Healthline.com
Aug 13, 2021 · “It’s also probably better for your cardiovascular system, as there is early atherosclerosis and cardiovascular morbidity in RA. Most of the studies are supporting the idea that early intervention...
Top10homeremedies.com
Gold is effective in the treatment of rheumatoid arthritis when it is given intramuscularly. Intramuscular gold salts were, until the 1990’s, the most often used DMARD agents but have been replaced by Methotrexate and other DMARDS as the preferred agents to treat RA. Two injectable compounds are available, (Myochrysine® and Solganal®). Gold compounds are rarely used …
Webmd.com
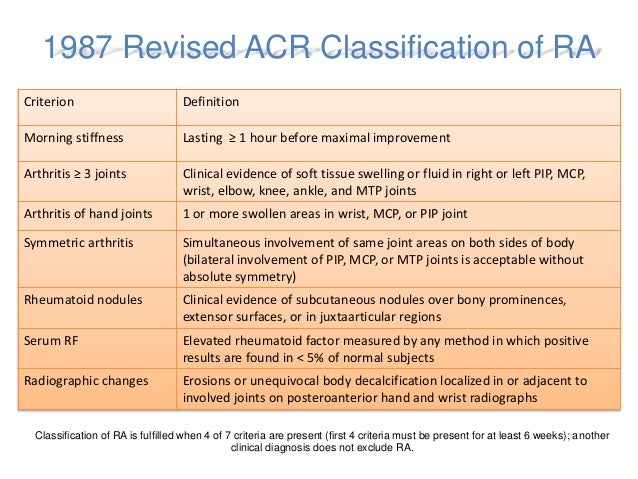
RA is diagnosed by reviewing symptoms, conducting a physical examination, and doing X-rays and lab tests. It’s best to diagnose RA early—within 6 months of the onset of symptoms—so that people with the disease can begin treatment to slow or stop disease progression (for example, damage to joints).
How can I Manage my Ra on a daily basis?
The American College of Rheumatology (ACR) have published its new 2020 guideline for rheumatoid arthritis treatments. The ACR updates its guideline for the treatment of rheumatoid arthritis (RA) every few years. The last changes appeared in 2015. Since then, new drugs have hit the market, older drugs have been reassessed, and there’s more ...
Why is early rheumatoid arthritis treatment so important?
The goals of rheumatoid arthritis treatment are to ease pain, control inflammation and prevent long-term damage. Learn about which medicines your doctor may use first. Read More
What are the goals of treatment for rheumatoid arthritis (RA)?
Abatacept ( Orencia ). It attaches to and blocks the action of cells that promote inflammation. You'll get an infusion once every 2 weeks to start. Then you'll get the drug once a month. Each ...
What is the first-line drug treatment for rheumatoid arthritis (RA)?
Slowing down the progression of bone damage. Reducing fatigue. Undergoing infusion therapy for rheumatoid arthritis can provide relief from symptoms anywhere between six months to a year. The length of each infusion session depends on the severity of the illness, as well as the type of medication being administered.
When should you start treatment for rheumatoid arthritis?
The recommendations also suggest patients at risk for chronic arthritis should begin a course of disease-modifying anti-rheumatic drugs (DMARDs) within three months of symptoms appearing.Aug 13, 2021
When should you start biologics for rheumatoid arthritis?
Why is early treatment of rheumatoid arthritis important?
Identification of RA at initial presentation and treatment at earlier stage can affect disease course, prevent the development of joint erosions or retard progression of erosive disease (5, 9).
When should you start RA DMARD?
Is methotrexate safer than biologics?
How long can you stay on biologics?
Should arthritis be treated early?
Can RA stay mild?
What is the initial management of rheumatoid arthritis?
What is the first-line treatment for arthritis?
What is the difference between sulfasalazine and methotrexate?
What Is Rheumatoid Arthritis (RA)?
Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by m...
What Are The Signs and Symptoms of RA?
With RA, there are times when symptoms get worse, known as flares, and times when symptoms get better, known as remission.Signs and symptoms of RA...
What Are The Risk Factors For RA?
Researchers have studied a number of genetic and environmental factors to determine if they change person’s risk of developing RA.Characteristics t...
Who Should Diagnose and Treat RA?
A doctor or a team of doctors who specialize in care of RA patients should diagnose and treat RA. This is especially important because the signs an...
What Are The Complications of RA?
Rheumatoid arthritis (RA) has many physical and social consequences and can lower quality of life. It can cause pain, disability, and premature dea...
How Can I Manage Ra and Improve My Quality of Life?
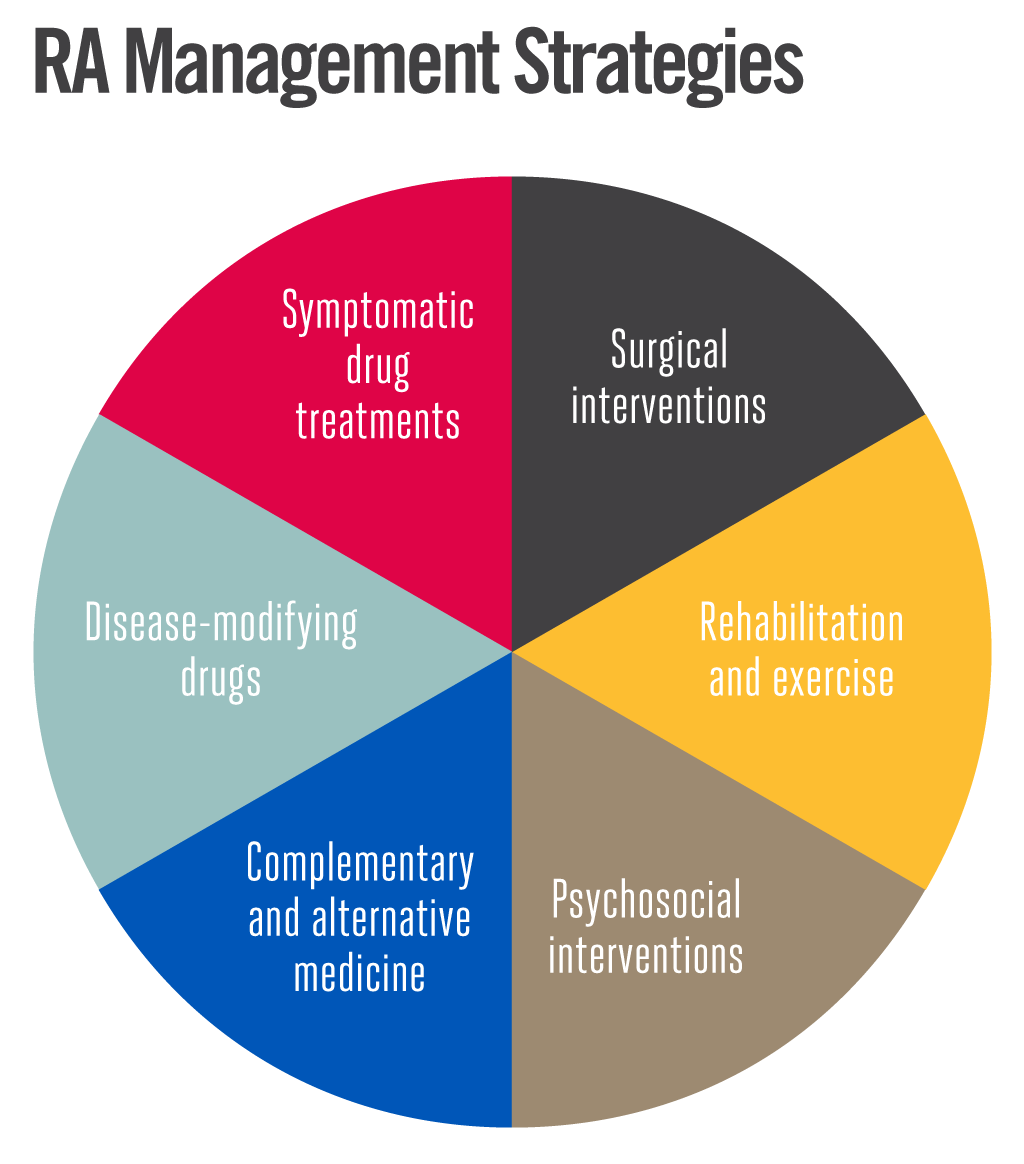
RA affects many aspects of daily living including work, leisure and social activities. Fortunately, there are multiple low-cost strategies in the c...
Learn More About Arthritis
1. Arthritis Types 2. Physical Activity for Arthritis 3. Frequently Asked Questions (FAQs) 4. Arthritis-Related Statistics
How to fix rheumatoid arthritis?
Surgery may help restore your ability to use your joint. It can also reduce pain and improve function. Rheumatoid arthritis surgery may involve one or more of the following procedures: Synovectomy. Surgery to remove the inflamed lining of the joint (synovium) can help reduce pain and improve the joint's flexibility. Tendon repair.
What are the drugs that slow the progression of rheumatoid arthritis?
Conventional DMARDs. These drugs can slow the progression of rheumatoid arthritis and save the joints and other tissues from permanent damage. Common DMARDs include methotrexate (Trexall, Otrexup, others), leflunomide (Arava), hydroxychloroquine (Plaquenil) and sulfasalazine (Azulfidine). Side effects vary but may include liver damage ...
Why is rheumatoid arthritis so difficult to diagnose?
Rheumatoid arthritis can be difficult to diagnose in its early stages because the early signs and symptoms mimic those of many other diseases. There is no one blood test or physical finding to confirm the diagnosis. During the physical exam, your doctor will check your joints for swelling, redness and warmth.
What does CRP mean in rheumatoid arthritis?
People with rheumatoid arthritis often have an elevated erythrocyte sedimentation rate (ESR, also known as sed rate) or C-reactive protein (CRP) level, which may indicate the presence of an inflammatory process in the body.
What tests can be done to diagnose rheumatoid arthritis?
Imaging tests. Your doctor may recommend X-rays to help track the progression of rheumatoid arthritis in your joints over time. MRI and ultrasound tests can help your doctor judge the severity of the disease in your body.
Does fish oil help with arthritis?
Fish oil. Some preliminary studies have found that fish oil supplements may reduce rheumatoid arthritis pain and stiffness. Side effects can include nausea, belching and a fishy taste in the mouth. Fish oil can interfere with medications, so check with your doctor first.
Does fish oil affect rheumatoid arthritis?
Plant oils. The seeds of evening primrose, borage and black currant contain a type of fatty acid that may help with rheumatoid arthritis pain and morning stiffness.
What is the goal of RA?
These goals primarily focus on: Reducing inflammation. Preventing further or permanent damage. Improving the quality of life. Reducing daily and long-term side effects. Following a strict treatment regimen could bring RA into remission. Remission means that the level of disease activity has decreased in the body.
Is there a cure for rheumatoid arthritis?
Rheumatoid arthritis (RA) has no cure, but doctors recommend that patients adhere to suggested treatments early in diagnosis to decrease the severity of symptoms. There are a variety of treatment methods used to control symptoms and stop joint damage, including medications, surgery, and daily routine and lifestyle changes.
What is DMARDs for arthritis?
DMARDs, or disease-modifying antirheumatic drugs, are long-term medications meant to slow or alter the progression of rheumatoid arthritis by stopping the immune system from attacking healthy tissue. These drugs protect joints and tissues from permanent damage and gradually reduce daily pain.
What is tight control for RA?
Depending on the severity of your symptoms, the goals of treatment will be to gain “tight control” of RA, meaning the disease’s activity is kept steadily at a low level. Keeping RA in “tight control” can prevent long-term joint damage. These goals primarily focus on:
Can RA go into remission?
Following a strict treatment regimen could bring RA into remission. Remission means that the level of disease activity has decreased in the body. It is never an indication that symptoms will not return, but following remission, many patients can go for long periods of time without experiencing symptoms. There are many ways to treat rheumatoid ...
What does it mean to be in remission?
Remission means that the level of disease activity has decreased in the body. It is never an indication that symptoms will not return, but following remission, many patients can go for long periods of time without experiencing symptoms.
Can NSAIDs be used for kidney damage?
There are prescription NSAIDs that are safer or gastrointestinal friendly for people prone to stomach problems. NSAIDs can be taken orally or applied directly to the joint as a patch or cream. Corticosteroid medications or another form of drug used in the treatment of RA .
What is the goal of rheumatoid arthritis treatment?
The goal of rheumatoid arthritis treatment now aims toward achieving the lowest possible level of arthritis disease activity and remission if possible, minimizing joint damage, and enhancing physical function and quality of life.
Is there a cure for rheumatoid arthritis?
Rheumatoid arthritis is a chronic disorder for which there is no known cure . Fortunately in the last few years, a shift in strategy toward the earlier institution of disease modifying drugs and the availability of new classes of medications have greatly improved the outcomes that can be expected by most patients.
What are the different types of rheumatoid arthritis drugs?
There are three general classes of drugs commonly used in the treatment of rheumatoid arthritis: non-steroidal anti-inflammatory agents (NSAIDs), corticosteroids, and disease modifying anti-rheumatic drugs (DMARDs). NSAIDs and corticosteroids have a short onset of action while DMARDs can take several weeks or months to demonstrate a clinical effect. DMARDs include methotrexate, sulfasalazine, leflunomide (Arava®), etanercept (Enbrel®), infliximab (Remicade®), adalimumab (Humira®), certolizumab pegol (Cimzia®), golimumab (Simponi®), abatacept (Orencia®), rituximab (Rituxan®), tocilizumab (Actemra®), anakinra (Kineret®), antimalarials (e.g. Plaquenil®). Other immunomodulators are occasionally used including azathioprine (Imuran) and cyclosporine. Because cartilage damage and bony erosions frequently occur within the first two years of disease, rheumatologists now move aggressively to a DMARD agent early in the course of disease, usually as soon as a diagnosis is confirmed. Analgesic drugs are also sometimes helpful in decreasing pain until DMARDs take effect. A summary table of how to monitor drug treatment in rheumatoid arthritis is included.
Can corticosteroids be used as adjunctive therapy?
Corticosteroids are useful in early disease as temporary adjunctive therapy while waiting for DMARDs to exert their antiinflammatory effects. Corticosteroids are also useful as chronic adjunctive therapy in patients with severe disease that is not well controlled on NSAIDs and DMARDs.
Can DMARD be used for rheumatoid arthritis?
Although both NSAIDs and DMARD agents improve symptoms of active rheumatoid arthritis, only DMARD agents have been shown to alter the disease course and improve radiographic outcomes. DMARDs have an effect upon rheumatoid arthritis that is different and may be slower. In most cases, when the diagnosis of rheumatoid arthritis is confirmed, DMARD agents should be started. The presence of erosions or joint space narrowing on x-rays of the involved joints is a clear indication for DMARD therapy, however one should not wait for x-ray changes to occur. The currently available drugs include:
Is methotrexate good for RA?
Methotre xate is now considered the first -line DMARD agent for most patients with RA. It has a relatively rapid onset of action at therapeutic doses (6-8 weeks), good efficacy, favorable toxicity profile, ease of administration, and relatively low cost. When looking at groups of patients on different DMARDS, the majority of patients continue to take Methotrexate after 5 years, far more than other therapies reflecting both its efficacy and tolerability. Methotrexate is effective in reducing the signs and symptoms of RA, as well as slowing or halting radiographic damage. It was as effective as leflunomide and sulfasalazine in one study, and its effectiveness given early and in higher doses approached the efficacy of etanercept and adalimumab as single therapies in terms of signs and symptom improvement. Methotrexate is also effective in many other forms of inflammatory arthritis including psoriatic arthritis and other spondyloarthopathies, and is used in many other autoimmune diseases.
Is hydrochloroquine safe for arthritis?
Hydroxychloroquine is an antimalarial drug which is relatively safe and well-tolerated agent for the treatment of rheumatoid arthritis. Chloroquine is another antimalarial agent that is also sometimes used. Because these drugs have limited ability to prevent joint damage on their own, their use should probably be limited to patients with very mild, seronegative, and nonerosive disease. Hydroxychloroquine is sometimes combined with methotrexate for additive benefits for signs and symptoms or as part of a regimen of “triple therapy” with methotrexate and sulfasalazine.
What is the treatment for RA?
Treatment for RA usually includes the use of medications that slow disease and prevent joint deformity, called disease-modifying antirheumatic drugs (DMARDs); biological response modifiers (biologicals) are medications that are an effective second-line treatment.
When does RA start?
RA can begin at any age, but the likelihood increases with age. The onset of RA is highest among adults in their sixties. Sex. New cases of RA are typically two-to-three times higher in women than men. Genetics/inherited traits. People born with specific genes are more likely to develop RA.
What are the consequences of rheumatoid arthritis?
It can cause pain, disability, and premature death. Premature heart disease. People with RA are also at a higher risk for developing other chronic diseases such as heart disease and diabetes.
How to help arthritis?
Learn more about physical activity for arthritis. Go to effective physical activity programs. If you are worried about making arthritis worse or unsure how to safely exercise, participation in physical activity programs can help reduce pain and disability related to RA and improve mood and the ability to move.
What is RA in medical terms?
What is rheumatoid arthritis (RA)? Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body. RA mainly attacks the joints, usually many joints at once.
What is RA in the body?
Rheumatoid arthritis, or RA, is an autoimmune and inflammatory disease, which means that your immune system attacks healthy cells in your body by mistake, causing inflammation (painful swelling) in the affected parts of the body. RA mainly attacks the joints, usually many joints at once. RA commonly affects joints in the hands, wrists, and knees.
What are the effects of RA on the body?
RA can also affect other tissues throughout the body and cause problems in organs such as the lungs, heart, and eyes. Top of Page.
How many recommendations are there for non-drug treatment for RA?
Since then, new drugs have hit the market, older drugs have been reassessed, and there’s more evidence for the role of nondrug treatments for RA. Of 44 recommendations, only seven were considered strong, meaning there’s clear evidence that the benefits of the treatment outweigh the risks and most patients endorse them.
What is the best treatment for rheumatoid arthritis?
Methotrexate. Methotrexate is a conventional disease-modifying anti-inflammatory drug (DMARD). It works to lower inflammation and slow an overactive immune system, which occurs in rheumatoid arthritis. The new guidelines strongly recommend methotrexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who ...
Why are the remaining recommendations called conditional?
The remaining recommendations are called conditional because they lack good evidence one way or the other. The new guidelines don’t address vaccinations — particularly relevant right now — or nondrug therapies like diet and exercise. Those are expected in a later update. Here are some of the main takeaways:
Does methotrexate help with arthritis?
It works to lower inflammation and slow an overactive immune system, which occurs in rheumatoid arthritis. The new guidelines strongly recommend methotrexate alone (monotherapy) as the first treatment for people with moderate to high disease activity who haven’t taken DMARDs before. Methotrexate monotherapy is strongly recommended ...
What is the treatment to target approach?
Although there’s not much evidence to support it, a treat-to-target approach is strongly recommended for patients who haven’t taken biologics or small molecule drugs. In treat-to-target, doctors and patients decide on a goal and adjust treatment until the goal is reached. Though everyone hopes for remission, many patients may not be able to achieve it. A more realistic aim is low disease activity, which keeps symptoms under control and helps maintain a good quality of life. Still, the guideline states the goal should be tailored to each patient and remission can be the target when possible.
What is the most important factor in all treatment considerations?
The most important factor in all treatment considerations is shared decision-making, where patients are informed of all their options, including nondrug ones, and have a full voice in their own care. “Patients were involved in every step of the process [of creating the update], and the recommendations truly reflect their perspectives,” Dr. Fraenkel says.
What is the goal of treat to target?
In treat-to-target, doctors and patients decide on a goal and adjust treatment until the goal is reached. Though everyone hopes for remission, many patients may not be able to achieve it. A more realistic aim is low disease activity, which keeps symptoms under control and helps maintain a good quality of life.
Can RA affect your joints?
Read about it and ask your doctor questions. You probably first went to the doctor because of joint pain and swelling. But RA can affect many parts of your body. Talk to your rheumatologist about the different ways RA attacks your joints and organs. Learn how to control the disease.
Is RA a complex disease?
RA is a complex disease. Read about it and ask your doctor questions. You probably first went to the doctor because of joint pain and swelling. But RA can affect many parts of your body. Talk to your rheumatologist about the different ways RA attacks your joints and organs. Learn how to control the disease.
Can you find a rheumatologist near you?
Many insurance companies have people who will help you coordinate your treatment. If you can’t find a rheumatologist near you, video office visits may be an option.
What is the role of a PCP and a rheumatologist?
Be sure your primary care physician (PCP) and your rheumatologist share information. Rheumatologists focus on RA and your PCP handles other health problems, like diabetes, high blood pressure and osteoporosis. But each needs to know what the other is doing. Your job is to choose your doctors and ensure they talk to each other.
What is the best treatment for rheumatoid arthritis?
If you have rheumatoid arthritis (RA), your doctor may suggest you get an infusion treatment -- medicine that goes into your body through a needle they place in a vein.
How long does it take to get an infusion for RA?
And it takes between 30 minutes and 4 hours to get each infusion. Infusion Treatments for RA. Four biologic drugs for RA come as infusions: Abatacept ( Orencia ). It attaches to and blocks the action of cells that promote inflammation. You'll get an infusion once every 2 weeks to start.
How long does it take for Rituximab to work?
They block a substance called tumor necrosis factor (TNF) in your blood that promotes inflammation. Each infusion can take up to 4 hours. You'll get three infusions in the first 6 weeks of treatment, and then once every 8 weeks. Your symptoms may start to improve after two to three doses. Rituximab ( Rituxan ).
Can you take medicine before an infusion?
You may get medicine before your treatment to relax you if you're nervous. While the medicine goes in, you can read a book or watch a movie. Side Effects of Infusion Treatments. Infusions can cause mild reactions like: Pain, redness, or swelling of your skin where the needle goes in. Headache.
Can you read while taking biologics?
While the medicine goes in, you can read a book or watch a movie. Rarely, the reaction can be severe. If you have these symptoms, your doctor will stop the infusion and treat your symptoms. Because biologic drugs weaken your immune system, they can increase your risk for infections like colds, the flu, or pneumonia.
Can you give yourself shots with an infusion?
There are pros and cons to both methods. An infusion may be a better option if you don't like to give yourself shots and you don't want to take your medicine as often.
Can rheumatoid arthritis be treated with infusions?
Infusion Therapy for Rheumatoid Arthritis (RA) Having rheumatoid arthritis (RA) can turn even the most mundane tasks — such as personal hygiene, eating, and driving — into monumental tasks. So when you start experiencing symptoms, you hope your doctor is able to prescribe effective medications to help you resume your life with a sense of normalcy.
What are the benefits of infusion therapy for rheumatoid arthritis?
Their benefits include: Providing relief from swelling, pain, and stiffness. Allowing you to conduct your activities of daily living without difficulty. Preventing additional joint damage. Slowing down the progression of bone damage. Reducing fatigue. Undergoing infusion therapy for rheumatoid arthritis can provide relief from symptoms anywhere ...
What are the symptoms of arthritis?
In addition to painful, swollen joints, other symptoms may include fatigue, stiffness, and loss of appetite.
Does RA medication affect the immune system?
While doctors are not clear why this medication is effective for autoimmune conditions, the theory is that it interferes with the metabolic communication between the bodies immune system cells. If the cells can’t effectively communicate with each other, then the excessive immune response of RA is reduced.
Can arthritis be cured?
Joint damage worries and aching hands are no fun, and if you’re experiencing those kinds of problems because of rheumatoid arthritis you may have options that can help you feel better. There’s no cure for arthritis, which is unfortunate, but feeling better is definitely possible.
Is there a cure for arthritis?
There’s no cure for arthritis, which is unfortunate, but feeling better is definitely possible. The progression of RA may be diminished in severity and duration by the combination of medicines and therapy that work best as determined by you and your physician.
Is hydroxychloroquine good for arthritis?
Now it is generally used for rheumatoid arthritis, but it has also been shown to work well for juvenile arthritis, some lupus symptoms, and other types of autoimmune conditions.
Is hydroxychloroquine safe for RA?
If you have rheumatoid arthritis, talking to your doctor about hydroxychloroquine may be the right choice for your needs. The medication is generally well-tolerated, and has even been found safe overall ...
Can hydrochloroquine help with joint pain?
You can also put off joint damage, and in some cases, you can do more than just slow it down. Being able to stop joint damage can lessen pain and mean a better quality of life. Hydroxychloroquine is one of the medications that can be a valuable part of your treatment plan.

Diagnosis
Treatment
- There is no cure for rheumatoid arthritis. But clinical studies indicate that remission of symptoms is more likely when treatment begins early with medications known as disease-modifying antirheumatic drugs (DMARDs).
Clinical Trials
- Explore Mayo Clinic studiestesting new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and Home Remedies
- You can take steps to care for your body if you have rheumatoid arthritis. These self-care measures, when used along with your rheumatoid arthritis medications, can help you manage your signs and symptoms: 1. Exercise regularly.Gentle exercise can help strengthen the muscles around your joints, and it can help reduce fatigue you might feel. Check w...
Alternative Medicine
- Some common complementary and alternative treatments that have shown promise for rheumatoid arthritis include: 1. Fish oil.Some preliminary studies have found that fish oil supplements may reduce rheumatoid arthritis pain and stiffness. Side effects can include nausea, belching and a fishy taste in the mouth. Fish oil can interfere with medications, so check with yo…
Coping and Support
- The pain and disability associated with rheumatoid arthritis can affect a person's work and family life. Depression and anxiety are common, as are feelings of helplessness and low self-esteem. The degree to which rheumatoid arthritis affects your daily activities depends in part on how well you cope with the disease. Talk to your doctor or nurse about strategies for coping. With time yo…
Preparing For Your Appointment
- While you might first discuss your symptoms with your family doctor, he or she may refer you to a doctor who specializes in the treatment of arthritis and other inflammatory conditions (rheumatologist) for further evaluation.