Antibiotics work by killing bacteria or keeping them from growing. Resistant bacteria keep growing, even when antibiotics are used. This problem is seen most often in hospitals and nursing homes. New antibiotics are created to work against some resistant bacteria.
Do antibiotics work against resistant bacteria?
Antibiotics do not work against bacteria that have become resistant. When antibiotics are not used correctly, they may not kill all of the bacteria. The bacteria that an antibiotic does not kill can grow stronger.
What are antibiotic-resistant germs?
Some of those germs are resistant to antibiotics. Antibiotics kill germs that cause infections. But antibiotic-resistant germs find ways to survive. Antibiotics also kill good bacteria that protect the body from infection. Antibiotic-resistant germs can multiply. Some resistant germs can also give their resistance directly to other germs.
How can I help prevent the spread of antibiotic-resistant bacteria?
How can I help prevent the spread of antibiotic-resistant bacteria? 1 Understand that antibiotics cannot cure many common illnesses. 2 Always take antibiotics exactly as ordered by your healthcare provider. 3 Never save antibiotics or take leftover antibiotics that were given to you for another illness. 4 Wash your hands often with soap...
What happens if antibiotics are not used correctly?
When antibiotics are not used correctly, they may not kill all of the bacteria. The bacteria that an antibiotic does not kill can grow stronger. The antibiotic may not be able to kill the new germs. Germs can become resistant when the wrong type, wrong dose, or wrong treatment length of antibiotic is used.

How do you treat an infection that is resistant to antibiotics?
Antibiotic-resistant infections are treated with other types of antibiotics. Your NYU Langone doctor prescribes these medications based on the type of infection you have—and the types of medications to which the organism responds. Antibiotics may be taken by mouth or given through a vein with intravenous (IV) infusion.
What happens if an infection doesn't go away with antibiotics?
Someone with an infection that is resistant to a certain medicine can pass that resistant infection to another person. In this way, a hard-to-treat illness can be spread from person to person. In some cases, the antibiotic-resistant illness can lead to serious disability or even death.
What happens if your resistant to antibiotics?
Antibiotic resistance has spread around the world, and it's making some diseases, such as meningitis or pneumonia, more difficult to treat. You might need stronger, more expensive drugs. Or you might need to take them longer. You also might not get well as quickly, or you could develop other health issues.
Can resistant antibiotics work?
Antibiotic resistance happens when the germs no longer respond to the antibiotics designed to kill them. That means the germs are not killed and continue to grow. It does not mean our body is resistant to antibiotics.
What causes antibiotic resistance?
The main cause of antibiotic resistance is antibiotic use. When we use antibiotics, some bacteria die but resistant bacteria can survive and even multiply. The overuse of antibiotics makes resistant bacteria more common. The more we use antibiotics, the more chances bacteria have to become resistant to them.
Can you take a second course of antibiotics?
Accidentally taking an extra dose Accidentally taking 1 extra dose of your antibiotic is unlikely to cause you any serious harm. But it will increase your chances of getting side effects, such as pain in your stomach, diarrhoea, and feeling or being sick.
What do you mean by antibiotic resistance?
Antibiotic resistance occurs when bacteria develop the ability to survive exposure to antibiotics that were designed to kill them or stop their growth. Antibiotic resistant bacteria are free to grow, multiply and cause infection within the host even when exposed to antibiotics.
What is meant when a bacterium is said to become resistant to an antibiotic?
What is meant when a bacterium is said to become "resistant" to an antibiotic? The antibiotic kills or inhibits the bacterium. The antibiotic is metabolized by the bacterium, providing more energy for growth of the cell. The bacterium is neither killed nor inhibited by the antibiotic.
What is antibiotic resistance?
Antibiotic resistance happens when the germs no longer respond to the antibiotics designed to kill them. That means the germs are not killed and continue to grow. It does not mean our body is resistant to antibiotics.
How can antibiotics contribute to antibiotic resistance?
This is because increases in antibiotic resistance are driven by a combination of germs exposed to antibiotics, and the spread of those germs and their mechanisms of resistance.
What is an antibiotic?
Antibiotics are critical tools for preventing and treating infections caused by specific bacteria in people, animals, and crops. In health care, antibiotics are one of our most powerful drugs for fighting life-threatening bacterial infections.
How can I protect myself and my family from antibiotic resistance?
No one can completely avoid getting an infection, but there are additional steps you can take to protect yourself and your family.
What is the impact of antibiotic resistance on health?
Antibiotic resistance jeopardizes advancements in modern health care that we have come to rely on, such as joint replacements, organ transplants, and cancer therapy. These procedures have a significant risk of infection, and patients won’t be able to receive them if effective antibiotics are not available.
How to feel better when you don't need an antibiotic?
If your doctor decides an antibiotic is the best treatment when you are sick: Take the antibiotic exactly as your doctor tells you. Do not share your antibiotic with others. Do not save them for later.
What to do if you are sick and you are not getting an antibiotic?
Talk to your doctor about the best treatment if you are sick. Never pressure your doctor to prescribe an antibiotic. When antibiotics aren’t needed, they won’t help you, and their side effects could still cause harm. Ask your doctor or pharmacist about steps you can take to feel better when an antibiotic isn’t needed.
How are antibiotic-resistant infections treated?
But it might have certain drawbacks. It may have more side effects or a risk of promoting more resistance. In a few cases, your provider might not have another option. In this case, you will get supportive care.
What are the symptoms of an antibiotic-resistant infection?
They can cause many symptoms. But symptoms alone can’t tell you if an infection is from germs that are resistant to antibiotics.
What causes antibiotic resistance?
Antibiotic resistance can happen when bacteria are treated with an antibiotic. The medicine kills most of these germs. But a small group may survive. This might happen in a number of ways. The germs may:
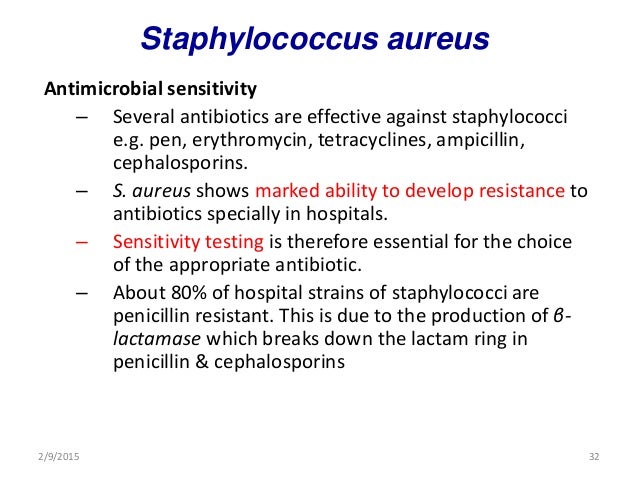
What is the difference between MRSA and Staphylococcus aureus?
Antibiotic resistance is often linked to a specific germ and antibiotic. For example, Staphylococcus aureus (or “staph”) is a type of bacteria that can cause illness. Methicillin-resistant S. aureus (MRSA) is a specific strain of staph bacteria. MRSA no longer responds to the antibiotic methicillin (and closely related medicines).
How do resistant bacteria spread?
When you touch the same object, the germs can enter your body. Often this is through a cut on your skin. Some infections can spread in the air when a person sneezes or coughs. Others can spread through sharing food with an infected person. Sexual contact is one more way these infections spread.
Why should you use antibiotics only when needed?
So you should use these medicines only when needed. Antibiotic resistance is often linked to a specific germ and antibiotic.
Why is it important to practice good hygiene?
Practice good hygiene. It helps prevent the spread of infections that are resistant to antibiotics.
What happens when you are infected with antibiotic resistance?
When antibiotics don't work, the result can be. longer illnesses.
What are some examples of bacteria resistant to antibiotics?
Examples of the types of bacteria that have become resistant to antibiotics include those that cause skin infections, urinary tract infections, meningitis, sexually transmitted diseases and respiratory tract infections such as pneumonia. In cooperation with other government agencies, the Food and Drug Administration ...
Why do we need antibiotic labeling?
Antibiotic labeling contains required statements in several places advising health care professionals that these drugs should be used only to treat infections that are believed to be caused by bacteria. Labeling also encourages health care professionals to counsel patients about proper use.
What is the term for the disease that occurs when bacteria change in a way that reduces or eliminates the effectiveness?
Misuse and overuse of these drugs, however, have contributed to a phenomenon known as antibiotic resistance. This resistance develops when potentially harmful bacteria change in a way that reduces or eliminates the effectiveness of antibiotics.
What is the FDA's role in labeling antibiotics?
FDA has also encouraged the development of new drugs, vaccines, and improved diagnostic tests for infectious diseases.
Why should patients not demand antibiotics?
Patients should not demand antibiotics when a health care professional says the drugs are not needed. Health care professionals should prescribe antibiotics only for infections they believe to be caused by bacteria.
When is it important to take antibiotics?
When you are prescribed an antibiotic to treat a bacterial infection, it's important to take the medication exactly as directed. Here are more tips to promote proper use of antibiotics. Take the antibiotics as prescribed. It's important to take the medication as prescribed by your doctor, even if you are feeling better.
Why are germs resistant to antibiotics?
Germs can become resistant when the wrong type, wrong dose, or wrong treatment length of antibiotic is used. Germs can also become resistant to more than one type of antibiotic. This has made it harder to cure infections that were once easily treated.
What are the risks of antibiotic resistant bacteria?
What are the risks of antibiotic-resistant bacteria? People with infections caused by antibiotic-resistant bacteria stay sick longer. Treatment requires more healthcare provider visits or longer hospital stays. Stronger antibiotic medicine may need to be given and this can cause worse side effects.
How do bacteria become resistant?
The bacteria that an antibiotic does not kill can grow stronger. The antibiotic may not be able to kill the new bacteria. Bacteria can become resistant when the wrong type, wrong dose, or wrong treatment length of antibiotic is used. They can also become resistant to more than one type of antibiotic. This has made it harder to cure infections that used to be easily treated.
How to get rid of a bacterial infection?
Never save antibiotics or take leftover antibiotics that were given to you for another illness. Wash your hands often with soap and hot water. Carry germ-killing gel with you. You can use the gel to clean your hands when you have no soap and water. Clean surfaces well.
Can antibiotics make a virus worse?
Stronger antibiotic medicine may need to be given and this can cause worse side effects. Any delay in treatment can cause the infection to become worse. Even if the stronger antibiotics kill the bacteria, the infection can become life-threatening.
Can you refuse treatment?
You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Can you take antibiotics for ear infections?
Your healthcare provider may not order antibiotics to treat you or your child. Antibiotics are not usually needed to treat many colds and ear infections. Always take antibiotics exactly as ordered by your healthcare provider. Ask when you should start to feel better.
How does antibiotic resistance happen?
How Antibiotic Resistance Happens. Antibiotics save lives but any time antibiotics are used, they can cause side effects and lead to antibiotic resistance. Since the 1940s, antibiotics have greatly reduced illness and death from infectious diseases. However, as we use the drugs, germs develop defense strategies against them.
How do antibiotics fight germs?
Antibiotics fight germs (bacteria and fungi). But germs fight back and find new ways to survive. Their defense strategies are called resistance mechanisms . Bacteria develop resistance mechanisms by using instructions provided by their DNA. Often, resistance genes are found within plasmids, small pieces of DNA that carry genetic instructions from one germ to another. This means that some bacteria can share their DNA and make other germs become resistant.
What bacteria break down antibiotics?
Germs change or destroy the antibiotics with enzymes, proteins that break down the drug. Example: Klebsiella pneumoniae bacteria produce enzymes called carbapenemases, which break down carbapenem drugs and most other beta-lactam drugs. Bypass the effects of the antibiotic.
How did antibiotics help the world?
However, as we use the drugs, germs develop defense strategies against them. This makes the drugs less effective.
What is the name of the drug that treats infections?
Antimicrobials Treat Infections Caused by Microbes. Microbes are very small living organisms, like bacteria. Most microbes are harmless and even helpful to humans, but some can cause infections and disease. Drugs used to treat these infections are called antimicrobials .
What is Gram negative bacteria?
Example: Gram-negative bacteria have an outer layer (membrane) that protects them from their environment. These bacteria can use this membrane to selectively keep antibiotic drugs from entering. Get rid of the antibiotic.
Can Staphylococcus aureus be bypassed?
Example: Some Staphylococcus aureus bacteria can bypass the drug effects of trimethoprim . Change the targets for the antibiotic. Many antibiotic drugs are designed to single out and destroy specific parts (or targets) of a bacterium. Germs change the antibiotic’s target so the drug can no longer fit and do its job.
Why do we use antibiotics?
We use a lot of antibiotics in humans — too much, and not always for the right reasons. When we prescribe antibiotics for viral illnesses like a cold, the flu, or common sinusitis, we create a massive shift in the body’s bacteria for no good reason (antibiotics are useless against viral infections).
What is the purpose of antibiotic testing?
Antibiotic testing involves growing a sample of urine in a petri dish, finding the bacteria causing infection, and testing them against a range of antibiotics to see which ones kill the bacteria best. This process takes time and money, but it’s important to get the right treatment for your infection.
What can I take for UTI pain?
While you wait for the results, taking over-the-counter analgesics like acetaminophen or ibuprofen and drinking more water can help to relieve UTI pain and discomfort. If antibiotic resistance continues to grow, more people will need intravenous treatment for UTIs we used to cure with simple oral antibiotic courses.
How do bacteria survive under pressure?
Under pressure, bacteria exchange genetic material and evolve, gaining survival traits like the ability to pump out, break down, or avoid antibiotics we want to use against them. Without antibiotic tools to kill them, these bacteria can attack us freely, and sometimes win.
What to do if you have a UTI?
If you’re having UTI symptoms like burning with urination, more frequent urination, bloody or cloudy urine, low abdominal pain, or fever, you should see a medical provider to get tested. You’ll have to urinate into a container and the medical office will test for products of bacterial metabolism.
Can UTIs be prevented?
Unfortunately, most UTIs are not completely preventable, and are caused by differences in the structure or function of the urinary tract and immune system. But there are things you can do to keep healthy. For example, stay hydrated to increase urine production and flush out unwanted bacterial intruders.
Is antibiotic resistance on the rise?
Antibiotic-resistant urinary tract infections are on the rise. October 14, 2019. By: Lisa Bebell, MD , Contributor. There is a global crisis of antibiotic resistance, and urinary tract infections (UTIs) may be the canary in the coal mine. UTIs are one of the most common types of infections; at least one in two women and one in 10 men will ...
What is the cause of antibiotic resistance?
Antibiotic resistance occurs when the bacteria that is causing the infection is no longer affected by a particular antibiotic and is able to continue to grow and multiply. Inappropriate and unnecessary antibiotic use contributes to the increasing problem of antibiotic resistance.
Why do antibiotics sometimes not work for a urinary tract infection?
If an antibiotic doesn’t work it is likely that the bacteria causing the UTI is not susceptible or is resistant to the antibiotic you are taking .
What are the signs that an antibiotic is not working for a urinary tract infection?
Usually people start to feel better within 1-2 days of starting an antibiotic to treat a bladder infection. If your symptoms don’t improve or you start to feel worse then your antibiotic may not be working.
What is the best treatment for UTI?
Facebook. Twitter. Email. Print. Antibiotics are the mainstay of treatment for urinary tract infections (UTIs), most of which are caused by a bacteria called Escherichia Coli (E. Coli). Infections of the lower urinary tract, which includes bladder infections (cystitis), are the most common type of UTI and are usually treated with ...
What to do if antibiotic doesn't work?
What should I do if my antibiotic doesn’t work for my urinary tract infection? If your symptoms don’t improve within a couple of days or get worse after starting an antibiotic you should contact your healthcare provider. A different antibiotic, a longer course of antibiotics or another treatment may be required.
What to do if you have a UTI?
A physical exam or urine sample may be required. When you have a UTI it’s important to: Only take an antibiotic that has been prescribed for you. Take the antibiotic exactly as instructed by your healthcare provider and finish the full course of treatment even if you feel better. Drink plenty of water and other fluids.
What happens if your antibiotics aren't working?
Feeling pressure or cramping in your lower abdomen. If your antibiotic is not working then these symptoms will likely continue and you may even develop symptoms of a more serious kidney infection (pyelonephritis) including: Fever. Chills.
Why do we use intravenous antibiotics?
Answer: We use intravenous antibiotics for very severe infections, such as sepsis because intravenous antibiotics reach tissues faster and at higher concentrations than oral antibiotics. We may also use intravenous antibiotics for infections in parts of the body where penetration of oral antibiotics is less effective, ...
Why do we need to take antibiotics when we feel sick?
It is essential to use antibiotics smartly, as the rate of emergence of multi-drug resistant bacteria continues to increase.
What does it mean to be antimicrobial steward?
Can you explain what this means? A: Antimicrobial stewardship means using antibiotics in a judicious way in order to avoid the emergence of resistant bacteria.
Why are hospitals a source of MRSA?
Why? A: In general, health care facilities (including hospitals and nursing facilities) have a much higher rate of resistant bacteria, simply because they care for people with the most severe infections who have received antibiotics frequently.
Do antibiotics kill viruses?
Probably the most frequent case is with viral illnesses, such as colds. Antibiotics kill bacteria only and don’t have any effect against viruses.
Can you get an infection from IV antibiotics?
A: Most patients who require IV antibiotics have had some previous medical problem or hospitalization that has made them more prone to infection. Sometimes, though, people get a deep or serious infection from bacteria living on their own skin.
Is IV antibiotics related to antibiotic resistance?
Q: Is the use of IV antibiotics related to a rise in antibiotic-resistant infections? A: Absolutely. As antibiotic resistance has increased, our ability to use oral antibiotics to treat infections has declined. Infections that generally would not require intravenous antibiotics now often do.

A Public Health Issue
- Antibiotic resistance is a growing public health concern worldwide. When a person is infected with an antibiotic-resistant bacterium, not only is treatment of that patient more difficult, but the antibiotic-resistant bacterium may spread to other people. When antibiotics don't work, the result can be 1. longer illnesses 2. more complicated illnesse...
Antibiotics Fight Bacteria, Not Viruses
- Antibiotics are meant to be used against bacterial infections. For example, they are used to treat strep throat, which is caused by streptococcal bacteria, and skin infections caused by staphylococcal bacteria. Although antibiotics kill bacteria, they are not effective against viruses. Therefore, they will not be effective against viral infections such as colds, most coughs, many ty…
Follow Directions For Proper Use
- When you are prescribed an antibiotic to treat a bacterial infection, it's important to take the medication exactly as directed. Here are more tips to promote proper use of antibiotics. 1. Take the antibiotics as prescribed.It's important to take the medication as prescribed by your doctor, even if you are feeling better. If treatment stops too soon, and you become sick again, the remai…
What FDA Is Doing
- FDA combating antibiotic resistance through activities that include 1. Approval of certain new antibiotics. Since 2015, FDA approved new antibiotics that can treat certain resistant bacteria. Health care professional are encouraged to use the new antibiotics appropriately and for some antibiotics, use only in patients who have limited or no other treatment options. 2. Labeling regul…