Treatment after three weeks of illness is unlikely to help. The bacteria are gone from your body by then, even though you usually will still have symptoms. This is because the bacteria have already done damage to your body.
Full Answer
When should I be treated for pertussis?
Treatment after three weeks of illness is unlikely to help. The bacteria are gone from your body by then, even though you usually will still have symptoms. This is because the bacteria have already done damage to your body. There are several antibiotics (medications that can help treat diseases caused by bacteria) available to treat pertussis.
How serious is pertussis?
Mar 30, 2016 · Several factors have been attributed to the increase in incidence rates and the shift in the epidemiology of pertussis, including lower immunization rates among adolescents and adults, waning immunity after receipt of acellular pertussis vaccines, an increase in the awareness of pertussis by health care providers caring for adolescents and adults, …
How useful are antimicrobials in the treatment of pertussis?
Dec 15, 2021 · If you have had pertussis for three weeks or more, antibiotics will not be prescribed because the bacteria are already gone from your body. At this point, your symptoms will slowly improve on their own, but your doctor will want to address any other damage done to your body while you were sick.
What is the prognosis of B pertussis without treatment?
Aug 01, 2021 · Antibiotic treatment is intended to prevent transmission of pertussis to others and does not shorten the disease course or improve symptoms. ... does not …

How effective is pertussis treatment?
Treat appropriately for pertussis. Because pertussis may progress rapidly in young infants, treat suspected and confirmed cases promptly. However, treatment is ineffective if started late in the course of illness.
What happens if pertussis is left untreated?
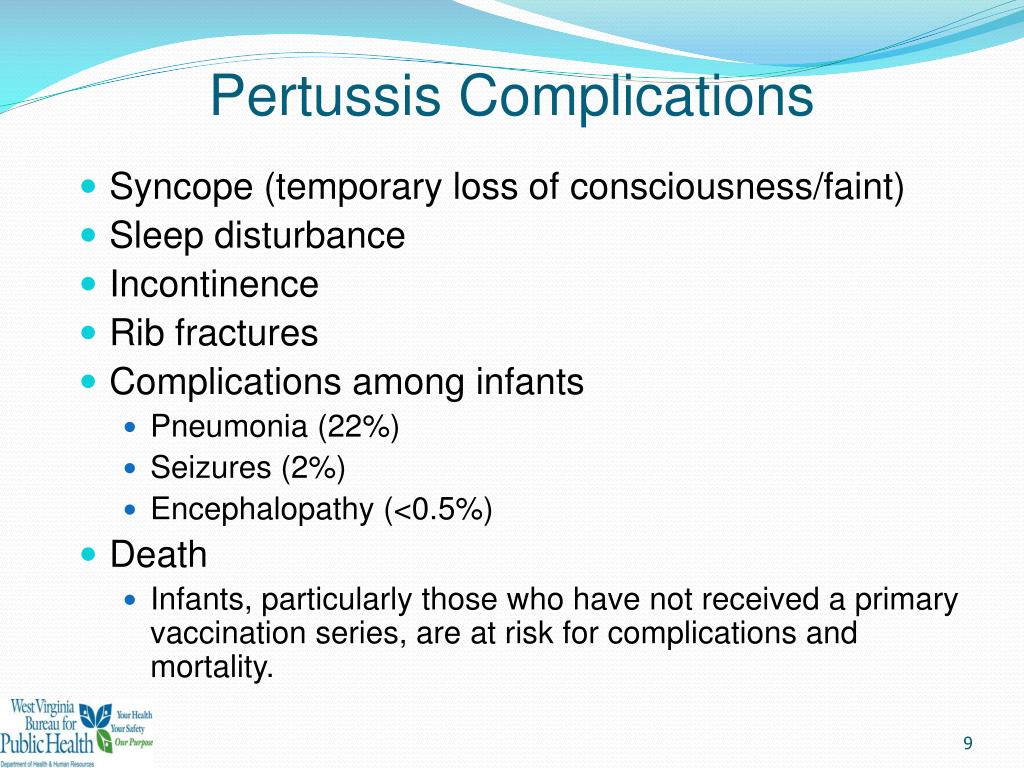
Complications of whooping cough are more common in infants and young children. They may include pneumonia, middle ear infection, loss of appetite, sleep disturbance, fainting, dehydration, seizures, altered brain function (encephalopathy), brief periods when breathing stops and death.
What is the most common complication of pertussis vaccine?
Clinical Complications68% will have apnea.23% get pneumonia.1.2% will have seizures.1% will die.0.4% will have encephalopathy (as a result of hypoxia from coughing or possibly from toxin)
How long does it take to get rid of pertussis?
Duration. Pertussis usually causes prolonged symptoms — 1 to 2 weeks of common cold symptoms, followed by up to 3 months of severe coughing. The last stage consists of another few weeks of recovery with gradual clearing of symptoms. In some children, the recovery period can last for months.
Can whooping cough permanently damage your lungs?
As symptoms progress, complications may occur, particularly in infants, who can be subject to pneumonia, heart failure, collapsed lung, brain bleeds and even death. In older children and adults, coughing spells may result in loss of bladder control and retching and vomiting, leading to rib fracture.Aug 31, 2021
Can pertussis cause permanent damage?
Children who survive a severe case of pertussis can suffer from long-term health and developmental problems, researchers reported in September.
When should you be hospitalized for pertussis?
Infants with pertussis, especially younger than 6 months, often require hospitalization for supportive care for coughing spasms and feeding difficulties (3). Complications can include pneumonia, encephalopathy, seizures, and death (3).
Can whooping cough last for years?
Once infected, whooping cough lasts from three to six months with treatment. With the proper treatment, most people recover and have no lasting effects. Whooping cough, also called pertussis, is a highly infectious disease that you may pass on without even knowing you have it.Feb 18, 2021
What are the 3 stages of pertussis?
Pertussis is a highly contagious acute respiratory disease caused by the bacteria Bordetella pertussis. This disease has 3 stages: catarrhal, paroxysmal, and convalescent.
Can whooping cough be chronic?
pertussis infection is a common cause of persistent cough in adults. This is of concern, because these patients may be B. pertussis reservoirs from which transmission may occur to infants, in whom the disease can be devastating.
When does whooping cough peak?
Q: Why are reported cases of pertussis increasing? A: Since the early 1980s, there has been an overall trend of an increase in reported pertussis cases. Pertussis is naturally cyclic in nature, with peaks in disease every 3 to 5 years.
What is the pathogen that causes pertussis?
Pertussis, also known as whooping cough, is a highly contagious respiratory disease. It is caused by the bacterium Bordetella pertussis.
How long does it take for pertussis to get out of your system?
They remain infectious through the third week after the onset of paroxysms (multiple, rapid coughs) or until 5 days after the start of effective antimicrobial treatment.
What antimicrobials are used for pertussis?
The recommended antimicrobial agents for treatment or chemoprophylaxis of pertussis are. Clinicians can also use Trimethoprim-sulfamethoxasole. Clinicians should choose the antimicrobial after consideration of the.
What is the CDC's goal for postexposure antibiotics?
CDC supports targeting postexposure antibiotic use to persons at high risk of developing severe pertussis and to persons who will have close contact with those at high risk of developing severe pertussis. Learn more about use of PEP.
How long before coughing paroxysms occur?
If a patient starts treatment for pertussis early in the course of illness, during the first 1 to 2 weeks before coughing paroxysms occur, symptoms may be lessened. Clinicians should strongly consider treating prior to test results if clinical history is strongly suggestive or patient is at risk for severe or complicated disease (e.g., infants). ...
How long to close contacts with antibiotics?
Administer a course of antibiotics to close contacts within 3 weeks of exposure, especially in high-risk settings. Use the same doses as in the treatment schedule. Early empiric treatment is important for infants.
How long after a cough can you treat?
A reasonable guideline is to treat persons older than 1 year of age within 3 weeks of cough onset and infants younger than 1 year of age and pregnant women (especially near term ) within 6 weeks of cough onset.
Is azithromycin safe for infants?
However, azithromycin remains the drug of choice for treatment or prophylaxis of pertussis in very young infants because the risk of developing severe pertussis and life-threatening complications outweigh the potential risk of IHPS.
How to stop vomiting from a syringe?
Supportive care, such as plenty of rest and fluids, can ease symptoms. Eating small, frequent meals can help prevent vomiting. It may also be helpful to rid your home of any irritants that could trigger coughing, such as smoke, dust and chemical fumes.
Why do we need booster shots?
Booster shots may be needed throughout life to ensure that your immunity remains intact.
How to contact the lung association?
If you would like to talk to a trained respiratory professional who can help answer your questions or connect you with additional support, call the Lung Association's Lung HelpLine at 1-800-LUNGUSA.
Can antibiotics help with pertussis?
Because the risk of pertussis transmission is so high, if you or someone in your family has pertussis, your doctor will likely suggest that everyone in the household is treated with antibiotics. Like many other illnesses, having good health habits can reduce the spread of pertussis.
How long does it take to get rid of pertussis?
Pharmacologic treatment of pertussis consists of antibiotics. Treatment is recommended within 3 weeks of symptom onset. 9 The timing of antibiotic administration plays a role in the antibiotic’s effect. Administration during the initial phase—particularly within the first 7 days of symptom onset—may reduce symptom severity and duration, whereas later administration serves merely to reduce the risk of transmission. 1,4 The majority of patients receiving antimicrobial therapy for pertussis do not experience substantial relief of clinical symptoms. 8 There is no evidence that antimicrobial treatment leads to reduced mortality or prevents serious complications such as pneumonia; the main benefit is the reduced risk of transmission to other people due to more rapid eradication of B pertussis from the nasopharynx. 1,4,8,10
How long does it take for a cough to go away?
4 Therefore, pertussis should be suspected in any patient presenting with a cough that has persisted for more than 3 weeks. Other concomitant symptoms with cough are diaphoresis and syncope.
What is the best way to prevent infection in adults?
Infection prevention in adults is managed through scheduled vaccination with tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap). Pharmacists are accessible sources of immunization education and administration, and they can impact infection outcome in patients through timely referrals for antimicrobial treatment ...
Why do women need booster shots?
Although pertussis tends to be less severe in adults, booster vaccinations are critical for maintaining herd immunity and preventing the spread of infection , particularly to children. A booster is recommended during each of a woman’s pregnancies to confer temporary immunity to the infant.
What is the role of a pharmacist?
The pharmacist’s role as a disseminator of information regarding the importance of vaccination and its proper timing is crucial for disease-prevention advocacy . Additionally, pharmacists can serve as accessible sources of vaccine administration within the community.
Is coughing a symptom of pertussis?
In fact, a persistent cough may be the only symptom in adults and adolescents. Because the symptoms are nonspecific, providers may overlook pertussis as the source of infection in these patients. 1. Rates of pertussis in the United States have increased steadily since the 1980s, peaking at 48,277 cases reported to the CDC in 2012—the highest ...
Is azithromycin better than clarithromycin?
Conversely, azithromycin and clarithromycin are better tolerated, have similar efficacy, and possess simpler dosing regimens (once daily for 5 days and twice daily for 7 days, respectively). 1,9 Common adverse effects of macrolides include nausea, vomiting, and diarrhea. 8,9.
EVIDENCE SUMMARY
The key clinical features of the initial catarrhal stage are difficult to distinguish from a viral upper respiratory tract infection and include malaise, rhinorrhea, dry cough, and lacrimation. Fever is usually mild or absent. After one to two weeks, the paroxysmal stage may manifest.
EVIDENCE SUMMARY
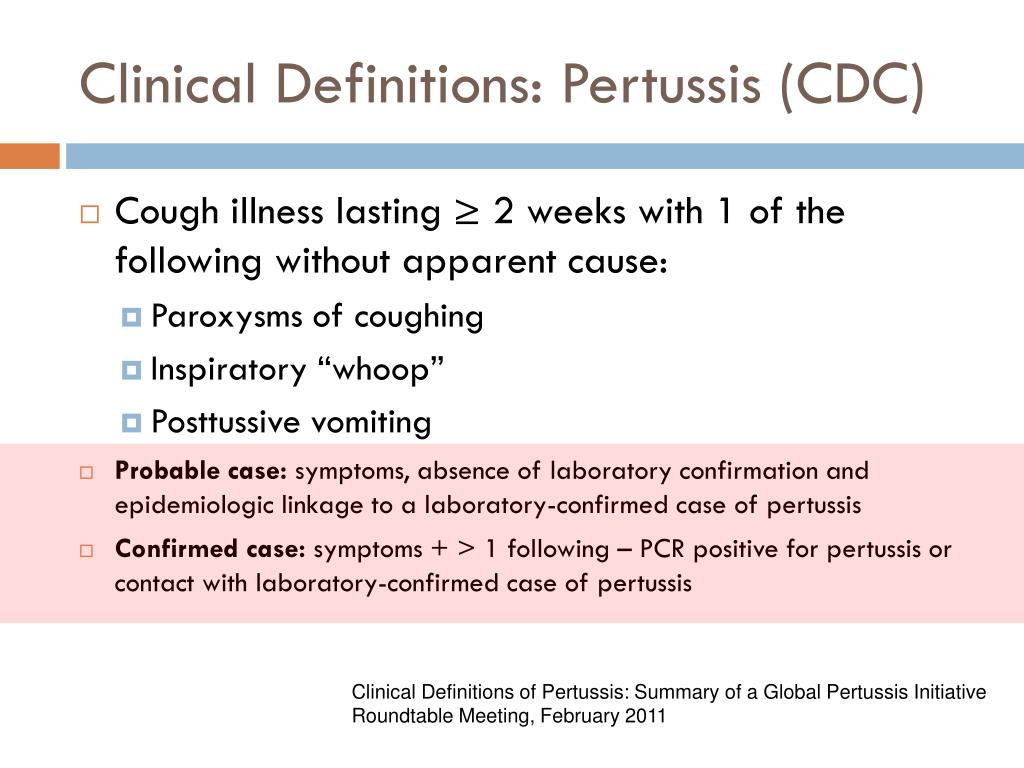
No validated, accepted clinical decision rule has been established for diagnosing pertussis. 13 However, the key clinical features of the infection are included in CDC and World Health Organization (WHO) case definitions.
EVIDENCE SUMMARY
The sensitivities of culture and PCR are highest during the catarrhal and early paroxysmal phase, whereas the sensitivity of serology (immunoglobulin G) does not peak until late in the paroxysmal and convalescent phases ( Table 3).
EVIDENCE SUMMARY
Unlike with other vaccines, there is not a standardized antibody titer to confirm protection against pertussis.
EVIDENCE SUMMARY
Because of the increasing incidence of pertussis in the United States and an observed waning immunity regardless of the source of inoculation (whole cell or acellular vaccine or infection), the CDC's Advisory Committee on Immunization Practices (ACIP) published updated pertussis vaccination guidelines in 2005, including introducing a booster of Tdap, rather than tetanus and diphtheria toxoids (Td), at 11 to 12 years of age or once as an adult if not previously received.
EVIDENCE SUMMARY
There is no difference in adverse effects in patients given Td or Tdap at an interval of five to 10 years, and data in pregnant patients given multiple doses in shorter time spans also have not shown an increase in adverse effects.
EVIDENCE SUMMARY
Immunization should be temporarily delayed in a patient who has uncontrolled seizure disorder or a progressing neurologic disorder, such as infantile spasms, until the disorder is stabilized.
Why do people get whooping cough?
Whooping cough is caused by Bordetella pertussis bacteria. An effective vaccine has been available for 70 years, and because of its widespread use among children, there are now far fewer cases and deaths from the disease.
What should a whooping couph eat?
A whooping couph should do away from all foods which produce phlegm like milk, ghee, sweets, rice, refined flour products, sugar and lentils. His diet should consist of oranges, musk melon, tomatoes and rasberry. Vegetables like spinch, cabbage, gourds, should be taken in a boiled form without addition of any condiments.
Does pertussis fade with time?
Here is what the CDC has to say on the subject: Vaccine protection for pertussis, tetanus, and diphtheria can fade with time. Before 2005, the only booster vaccine available contained tetanus and diphtheria (called Td), and was recommended for adolescents and adults every 10 years.
Is the CDC relaxed?
The CDC has relaxed some prevention measures, particularly for people who are fully vaccinated, and especially outdoors. Meanwhile, scientists continue to explore treatments and to keep an eye on viral variants. Stay Informed. View Coronavirus COVID-19 Resource Center.
Can you have pertussis if you can't shake?
First, if you have a bad cough that you can’t shake, it’s possible that you have pertussis. By some estimates, 10% to 30% of prolonged coughs in adults are caused by pertussis. Mind you, there seem to be swings in the number of new cases each year, so those estimates might be high in a low incidence year.
How long does it take for a pertussis case to become non-infectious?
Cases will become noninfectious after completing 5 days of antibiotic treatment. Treatment initiated more than 3 weeks after onset of illness is of no value because viable organisms are no longer present. In certain situations, close contacts of pertussis cases may be treated with antimicrobials to prevent infection.
How long does it take to initiate prophylaxis?
Prophylaxis should be initiated as soon as possible within 21 days (the maximum incubation period for pertussis) of exposure to an infectious case. Special emphasis for prophylaxis should be placed on: Household members.
How long does azithromycin last?
Azithromycin [ 1, 4] (3-day course not yet approved for treatment of pertussis) 1-5 months: 10 mg/kg/day orally daily for 5 days. <1 month of age: same as above and is the preferred choice for infants <1 month old.
How long does SMX last?
8 mg TMP/40 mg SMX/kg/day orally divided into 2 doses/day for 14 days (maximum 320mg TMP/1600mg SMX/ day) 320 mg TMP/1600 mg SMX per day orally divided into 2 doses/day for 14 days. 1. FDA Pregnancy Category B drug.
Etiology
Clinical Presentation and Diagnosis
- The recommended antimicrobial agents for treatment or chemoprophylaxis of pertussis are 1. Azithromycin* 2. Clarithromycin 3. Erythromycin Clinicians can also use Trimethoprim-sulfamethoxasole. Clinicians should choose the antimicrobial after consideration of the 1. Potential for adverse events and drug interactions 2. Tolerability 3. Ease of adher...
Treatment
Postexposure Prophylaxis
Symptomatic Treatment
- Both the CDC and the World Health Organization define a clinical case of pertussis as a cough lasting for 2 weeks with one classic symptom, such as paroxysmal cough, posttussive emesis, or inspiratory whoop, without any other apparent causes. Although prolonged cough is a hallmark of pertussis, diagnosis should be based on a combination of clinical presentation and laboratory m…
Prevention
- Pharmacologic treatment of pertussis consists of antibiotics. Treatment is recommended within 3 weeks of symptom onset.9 The timing of antibiotic administration plays a role in the antibiotic’s effect. Administration during the initial phase—particularly within the first 7 days of symptom onset—may reduce symptom severity and duration, whereas late...
Conclusion
- After the risks versus benefits of antimicrobial therapy have been evaluated, postexposure prophylaxis may be administered within 21 days of exposure to an individual infected with B pertussis. Persons who are immunocompromised, have a chronic pulmonary condition, or are in close contact with infants are at high risk for pertussis and should receive prophylactic treatmen…