my paronychia is getting better?
The first signs that your fingertip is getting better will be that the sharpness of the pain will decrease (the pain will not entirely go away, but the worst of it will go down, and you will be able to think of something besides your painful finger) and the sharpness of the redness will decrease (the redness will not ...
Do you need oral antibiotics for paronychia?
Paronychia is an inflammation of the folds of tissue surrounding the nail of a toe or finger....SORT: KEY RECOMMENDATIONS FOR PRACTICE.Clinical recommendationEvidence ratingReferencesThere is no evidence that treatment with oral antibiotics is any better or worse than incision and drainage for acute paronychia.C233 more rows•Feb 1, 2008
Will antibiotics cure a finger infection?
It causes pain, swelling and redness. If not treated immediately, a pus-filled sac (abscess) can form. Early-stage felon finger infections can usually be treated with antibiotics.
How do I know if paronychia needs to be drained?
Paronychia drainage is recommended when an abscess forms within the nail folds or beneath the nail plate.
Should you keep paronychia covered?
Wash the area with clean water 2 times a day. Don't use hydrogen peroxide or alcohol, which can slow healing. You may cover the area with a thin layer of petroleum jelly, such as Vaseline, and a non-stick bandage.
Can you put ice on paronychia?
For swelling, ice the area and elevate the injured area above the heart.
How long should you follow up with a doctor for paronychia?
The patient should follow up with a provider in the next 24 to 48 hours to ensure drainage and to look for signs of worsening infection. Usually, incision and drainage is the adequate treatment of acute paronychia; however, if there is a significant extension of cellulitis, oral antibiotics may be prescribed as above.
How long does paronychia last?
The classification of paronychia is according to the clinical presentation: Acute paronychia - Lasting less than six weeks, painful and purulent condition; most frequently caused by a bacterial infection, especially staphylococci.
What causes paronychia in the cuticle?
Paronychia results from the disruption of the protective barrier between the nail and the nail fold, which is the cuticle. Trauma (including manicures and pedicures), infections (including bacterial, viral, and fungal), structural abnormalities, and inflammatory diseases (ex. psoriasis) are predisposing factors.
What is Paronychia level V?
[Level V] In most cases, the clinician (physician, NP, PA) will diagnose and prescribe treatment.
What is the pain of a paronychia?
Paronychia is most commonly an acute inflammatory process causing painful redness and swelling to the lateral nail fold and is primarily diagnosed based on clinical presentation. The patient will usually present within the first few days of infection due to the pain.
What is the differential diagnosis of paronychia?
Differential diagnosis of paronychia include: 1- Cellulitis - Cellulitis is a superficial infection and will present as erythema and swelling to the affected portion of the body with no area of fluctuance. Treatment is with oral antibiotics.
How to treat paronychias?
Paronychias are usually either treated with incision and drainage or antibiotics. If there is inflammation with no definite abscess, treatment can include warm soaks with water or antiseptic solutions (chlorhexidine, povidone-iodine) and antibiotics. Warm soaks should be for 10 to 15 minutes, multiple times a day.
How to treat an infected fingernail?
1. Protect Nail. Do not remove any part of the nail. If an artificial nail is on an infected finger, remove it. 2. Reduce Pain and Swelling. For mild nail infection or while waiting to see a doctor:
What to do if you have a pus pocket?
In chronic cases of paronychia, your doctor may prescribe an anti-fungal topical. If a pus-filled abscess pocket develops, a doctor may need to drain it.
What is the treatment for paronychia?
The initial medical treatment consists of the application of topical antifungal agents. Topical miconazole may be used as the initial agent. Oral ketoconazole or fluconazole may be added in more severe cases.
What to do if paronychia does not resolve?
If paronychia does not resolve despite best medical efforts, surgical intervention may be indicated. Also, if an abscess has developed, incision and drainage must be performed (see the image below). Surgical debridement may be required if fulminant infection is present. Paronychia incision and drainage.
Why do immunocompromised patients need more aggressive treatment?
Patients with diabetes and those who are immunocompromised need more aggressive treatment because the response to therapy is slower in these patients than in others. In cases induced by retinoids or protease inhibitors, the paronychia usually resolves if the medication is discontinued. Previous.
What antibiotics are used to treat S aureus?
Oral antibiotics with gram-positive coverage against S aureus, such as amoxicillin and clavulanic acid (Augmentin), clindamycin (Cleocin), or or cephalexin, are usually administered concomitantly with warm water soaks.
Why is there no excision of the paronychia?
Often, no excision of any tissues is made, because only blunt dissection and separation are needed to evacuate the pus from the paronychia. The wound should be well irrigated with isotonic sodium chloride solution, and plain gauze packing should be inserted under the fold to keep the cavity open and allow drainage.
Where is the needle inserted in a paronychia?
The technique is performed as follows: The needle is positioned bevel up and laid horizontally on the nail surface; it is inserted at the lateral nail fold where it meets the nail itself, at the point of maximum fluctuance. The skin of the nail fold is lifted, releasing pus from the paronychia cavity.
What to do if an abscess has developed?
If an abscess has developed, however, incision and drainage must be performed. Surgical debridement may be required if fulminant infection is present. [ 39, 40] Herpetic whitlow and paronychia must be distinguished because the treatments are drastically different. Misdiagnosis and mistreatment may do more harm than good.
How long does paronychia last?
Chronic paronychia is an inflammatory recalcitrant disorder affecting the nail folds. It can be defined as an inflammation lasting for more than 6 weeks and involving one or more of the three nail folds (one proximal and two lateral).[1] .
What drugs cause chronic paronychia?
Drug toxicity from medications such as retinoids, epidermal growth factor-receptor inhibitors (cetuximab), and protease inhibitors. Indinavir- induces retinoid-like effects and remains the most frequent cause of chronic paronychia in patients with HIV disease. Retinoids also induce chronic paronychia.
What causes paronychia?
There are many rare causes of chronic paronychia, which should always be kept in mind and some of which include the following: 1 Infections (Bacterial, mycobacterial, or viral) 2 Raynaud's disease 3 Metastatic cancer, subungual melanoma, squamous cell carcinoma. Benign and malignant neoplasms should always be excluded when chronic paronychia does not respond to conventional treatment 4 Papulosquamous disorders like psoriasis, vesicobullous disorders-pemphigus 5 Drug toxicity from medications such as retinoids, epidermal growth factor-receptor inhibitors (cetuximab), and protease inhibitors. Indinavir- induces retinoid-like effects and remains the most frequent cause of chronic paronychia in patients with HIV disease. Retinoids also induce chronic paronychia. The mechanism can be -nail fragility and minor trauma by small nail fragments.[10] Paronychia has also been reported in patients taking cetuximab (Erbitux), an anti-epidermal growth factor-receptor (EGFR) antibody used in the treatment of solid tumors.[11]
What is the differential diagnosis of chronic paronychia?
The differential diagnosis of chronic paronychia includes squamous cell carcinoma of the nail, malignant melanoma, metastases from malignant tumors. The clinician should consider the possibility of the carcinoma when a chronic inflammatory process is unresponsive to treatment.
Is paronychia a dermatitis?
Previously, it was believed that chronic paronychia is caused by Candida.[6] . However, recent data reveals that it is a form of hand dermatitis caused by environmental exposure. Candidais often isolated; however, in many cases, Candidadisappears when the physiologic barrier is restored.[7] .
Is paronychia a mycotic disease?
Hence, the recent view holds that chronic paronychia is not a mycotic disease but an ecze matous condition with a multifactorial etiology. For this reason, topical and systemic steroids may be used successfully, whereas systemic anti-fungals are of little value.
How long does paronychia last?
The nail fold is the skin around your nail. Paronychia may happen suddenly and last for 6 weeks or longer. You may have paronychia on more than 1 finger or toe.
What are some examples of paronychia?
Some examples are skin cancer, psoriasis, HIV, and lupus. Chemicals: Contact with soaps, detergents, and other chemicals can cause inflammation and lead to paronychia. Allergies: Allergies to certain foods, nail polish, or latex can cause inflammation and increase your risk.
What is the best medicine for fungus?
Antifungal medicine: This medicine helps kill fungus that may be causing your infection. It may be given as a cream or ointment. NSAIDs: These medicines decrease pain and swelling. NSAIDs are available without a doctor's order. Ask your healthcare provider which medicine is right for you.
What is the mechanism of action of antifungal agents?
The mechanism of action of antifungal agents usually involves the alteration of the permeability of the cell membrane (polyenes) of the fungal cell or the inhibition of pathways (en zymes, substrates, transport) necessary for sterol/cell membrane synthesis.
What is clindamycin used for?
Clindamycin (Cleocin) View full drug information. This agent is a lincosamide used in the treatment of serious skin and soft tissue staphylococcal infections. It is also effective against aerobic and anaerobic streptococci (except enterococci).
What is the action of imidazole?
An imidazole with broad-spectrum antifungal action, it inhibits the synthesis of ergosterol, causing cellular components to leak and resulting in fungal cell death. This is a synthetic fungistatic triazole that inhibits cytochrome P-450–dependent synthesis of ergosterol, a vital component of fungal cell membranes.
Where is clindamycin excreted?
Clindamycin widely distributes in the body without penetration of the central nervous system (CNS). It is protein bound and excreted by the liver and kidneys. Amoxicillin and clavulanic acid (Augmentin, Augmentin XR, Amoclan) View full drug information.
Does penicillin cover staph?
Although penicillin covers oral flora, it does not cover methicillin-resistant Staphylococcus aureus (MRSA). Trimethoprim and sulfamethoxazole (TMP/SMZ), doxycycline, or clindamycin may be considered to cover community-acquired MRSA and anaerobic organisms. Cephalexin may also be effective.
Is cephalexin effective against staphylococcus?
Cephalexin may also be effective. Combination therapy with an intravenous agent that provides antimicrobial activity against staphylococci is used for inpatient therapy. Chronic paronychial infections are usually managed with oral antifungals such as ketoconazole, itraconazole, or fluconazole. [ 43] .