What drugs are used to treat TB?
1. Garlic...
2. Bananas...
3. Drumstick...
4. Indian Gooseberry...
5. Oranges...
6. Custard Apple...
7. Black Pepper...
8. Walnuts...
Learn More...What are the side effects of TB medications?
These are the three treatment options:
- Isoniazid (INH): This is the most common therapy for latent TB. You typically take an isoniazid antibiotic pill daily for 9 months.
- Rifampin ( Rifadin, Rimactane): You take this antibiotic each day for 4 months. ...
- Isoniazid and rifapentine: You take both of these antibiotics once a week for 3 months under your doctor’s supervision.
Is MDR TB curable?
When taking these medications, call your doctor immediately if you have any of the following:
- Nausea or vomiting
- Loss of appetite
- A yellow color to your skin (jaundice)
- Dark urine
- Easy bruising or bleeding
- Blurred vision
What is the treatment for drug resistant TB?
Treatment of MDR-TB. It is curable but has long term hazards on the body. Yes, it is 100% curable. Multi-drug resistance tuberculosis is TB that does not respond to at least rifampicin and isoniazid, the two powerful anti-tb drugs.
Why is multidrug used to treat TB?
The bacteria that cause tuberculosis (TB) can develop resistance to the antimicrobial drugs used to cure the disease. Multidrug-resistant TB (MDR-TB) is TB that does not respond to at least isoniazid and rifampicin, the 2 most powerful anti-TB drugs.
What is treatment for MDR-TB?
Levofloxacin and moxifloxacin are the two most frequently recommended agents, and the WHO has recommended the use of these drugs for the treatment of MDR-TB. The optimal dose of levofloxacin is 750 mg once daily and that of moxifloxacin is 400 mg once daily.
Can MDR-TB be cured completely?
The Grim Facts of Today's TB Therapy The pandemic can't be overcome without improved cures. Only about half the people with MDR-TB around the world are successfully cured. TB treatment is lengthy and burdensome to patients and treatment providers alike.
How long is treatment for MDR-TB?
MDR- and XDR-TB need prolonged treatment duration, from 18 to 24 months after sputum culture conversion, as recommended by the World Health Organization (WHO) [2]. A prolonged duration of treatment may lead to poor adherence, higher cost and undue toxicity.
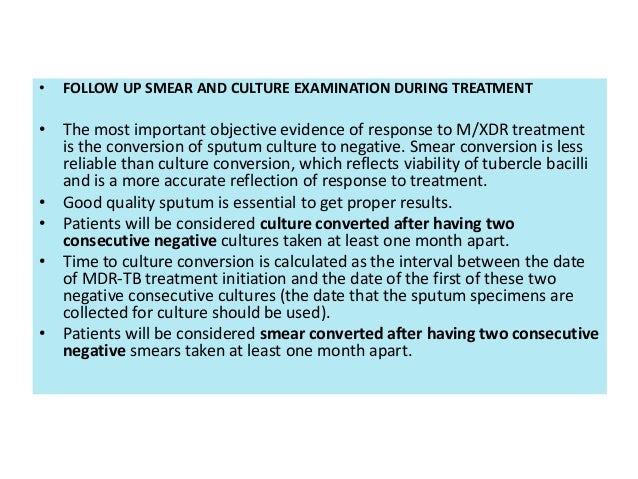
How do you know if MDR-TB treatment is working?
Physical Signs That TB Treatment Is WorkingA reduction in symptoms, such as less coughing.Overall improvement in the way one feels.Weight gain.Increased appetite.Improvement in strength and stamina.
Why is drug resistance a problem?
Antibiotic resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them. That means the germs are not killed and continue to grow. More than 2.8 million antibiotic-resistant infections occur in the U.S. each year.
How serious is MDR-TB?
MDR-TB, which is deemed a public health crisis by the World Health Organization (WHO), is caused by strains of TB bacteria that do not respond to standard antibiotics, which can lead to treatment failures or death.
Is MTB curable?
Although doctors tend to assure the patients that the disease is curable, current treatments do not prevent TB infection caused by Mycobacterium tuberculosis (Mtb) reinfection. In 2017, 10 million people fell ill with TB, and 1.6 million died from the disease (including 0.3 million among people with HIV).
Can drug-resistant cure?
In most cases, TB is treatable and curable; however, people with TB can die if they do not get proper treatment. Sometimes drug-resistant TB occurs when bacteria become resistant to the drugs used to treat TB. This means that the drug can no longer kill the TB bacteria.
WHO guidelines MDR-TB treatment?
Current policy recommendations on treatment and care for DR-TB. In patients with confirmed rifampicin-susceptible and isoniazid-resistant tuberculosis, treatment with rifampicin, ethambutol, pyrazinamide and levofloxacin is recommended for a duration of 6 months.
What Is Tuberculosis (TB)?
Tuberculosis (TB)(https://www.cdc.gov/tb/publications/factsheets/general/tb.htm) is a disease caused by bacteria that are spread from person to per...
What Is Multidrug-Resistant Tuberculosis (MDR TB)?
Multidrug-resistant TB (MDR TB) is caused by an organism that is resistant to at least isoniazid and rifampin, the two most potent TB drugs. These...
What Is Extensively Drug Resistant Tuberculosis (XDR TB)?
Extensively drug resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least...
How Does Drug Resistance Happen?
Resistance to anti-TB drugs can occur when these drugs are misused or mismanaged. Examples include when patients do not complete their full course...
Who Is at Risk For Getting MDR TB?
Drug resistance is more common in people who: 1. Do not take their TB medicine regularly 2. Do not take all of their TB medicine as told by their d...
How Can MDR TB Be Prevented?
The most important thing a person can do to prevent the spread of MDR TB is to take all of their medications exactly as prescribed by their health...
Is There A Vaccine to Prevent TB?
Yes, there is a vaccine for TB disease called Bacille Calmette-Guérin (BCG)(https://www.cdc.gov/tb/publications/factsheets/prevention/bcg.htm). It...
What Should I Do If I Think I Have been Exposed to Someone With TB Disease?
If you think you have been exposed to someone with TB disease, you should contact your doctor or local health department about getting a TB skin te...
What Are The Symptoms of TB Disease?
The general symptoms of TB disease include feelings of sickness or weakness, weight loss, fever, and night sweats. The symptoms of TB disease of th...
What is the most effective anti-TB drug?
Fluoroquinolones are often the most effective anti-TB drugs in an MDR-TB regimen. There are two important recommendations regarding fluoroquinolone use from the 2011 update of the Guidelines for the programmatic management of drug-resistant tuberculosis(1).
How early can you start anti-TB treatment?
Antiretroviral therapy (ART) is recommended for all patients with HIV and drug-resistant TB, irrespective of CD4 cell-count, as early as possible (within the first eight weeks) following initiation of the anti-TB treatment (strong recommendation) (1). The drug dosage is usually determined by age and weight.
Does Linezolid work for meningitis?
Linezolid is believed to penetrate the central nervous system, and has been used in meningitis treatment (35). Imipenem has good central nervous system penetration, but children with meningitis treated with imipenem, had high rates of seizures (meropenem is preferred for meningitis cases and children) (11,36,37). 5.12.
Is amikacin a cross resistance drug?
Amikacin has a lower minimum inhibitory concentration and may be the most efficacious of the two (2), however, clinical comparison is lacking. Capreomycin may have cross-resistance with amikacin/kanamycin if the rrs gene mutation is present, but the clinical implications of this are not well understood.
Why is TB resistant?
The resistance formed can be due to multiple of reasons such as 1) people who have already been diagnosed and are on treatment therapy leaving it halfway 2) using drugs of poor quality for treatment, taking drugs irregularly 3) and coming from areas where drug resistant TB is very common.
What are the other drugs in TB?
Other drugs are second line drugs or reserve TB drugs. Drugs used to treat resistant infections are classified into five groups. The first line drugs are in the first group, besides streptomycin, which is in the second group. All the other drugs are from second line of drugs. Group 1 TB drugs: First Line Oral Agents.
Why is there a nation action plan for tuberculosis?
The need to reverse and hinder the transmission of multidrug resistant tuberculosis throughout the world, prevent any national outbreaks, and maintain decades of investment into public health has lead to building up a Nation Action Plan to fight this disease.
How do you know if you have multidrug resistant?
According to WHO estimates, five percent of all disease cases are in fact multidrug resistant which makes up nearly 480 000 cases and 190 000 deaths each year globally.
How long does it take for a drug resistant tuberculosis test to show clear growth?
Compared to normal drug susceptibility tests for rapidly growing bacteria M. Tuberculosis takes nearly twenty four hours to replicate and a month to show clear growth on solid media.
What is the disease caused by mycobacterium tuberculosis?
Tuberculosis itself is a bacterial infection caused by Mycobacterium tuberculosis. Though lungs are usually the prey of the disease but the bacterium can often attack spine, brain, and kidneys. The drug resistant disease occurs when some bacteria become resistant to the effects of antibiotics or anti TB drugs.
What are the side effects of TB treatment?
A high proportion of patients receiving this kind of treatment can experience side effects like depression, hearing loss, psychosis, hepatitis, and kidney impairment. Average costs of resistant TB treatment increase as the Tuberculosis bacterium resistance grows.
What is XDR TB?
Extensively Drug-resistant TB (XDR TB) Extensively drug-resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). Because XDR TB is resistant to the most potent TB drugs, ...
Why is XDR TB so resistant to TB drugs?
Because XDR TB is resistant to the most potent TB drugs, patients are left with treatment options that are much less effective. XDR TB is of special concern for people with HIV infection or other conditions that can weaken the immune system.
What are some examples of drug resistant TB?
Causes of Drug Resistant TB. Drug-resistant TB can occur when the drugs used to treat TB are misused or mismanaged. Examples of misuse or mismanagement include. People do not complete a full course of TB treatment. Health care providers prescribe the wrong treatment (the wrong dose or length of time)
What is TB resistant?
Treatment of Drug-Resistant TB. Drug-resistant TB is caused by TB bacteria that are resistant to at least one first-line anti-TB drug.
How is TB spread?
TB is spread through the air from one person to another. The TB bacteria are put into the air when a person with TB disease of the lungs or throat coughs, sneezes, speaks, or sings. People nearby may breathe in these bacteria and become infected. Causes of Drug Resistant TB.
What is the disease caused by bacteria that are spread from person to person through the air?
Tuberculosis ( TB) is a disease caused by bacteria that are spread from person to person through the air. TB usually affects the lungs, but it can also affect other parts of the body, such as the brain, the kidneys, or the spine.
Do not take TB drugs?
Do not take their TB drugs regularly. Do not take all of their TB drugs. Develop TB disease again, after being treated for TB disease in the past. Come from areas of the world where drug-resistant TB is common. Have spent time with someone known to have drug-resistant TB disease. Types of Drug Resistant TB.
What is MDR TB?
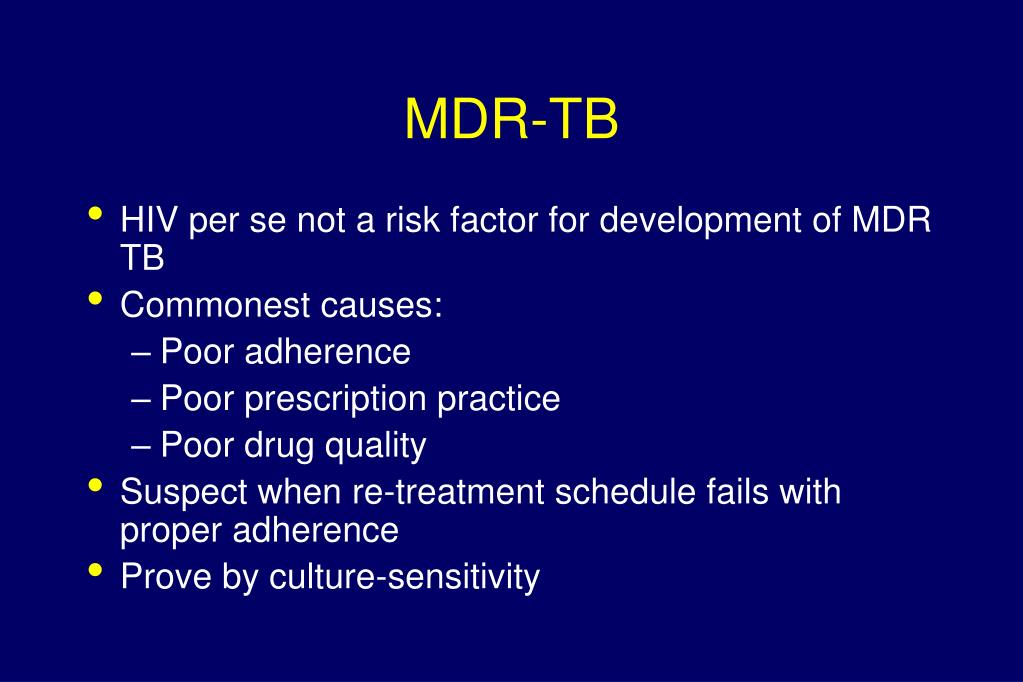
Specialty. Infectious disease. Multidrug-resistant tuberculosis ( MDR-TB) is a form of tuberculosis (TB) infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications (drugs), isoniazid and rifampin. Some forms of TB are also resistant to second-line medications, ...
Why is MDR TB so common?
MDR-TB most commonly develops in the course of TB treatment, and is most commonly due to doctors giving inappropriate treatment, or patients missing doses or failing to complete their treatment. Because MDR tuberculosis is an airborne pathogen, persons with active, pulmonary tuberculosis caused by a multidrug-resistant strain can transmit the disease if they are alive and coughing. TB strains are often less fit and less transmissible, and outbreaks occur more readily in people with weakened immune systems (e.g., patients with HIV ). Outbreaks among non immunocompromised healthy people do occur, but are less common.
What are the hot spots of tuberculosis?
One of the so-called "hot-spots" of drug-resistant tuberculosis is within the Russian prison system. Infectious disease researchers Nachega & Chaisson report that 10% of the one million prisoners within the system have active TB. One of their studies found that 75% of newly diagnosed inmates with TB are resistant to at least one drug; 40% of new cases are multidrug-resistant. In 1997, TB accounted for almost half of all Russian prison deaths, and as Bobrik et al. point out in their public health study, the 90% reduction in TB incidence contributed to a consequential fall in the prisoner death rate in the years following 1997. Baussano et al. articulate that concerning statistics like these are especially worrisome because spikes in TB incidence in prisons are linked to corresponding outbreaks in surrounding communities. Additionally, rising rates of incarceration, especially in Central Asian and Eastern European countries like Russia, have been correlated with higher TB rates in civilian populations. Even as the DOTS program is expanded throughout Russian prisons, researchers such as Shin et al. have noted that wide-scale interventions have not had their desired effect, especially with regard to the spread of drug-resistant strains of TB.
What drugs are resistant to MDR-TB?
MDR-TB can become resistant to the major second-line TB drug groups: fluoroquinolones ( moxifloxacin, ofloxacin) and injectable aminoglycoside or polypeptide drugs ( amikacin, capreomycin, kanamycin ). When MDR-TB is resistant to at least one drug from each group, it is classified as extensively drug-resistant tuberculosis (XDR-TB).
How many deaths from MDR TB in 2016?
MDR-TB caused an estimated 600,000 new TB cases and 240,000 deaths in 2016 and MDR-TB accounts for 4.1% of all new TB cases and 19% of previously treated cases worldwide. Globally, most MDR-TB cases occur in South America, Southern Africa, India, China, and the former Soviet Union.
How many MDR TB cases were there in 2011?
Levels are much higher in those previously treated for tuberculosis - about 20%. WHO estimates that there were about 0.5 million new MDR-TB cases in the world in 2011.
How does TB develop drug resistance?
The TB bacteria has natural defenses against some drugs, and can acquire drug resistance through genetic mutations. The bacteria does not have the ability to transfer genes for resistance between organisms through plasmids ( see horizontal transfer ). Some mechanisms of drug resistance include:
What is MDR TB?
Multidrug-resistant tuberculosis (MDR-TB) is an increasing global problem, with most cases arising from a mixture of physician error and patient non-compliance during treatment of susceptible TB. The extent and burden of MDR-TB varies significantly from country to country and region to region. As with TB itself, the overwhelming burden of MDR-TB is in high-burden resource-poor countries. The diagnosis depends on confirming the drug susceptibility pattern of isolated organisms, which is often only possible in resource-rich settings. There should be a strong suspicion of drug resistance, including MDR-TB, in persons with a history of prior treatment or in treatment failure cases. Treatment in developed countries is expensive and involves an individualized regimen based on drug susceptibility data and use of reserve drugs. In resource-poor settings a WHO retreatment regimen may be used, but increasingly the move is to a directly observed treatment based 'DOTS-plus' regimen in a supported national TB programme. However, even where such treatment is given, the outcome for patients is significantly worse than that for fully susceptible TB and has a much higher cost.
What is treatment in developed countries?
Treatment in developed countries is expensive and involves an individualized regimen based on drug susceptibility data and use of reserve drugs.