
What is the best treatment for STEMI?
Good quality studies have provided strong support for the specific added value of glycoprotein IIb/IIIa inhibitors (especially abciximab), dual antiplatelet therapy (the addition of the thienopyridine, clopidogrel, to aspirin use), and bare-metal stents (BMS), for a broad range of STEMI patients.
What is the pre-hospital care of patients with STEMI?
In ST-elevation myocardial infarction (STEMI) the pre-hospital phase is the most critical, as the administration of the most appropriate treatment in a timely manner is instrumental for mortality reduction. STEMI systems of care based on networks of medical institutions connected by an efficient eme … Pre-hospital treatment of STEMI patients.
What are the causes of STEMI?
Some of those conditions include: Inflammation of the heart or the pericardium (the sac around the heart). Heart problems caused by extreme stress or emotional strain (takotsubo cardiomyopathy, also known as broken heart syndrome). Irregular heart rhythms (arrhythmias). Electrolyte imbalances. Management and Treatment How is STEMI treated?
What are the treatment options for ST-elevation myocardial infarction (STEMI)?
There is general consensus that emergency percutaneous coronary intervention (PCI) is the preferred treatment for patients with ST-elevation myocardial infarction (STEMI), so long as it can be delivered in a timely fashion, by an experienced' operator and cardiac catheterization laboratory (CCL) team.
Why is it important to receive treatment quickly with a myocardial infarction?
A heart attack happens when blood flow to the heart suddenly becomes blocked. Without the blood coming in, the heart can't get oxygen. If not treated quickly, the heart muscle begins to die. But if you do get quick treatment, you may be able to prevent or limit damage to the heart muscle.
Why is STEMI a medical emergency?
A STEMI is a full-blown heart attack caused by the complete blockage of a heart artery. A STEMI heart attack, like a Widow Maker, is taken very seriously and is a medical emergency that needs immediate attention.
Why do we give ASA in the emergency treatment of MI?
A Word From Verywell Aspirin is effective in reducing the blood clots that are blocking a coronary artery during an acute heart attack. Anyone who has already had a heart attack, or who has an increased risk of having one in the future, should always carry a few non-coated adult aspirins with them.
What happens if a STEMI goes untreated?
Left untreated, the mortality rate of STEMI can exceed 30%, and the presence of mechanical complications (papillary muscle rupture, ventricular septal defect [VSD], and free wall rupture) increases the mortality rate to 90%.
Is a STEMI an emergency?
ST-segment myocardial infarction (STEMI) is a time-sensitive emergency that requires swift and seamless integration of prehospital and emergency department resources in order to achieve early diagnosis and reperfusion therapy.
What are the emergency department goals of management for a patient with a STEMI?
The diagnosis of ST‐segment elevation myocardial infarction (STEMI) in the emergency department (ED) is made solely by ECG. Timely diagnosis is critical to achieving timely intervention. The goal is to achieve a door‐to‐ECG time of 10 minutes.
What is the immediate intervention for acute myocardial infarction?
Although the immediate priority in managing acute myocardial infarction is thrombolysis and reperfusion of the myocardium, a variety of other drug therapies such as heparin, β-adrenoceptor blockers, magnesium and insulin might also be considered in the early hours.
What is the benefit of ASA during a suspected AMI?
Aspirin is an effective, inexpensive, and safe treatment of AMI. In 1988, ISIS-2 reported that aspirin therapy reduced short-term mortality in patients with suspected AMI by 23%.
Why do we give aspirin for an MI?
Long-term aspirin therapy reduces the yearly risk of serious vascular events (nonfatal myocardial infarction, nonfatal stroke, or vascular death), which corresponds to an absolute reduction of nonfatal events and to a smaller, but still definite, reduction in vascular death.
Is a STEMI life-threatening?
The bottom line is that STEMI heart attacks are always life-threatening and require quick assessment and treatment.
What is the prognosis for STEMI?
The five-year survival rate for NSTEMI patients was 51%, 42% among women and 57% among men. The five-year survival rate for STEMI patients was 77%, 68% among women and 80% among men. Five year age-adjusted survival rates were higher for STEMI than NSTEMI (logrank: p <0.01).
What is the treatment for STEMI?
The priority in treating a STEMI heart attack is to open the artery quickly, saving as much heart muscle as possible. Treatment options include percutaneous coronary intervention (PCI), a term that encompasses both angioplasty and stenting; clot-busting medication; and coronary artery bypass graft surgery (CABG).
What is PCI in cardiac surgery?
There is general consensus that emergency percutaneous coronary intervention (PCI) is the preferred treatment for patients with ST-elevation myocardial infarction (STEMI), so long as it can be delivered in a timely fashion, by an experienced' operator and cardiac catheterization laboratory (CCL) team. STEMI is both a functional and structural issue.
Does bivalirudin stimulate platelets?
The benefits of both bivalirudin (anti-thrombin drug with efficacy against clot-bound thrombin, which does not appear to stimulate platelets) and abciximab (glycoprotein IIb/IIIa inhibitor which is antibody to platelet receptors), as PCI adjuncts generally, and for STEMI patients, in particular, are supported by multiple trials.
How long does fibrinolysis take for STEMI?
In US and European guidelines in which fibrinolysis is recommended for patients with STEMI if the FMC-to-PPCI delay is >90–120 min, the fact that fibrinolysis is also associated with a delay from FMC is overlooked. PPCI might have an outcome benefit even if the FMC-to-PPCI delay is >120 min, as long as the PCI-related delay is <120 min. To optimize the time to reperfusion, PPCI should be performed as soon as possible. A strategy of prehospital diagnosis of STEMI combined with field triage of patients directly to high-volume PCI centres providing 24-h PCI facilities is recommended to increase the number of patients with STEMI who will benefit from PPCI.
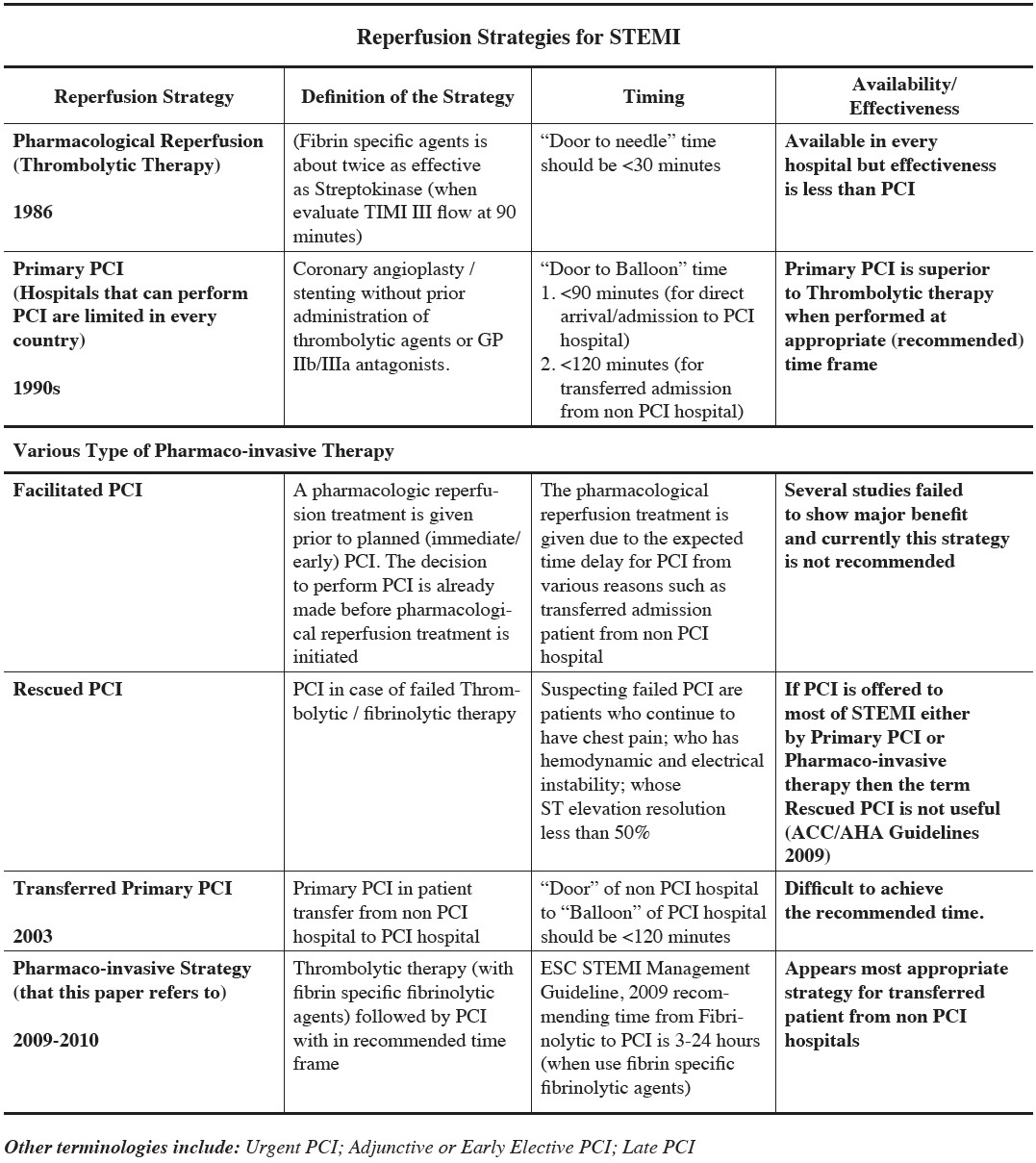
What is the best reperfusion strategy for ST-segment elevation myocardial infarction?
Reperfusion therapy with either fibrinolysis or primary percutaneous coronary intervention (PPCI) is mandatory in patients with ST-segment elevation myocardial infarction (STEMI). 1, 2 According to the European and US guidelines, PPCI is the optimal reperfusion strategy if initiated in a timely fashion. However, the 2011 US guidelines for revascularization of patients with STEMI specifically state that in hospitals where PPCI cannot be performed within 90–120 min after first medical contact (FMC), defined as call to the emergency medical services (EMS) or self-presentation at hospital, fibrinolytic therapy should be the primary reperfusion strategy. 3 In addition, the 2010 ESC guidelines for myocardial revascularization and the 2012 ESC guidelines for the management of acute myocardial infarction in patients with STEMI also indicate fibrinolysis as the first choice of treatment if PPCI cannot be performed within 90–120 min after FMC. 4, 5
What is the delay in reperfusion?
Delay to reperfusion in patients with STEMI is caused by patient delay and health-care system delay ( Figure 1 ). Patient delay is the time from symptom onset until FMC, and health-care system delay is the time from FMC to reperfusion. Health-care system delay can occur at several stages: FMC-to-fibrinolysis delay is the time from FMC to initiation of fibrinolysis, and FMC-to-PPCI delay is the time from FMC to initiation of PPCI. Importantly, percutaneous coronary intervention (PCI)-related delay is the extra time needed to perform PPCI instead of administering fibrinolysis. Door-to-balloon delay is the time from arrival at the PCI-centre until initiation of PCI.
When patients with chest discomfort contact the health-care system, an optimal strategy would be for an ambulance to be dispatche
When patients with chest discomfort contact the health-care system, an optimal strategy would be for an ambulance to be dispatched to the patient immediately, rather than waiting for a primary- care physician to evaluate the patient. When the ambulance services arrive at the scene, acquisition of a prehospital ECG is mandatory. If emergency vehicles are not staffed with physicians or paramedics trained to establish a prehospital diagnosis of STEMI, transmitting the ECG recordings to a hospital-based physician for further analysis is recommended. 40, 41, 42, 43 When a diagnosis of STEMI is confirmed, patients should be rerouted to the nearest interventional hospital for PPCI. In this setting, initial admission to a local hospital has been associated with a 30–50 min extra delay before transfer to the interventional hospital and, therefore, should be avoided. 44 A rerouting strategy, for example one that bypasses the local hospital, would result in a substantial reduction in the cumulative treatment delay, 43, 45 but might mean that patients are transported long distances without being accompanied by a physician. Such a strategy might require the ambulance staff to receive more training than at present. Alternatively, a rendezvous-type strategy is possible, whereby a physician is dispatched to meet the primary ambulance team on route to the interventional centre.
Is fibrinolysis recommended for ST-segment elevation myocardial infarction?
Fibrinolysis is recommended in European and US guidelines for patients with ST-segment elevation myocardial infarction (STEMI) when a strategy of primary percutaneous coronary intervention (PPCI) is associated with ≥120 min delay from first medical contact (FMC), defined as call to the emergency medical services or self-presentation at hospital. Current evidence indicates that reperfusion therapy should be initiated as soon as possible after FMC. However, fibrinolysis cannot be initiated instantaneously at FMC, and PPCI is superior to fibrinolysis in reducing mortality if the extra time needed to perform PPCI instead of fibrinolysis (so-called PCI-related delay) is <120 min. During the past 10 years, the terms 'FMC-to-PPCI delay' and 'PCI-related delay' have been used in guidelines synonymously; however, a distinction should be made between the recommended FMC-to-PPCI delay and the acceptable PCI-related delay. In the future, an ideal recommendation would be to initiate reperfusion as soon as possible, preferably within 120 min of FMC in the case of PPCI. When the expected PCI-related delay is <120 min, PPCI should be the preferred reperfusion strategy, even if the FMC-to-PPCI delay is >120 min. Setting up a health-care system enabling prehospital diagnosis of STEMI with field triage of patients directly to catheterization laboratories at large-volume PCI centres (bypassing local hospitals, coronary care units, emergency departments, and intensive care units) will help to increase the proportion of patients with STEMI who will benefit from PPCI.
What is the role of paramedics in STEMI?
Paramedics and nurses have an important role in pre-hospital STEMI care and their empowerment is essential to increase the effectiveness of the system. Strong cooperation between cardiologists and emergency medicine doctors is mandatory for optimal pre-hospital STEMI care.
What is the prehospital phase of ST-elevation myocardial infarction?
In ST-elevation myocardial infarction (STEMI) the pre-hospital phase is the most critical, as the administration of the most appropriate treatment in a timely manner is instrumental for mortality reduction. STEMI systems of care based on networks of medical institutions connected by an efficient emergency medical service are pivotal. The first steps are devoted to minimize the patient's delay in seeking care, rapidly dispatch a properly staffed and equipped ambulance to make the diagnosis on scene, deliver initial drug therapy and transport the patient to the most appropriate (not necessarily the closest) cardiac facility. Primary PCI is the treatment of choice, but thrombolysis followed by coronary angiography and possibly PCI is a valid alternative, according to patient's baseline risk, time from symptoms onset and primary PCI-related delay. Paramedics and nurses have an important role in pre-hospital STEMI care and their empowerment is essential to increase the effectiveness of the system. Strong cooperation between cardiologists and emergency medicine doctors is mandatory for optimal pre-hospital STEMI care. Scientific societies have an important role in guideline implementation as well as in developing quality indicators and performance measures; health care professionals must overcome existing barriers to optimal care together with political and administrative decision makers.
