
Explore
Ringworm, also known as tinea corporis) is a contagious infection of the skin caused by a fungus. The infection starts as a rash with tiny red pimples. The pimples slowly spread and form a round or oval ring. A single patch of ringworm can be treated …
How do I choose the best tinea cruris treatment?
Oral antifungal treatment is usually required if tinea corporis is involving a hair-bearing site, is extensive, or has failed to clear with topical antifungals. Systemic therapy is also required for Majocchi granuloma and tinea imbricate.
What is the remedy for tinea cruris?
May 16, 2018 · Clotrimazole: apply 2-3 times a day for at least four weeks. Miconazole: apply twice a day and continue for 10 days after the skin is back to normal. Econazole: apply twice a day until the skin is back to normal. Ketoconazole: apply once or twice a day and continue for a few days after the skin is back to normal.
Does tinea cruris take time to cure?
The treatment of tinea corporis is mostly through topical therapy as dermatophyte infection seldom reaches the deeper tissues of the body. It is mostly superficial that topical anti-fungal is enough to treat this skin condition.
How to treat tinea cruris at home?
76 rows · Tinea corporis is an infection of the body surface with mold-like fungi called dermatophytes. Drugs used to treat Tinea Corporis The following list of medications are in some way related to or used in the treatment of this condition. Rx OTC Off-label Only Generics 1 2 3 4 Next View all results on one page Frequently asked questions
What is the best treatment for tinea corporis?
Among various options, topical terbinafine for 4 weeks appears to be the treatment of choice for limited disease (tinea corporis/cruris/pedis). For more extensive disease, the choice is less clear. Both terbinafine (250–500 mg/day for 2–6 weeks) and itraconazole (100–200 mg/day for 2–4 weeks) appear to be effective.
Which cream is best for tinea corporis?
Drugs used to treat Tinea CorporisDrug nameRatingRx/OTCView information about Nizoral Topical Nizoral Topical10Rx/OTCGeneric name: ketoconazole topical Drug class: topical antifungals For consumers: dosage, side effectsView information about tolnaftate tolnaftate9.0Rx/OTC72 more rows
Which antifungal is best for tinea corporis?
Limited disease – Tinea corporis usually responds well to topical antifungal drugs, such as azoles, allylamines, butenafine, ciclopirox, tolnaftate, and amorolfine (table 1) [16,32].May 27, 2021
What is tinea corporis caused by?
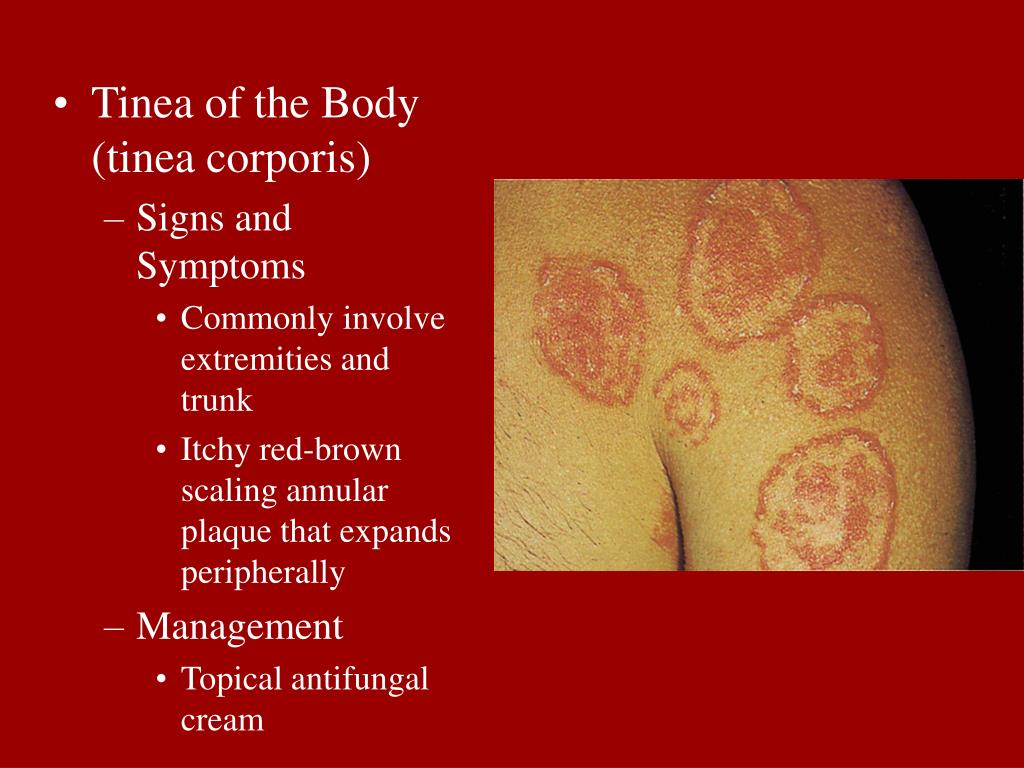
Ringworm of the body (tinea corporis) is a rash caused by a fungal infection. It's usually an itchy, circular rash with clearer skin in the middle. Ringworm gets its name because of its appearance.Sep 24, 2021
What causes tinea faciei?
The same fungus that causes tinea corporis (a body infection) causes tinea faciei. All tinea infections are spread from contact with infected people (children commonly spread tinea from one to another), infected animals, or contaminated personal objects such as towels.
What does tinea look like?
When fungus affects the skin of the body, it often produces itchy, red, raised, scaly patches that may blister and ooze. The patches often have sharply defined edges. They are often redder around the outside with normal skin tone in the center, creating the appearance of a ring.
How do I get rid of tinea corporis permanently?
Over-the-counter antifungals can kill the fungus and promote healing. Effective medications include miconazole (Cruex), clotrimazole (Desenex) and terbinafine (Lamisil). After cleaning the rash, apply a thin layer of antifungal medication to the affected area 2 to 3 times per day or as directed by the package.
How long does tinea take to heal?
Most mild cases of ringworm usually clear up in 2 to 4 weeks. But treatment might be needed for up to 3 months if the infection is more serious, or affects the nails or the scalp.
What gets rid of tinea faciei?
Most cases of tinea faciei are curable with topical antifungal agents. If a topical steroid has been applied, fungal folliculitis may be present. Fungal folliculitis requires systemic therapy. The frequency of daily application and duration of the treatment depend on the active ingredients of the preparation.Apr 9, 2021
How do you catch tinea corporis?
While it's most commonly spread from skin-to-skin contact, you can also catch it from touching something that someone with ringworm touched. To prevent ringworm, you should keep your skin clean and dry. Immediately after the gym or shower, put on clean, dry clothes. Avoid physical contact with someone who has ringworm.
Does tinea corporis go away on its own?
Without treatment, it may go away on its own in a matter of months in a healthy person. Or it may not. Ringworm on the body is usually treated with a topical ointment such as terbinafine.
What are the symptoms of tinea corporis?
Symptoms of body ringworm (tinea corporis) may include: Red, ring-shaped patches with raised, scaly edges. Itching....What are the symptoms of tinea infection?Itchy, burning rash on the feet.Whitening and breakdown of the skin between the toes.Scaling of the feet.Blisters on the feet.
How to treat ringworm on hands?
Apply a thin layer of cream just past the outside edges of the rash. Spread the cream, beginning from the outside area first, then move toward the center of the rash (Picture 1). Do not cover the ringworm with a bandage. Wash and dry your hands well.
How long does ringworm last?
If there are many patchy areas, the doctor may prescribe a stronger medicine. Ringworm usually goes away within 4 weeks of treatment.
How to prevent ringworm from spreading?
To prevent ringworm from spreading to others: Keep the skin clean and dry. Dry the skin well after washing or bathing. Wash hands well and right away if a ringworm rash is touched.
What is ringworm in the body?
Ringworm of the body (tin ee uh COR por is) is an infection of the skin caused by a fungus (a plant which is too small to see). Ringworm is not caused by a worm. The infection starts as a rash with tiny red pimples. The pimples slowly spread and form a round or oval ring, typically ½ to 1 inch (12 to 25 mm) in size.
What is the best treatment for tinea corporis?
Oral antifungal treatment is usually required if tinea corporis is involving a hair-bearing site, is extensive, or has failed to clear with topical antifungals. Systemic therapy is also required for Majocchi granuloma and tinea imbricate. Recommended oral agents are terbinafine and itraconazole.
What is Majocchi Granuloma?
Majocchi granuloma — a variant involving the hair follicles and subcutaneous tissue, most commonly found on the limbs after shaving. It presents as perifollicular papules or pustules. T. rubrum is the usual organism. Bullous tinea corporis — a rare variant presenting with vesicles or blisters.
What are the clinical variants of tinea corporis?
Clinical variants of tinea corporis. Clinical variants of tinea corporis can include the following types. Kerion — an intense pustular inflammatory reaction due to zoophilic fungi. Tinea gladiatorum — affects participants in contact sports such as wrestling or martial arts due to skin-to-skin contact.
What causes tinea corporis?
Tinea corporis is predominantly caused by dermatophyte fungi of the genera Trichophyton and Microsporum. The anthropophilic species T. rubrum is the most common causative agent of tinea corporis worldwide including New Zealand.
How is tinea corporis spread?
Tinea corporis is spread by the shedding of fungal spores from infected skin. Transmission is facilitated by a warm, moist environment and the sharing of fomites including bedding, towels, and clothing. Dermatophyte infection elsewhere on the skin, such as tinea pedis, can also be transferred.
How long does tinea corporis last?
Application needs to include an adequate margin around the lesion and a prolonged course continuing for at least 1–2 weeks after the visible rash has cleared. However, recurrence is common.
What is the secondary type of tinea corporis?
T. tonsurans — secondary to tinea capitis or skin-to-skin contact. M. canis (cats, dogs), and less commonly other zoonotic species including T. verrucosum (cattle), T. equinum (horses) and T. erinacei (hedgehogs). Tinea corporis is spread by the shedding of fungal spores from infected skin.
What is the treatment for tinea corporis?
Systemic therapy may be indicated for tinea corporis that includes extensive skin infection, immunosuppression, resistance to topical antifungal therapy, and comorbidities of tinea capitis or tinea unguium. Use of oral agents requires attention to potential drug interactions and monitoring for adverse effects.
Why does tinea corporis recur?
The tinea corporis may recur if therapy does not result in complete eradication of the organism, such as when patients stop applying topical therapy too soon or if the organism is resistant to the antifungal agent used. Reinfection may occur if a reservoir, such as an infected nail or hair follicle, is present.
What is the best treatment for tinea imbricata?
If there is no improvement, other dermatoses can be considered. The preferred treatment for tinea imbricata is griseofulvin or terbinafine, although some resistance has developed to oral griseofulvin. [ 37] . Botanical extracts appear promising.
How long does terbinafine last?
Oral terbinafine may be used at a dosage of 250 mg/d for 2 weeks; the potential exists for cytochrome P-450, specifically CYP-2D6, drug interactions with this agent. Systemic therapy is needed when the infection involves hair follicles, such as Majocchi granuloma.
Can topical steroid be used for tinea incognito?
In this case, topical therapy may serve as adjunct treatment with the oral medication. For severe cases of tinea incognito, oral antifungal treatment may be necessary. Important to note is that if the clinician suspects a dermatophyte infection, a topical steroid should not be prescribed.
Can tinea corporis be reinfected?
Reinfection may occur if a reservoir, such as an infected nail or hair follicle, is present. Many, if not most, adult patients with tinea corporis also have tinea pedi s and unguium, which should be treated. Id reaction. Dermatitis caused by exogenous agents initially arises at the site of contact.
What is the name of the fungus that infects the skin?
There are many types of fungal germs (fungi) and some can infect the skin, nails, and hair. Fungal infections are also known as 'tinea' or 'dermatophyte infections' or 'dermatophytosis'. This leaflet just deals with ringworm of the skin (sometimes called tinea corporis). See also the separate leaflets called Fungal Scalp Infection (Scalp Ringworm), ...
What is ringworm?
Ringworm Tinea Corporis. Ringworm. Ringworm is a skin infection caused by a fungus. It is not caused by worms, and there are no worms involved, despite the name! Treatment with an antifungal cream usually works well.
Where can I buy antifungal cream?
You can buy an antifungal cream from pharmacies, or get one on prescription. There are various types and brands - for example, terbinafine, clotrimazole, econazole, ketoconazole and miconazole. These are good at clearing fungal skin infections. There is no evidence that any one cream is better than any other one.
How to prevent fungus from spreading?
To prevent passing on the infection, do not share towels. Wash towels, sheets and clothes frequently. Clean your shower or bath well after use. Try not to scratch the rash, as this may spread the fungus to other areas of your body. You do not need to stay off work or school once treatment has started.
How often should I take ketoconazole?
Econazole: apply twice a day until the skin is back to normal. Ketoconazole: apply once or twice a day and continue for a few days after the skin is back to normal. Cannot be used for children. Terbinafine: apply once or twice a day for one to two weeks. Cannot be used for children.
How long should I use clotrimazole cream?
This varies between the different creams, so read the instructions carefully. Briefly: Clotrimazole: apply 2-3 times a day for at least four weeks. Miconazole: apply twice a day and continue for 10 days after the skin is back to normal.
How to describe ringworm?
From person to person by touching a person who has the infection. From touching items which have been in contact with an infected person. For example, towels, clothes, bed linen or chairs which have been used by somebody who has ringworm. From animals.
How to treat tinea corporis?
The treatment of tinea corporis is mostly through topical therapy as dermatophyte infection seldom reaches the deeper tissues of the body. It is mostly superficial that topical anti-fungal is enough to treat this skin condition. The anti-fungal cream is usually applied twice a day for a period of two weeks or depending on ...
What causes tinea corporis?
Trichophyton rubrum is among the most common cause of tinea corporis. It is regarded as one of the most common causes of dermatophytosis globally. T. rubrum mostly infect the areas between the toes and the feet and between the fingernails. It is the causative agent for jock itch, athlete’s foot and ringworm.
What is the ringworm on the skin?
The appearance of the skin of the affected area may appear scaly and dry and is usually itchy.The characteristic of the ringworm or of the skin patches in tinea corporis includes the following: The ringworm is somewhat oval in shape or resembling a ring. The borders or edges of the ring are irregular which may have a wavy pattern similar to ...
How long does it take for tinea corporis to appear?
It is usually asymptomatic and often starts as a flat and scaly patch on the skin. It takes about 4 days to 10 days from exposure to the fungi before the patch begins to develop.
Why does tinea corporis gladiatorum occur?
Tinea corporis gladiatorum is a form of tinea corporis present in wrestlers. The incidence is due to a skin-to-skin contact and the ringworm often develops in ...
Why is it called Ringworm?
It was so called ringworm due to its appearance similar to ringworm and its borders of irregular pattern and scaly texture similar to a snake or worm .Tinea corporis is generally a mild and non-life threatening skin condition that is caused by an infection from a fungus.
How often should I apply antifungal cream for tinea corporis?
The anti-fungal cream is usually applied twice a day for a period of two weeks or depending on the agent being used for treatment.The usual anti-fungal treatment for tinea corporis includes the following: Oral antifungal medications are given when tinea corporis remains unresponsive to topical therapy.
Treatment
Medical uses
- Luliconazole (Luzu) is an imidazole topical cream approved by the FDA in November 2013 for treatment of interdigital tinea pedis, tinea cruris, and tinea corporis. Approval was based on the results of three positive studies that evaluated 679 patients with either tinea pedis, corporis, or cruris. [28, 29]
Research
- The safety and efficacy of luliconazole topical cream 1% for tinea corporis was evaluated in a randomized, double-blind, vehicle-controlled, multicenter clinical trial in 75 individuals aged 2-17 years with a clinical- and culture-confirmed diagnosis of tinea corporis. Patients were randomized to receive luliconazole or vehicle cream. About 1-inch of topical cream was applied of the surrou…
Mechanism of action
- Allylamines (eg, naftifine, terbinafine) and the related benzylamine butenafine inhibit squalene epoxidase, which converts squalene to ergosterol. Inhibition of this enzyme causes squalene, a substance toxic to fungal cells, to accumulate intracellularly and leads to rapid cell death. Allylamines bind effectively to the stratum corneum because of their lipophilic nature. They also …
Pharmacology
- The mechanism of action of oral micronized griseofulvin against dermatophytes is disruption of the microtubule mitotic spindle formation in metaphase, causing arrest of fungal cell mitosis. A dose of 10 mg/kg/d for 4 weeks is effective. In addition, griseofulvin induces the cytochrome P-450 enzyme system and can increase the metabolism of CYP-450dependent drugs. It is the syst…
Clinical significance
- Systemic azoles (eg, fluconazole, itraconazole, ketoconazole) function similar to the topical agents, causing cell membrane destruction. [7]
Side effects
- Oral ketoconazole at 3-4 mg/kg/d may be given. However, this agent carries an associated risk of hepatitis in less than 1 in 10,000 cases and is rarely used orally for dermatophyte infections.
Interactions
- Oral itraconazole in doses of 100 mg/d for 2 weeks shows high efficacy. With an increased dose of 200 mg/d, the treatment duration can be reduced to 1 week. However, the cytochrome P-450 activity of itraconazole allows for potential interactions with other commonly prescribed drugs. [31] When it is appropriate to prescribe the drug, there may be some advantage to giving itracon…