How are benzodiazepines used to treat organophosphates?
In severe cases, doctors often prescribe benzodiazepines to prevent or stop seizures. If you have been exposed to organophosphates in small doses and don’t need to be hospitalized, you may administer a low dose of atropine to yourself using a commercially prepared injection:
What is the treatment for organophosphate toxicity?
Treatment Termination of the exposure including removing all soiled clothing. Gently cleanse with soap and water to hydrolyze organophosphate solutions. Airway control and adequate oxygenation. Intubation may be necessary in cases of respiratory distress due to laryngospasm, bronchospasm, bronchorrhea, or seizures.
What is organophosphate (OP) poisoning?
Organophosphate (OP) poisoning is a complex clinical condition. Increased acetylcholine (ACh) concentration in the cholinergic synapses attributable to acetylcholinesterase (AChE) inhibition leads to altered signaling in these synapses, causing various pathological effects, including failure of respiratory muscles and cardiac arrhythmias.
What is the mechanism of action of organophosphates?
Organophosphates are also used in ophthalmology – echothiopate is used to treat glaucoma. Organophosphate mechanism of toxicity: Acetylcholinesterase inhibitors that form a stable irreversible covalent bond to the enzyme.
Which is the most important drug in the treatment of organophosphate poisoning?
The definitive treatment for organophosphate poisoning is atropine, which competes with acetylcholine at the muscarinic receptors. The initial dose for adults is 2 to 5 mg IV or 0.05 mg/kg IV for children until reaching the adult dose.
Why do we give atropine in organophosphorus poisoning?
Atropine is administered intravenously to restore adequate cardiorespiratory function rapidly – a process often termed 'atropinzation'. It is used to reverse bradycardia and improve systolic blood pressure to greater than 80 mmHg.
Why is oximes used in organophosphorus poisoning?
The main therapeutic effect of pralidoxime is predicted to be recovery of neuromuscular transmission at nicotinic synapses. In vitro experiments have shown that oximes are effective reactivators of human AChE inhibited by OP compounds.
What is the antidote for organophosphate exposure called?
Sometimes, a drug called atropine is used as an organophosphate antidote to help stabilize your breathing. Another medication called pralidoxime can reduce neuromuscular symptoms.
Why pralidoxime is used in OPC poisoning?
Pralidoxime is an effective antidote for organophosphate poisoning only if the antidote is administered before the “aging” process (i.e., within 24 hours of exposure), which stabilizes the organophosphate-enzyme complex.
Why is atropine given before pralidoxime?
Because pralidoxime is less effective in relieving depression of the respiratory center, atropine is always required concomitantly to block the effect of accumulated acetylcholine at this site.
Why oximes are not used in carbamate poisoning?
The administration of oximes, acetylcholinesterase reactivators, in carbamate poisoning is controversial because of the potential toxicity of oximes in conjunction with carbamate especially in the case of the carbamate--"carbaryl" poisoning. However, recent data suggest that this concern may be unwarranted.
What do oximes do?
Oximes are the second important antidote in the treatment of nerve agent poisoning. Their primary role is to reactivate AChE after it has been phosphorylated by a nerve agent by removing the nerve agent from its active site.
What is the function of pralidoxime?
Pralidoxime is a medication used in the management and treatment of organophosphate poisoning. It is in the oxime class of drugs. This activity outlines the indications, action, and administration of pralidoxime therapy as a valuable agent in managing the toxicity of organophosphate-based pesticides and nerve agents.
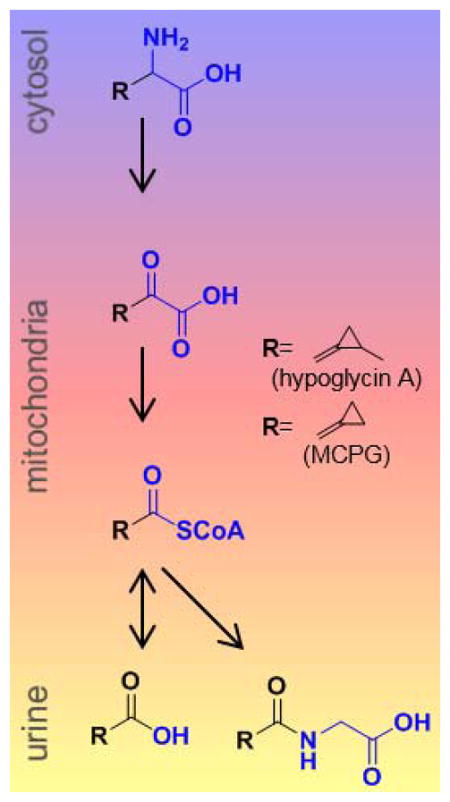
How do organophosphates affect the nervous system?
Upon entering the body—through ingestion, inhalation, or contact with skin—organophosphates inhibit cholinesterase, an enzyme in the human nervous system that breaks down acetylcholine, a neurotransmitter that carries signals between nerves and muscles.
What is pralidoxime used for?
Used as an antidote to reverse muscle paralysis resulting from OP AChE pesticide poisoning but is not effective once the OP compound has bound AChE irreversibly (aged).
Why is atropine used in intubation?
Intubation may be necessary in cases of respiratory distress due to laryngospasm, bronchospasm, bronchorrhea, or seizures. Immediate aggressive use of atropine may eliminate the need for intubation.
What is the best treatment for organophosphate poisoning?
The mainstays of medical therapy in organophosphate (OP) poisoning include atropine, pralidoxime (2-PAM), and benzodiazepines (eg, diazepam). Initial management must focus on adequate use of atropine. Optimizing oxygenation prior to the use of atropine is recommended to minimize the potential for dysrhythmias.
What is the endpoint of atropinization?
The endpoint for atropinization is dried pulmonary secretions and adequate oxygenation. Tachycardia and mydriasis must not be used to limit or to stop subsequent doses of atropine. The main concern with OP toxicity is respiratory failure from excessive airway secretions.
Does OP poisoning deplete atropine?
A severe OP pesticide poisoning case has been known to deplete a hospital’s supply of atropine. Data from the sarin attack on the Tokyo subway suggest that patients poisoned by nerve agents require much less atropine than those poisoned by OP pesticides.
Can glycopyrrolate be used for muscarinic toxicity?
If atropine is unavailable or in limited supply, intravenous glycopyrrolate or diphenhydramine may provide an alternative anticholinergic agent for treating muscarinic toxicity; however, glycopyrrolate does not cross the blood-brain barrier and cannot treat central effects of OP poisoning.
What are the complications of organophosphate poisoning?
These include: metabolic disorders, such as hyperglycemia (high blood sugar) and glycosuria (excess sugar in urine) diabetic ketoacidosis, in which your blood produces excess blood acids. pancreatitis, or inflammation of the pancreas. cancer.
How do you get organophosphate poisoning?
You can also get organophosphate poisoning by consuming contaminated food or water. The most common unintentional exposure routes are through breathing and contact with the skin.
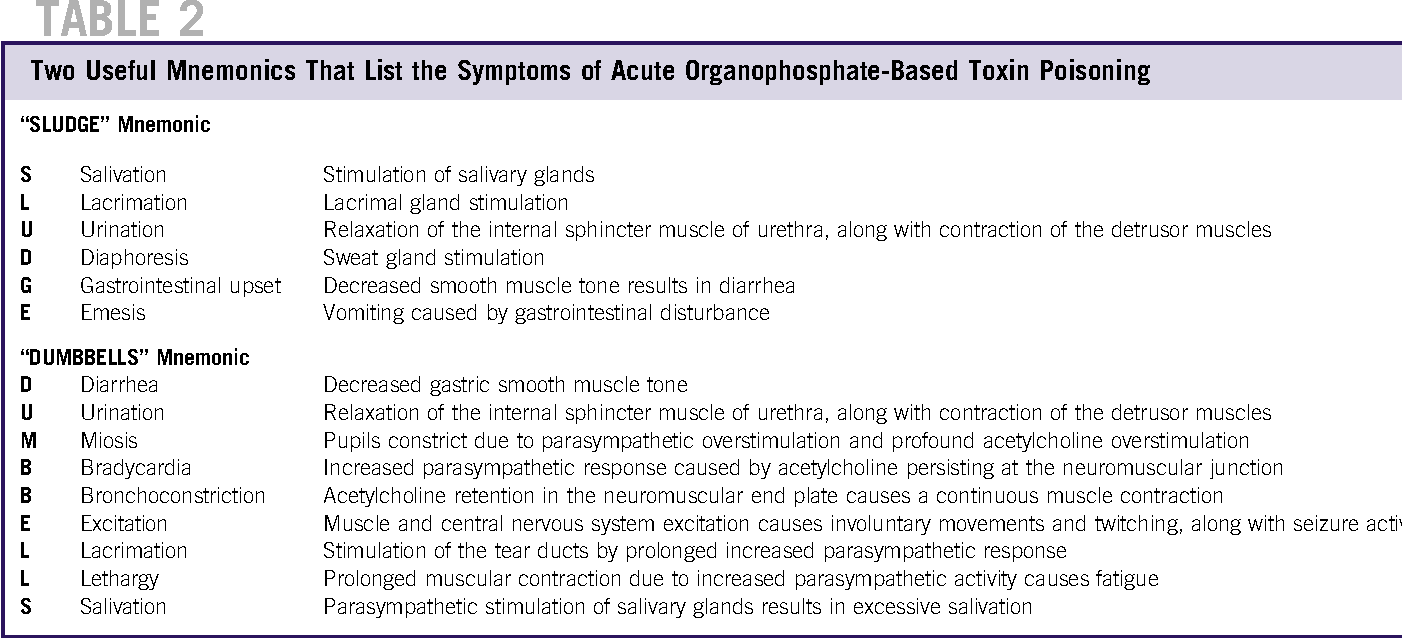
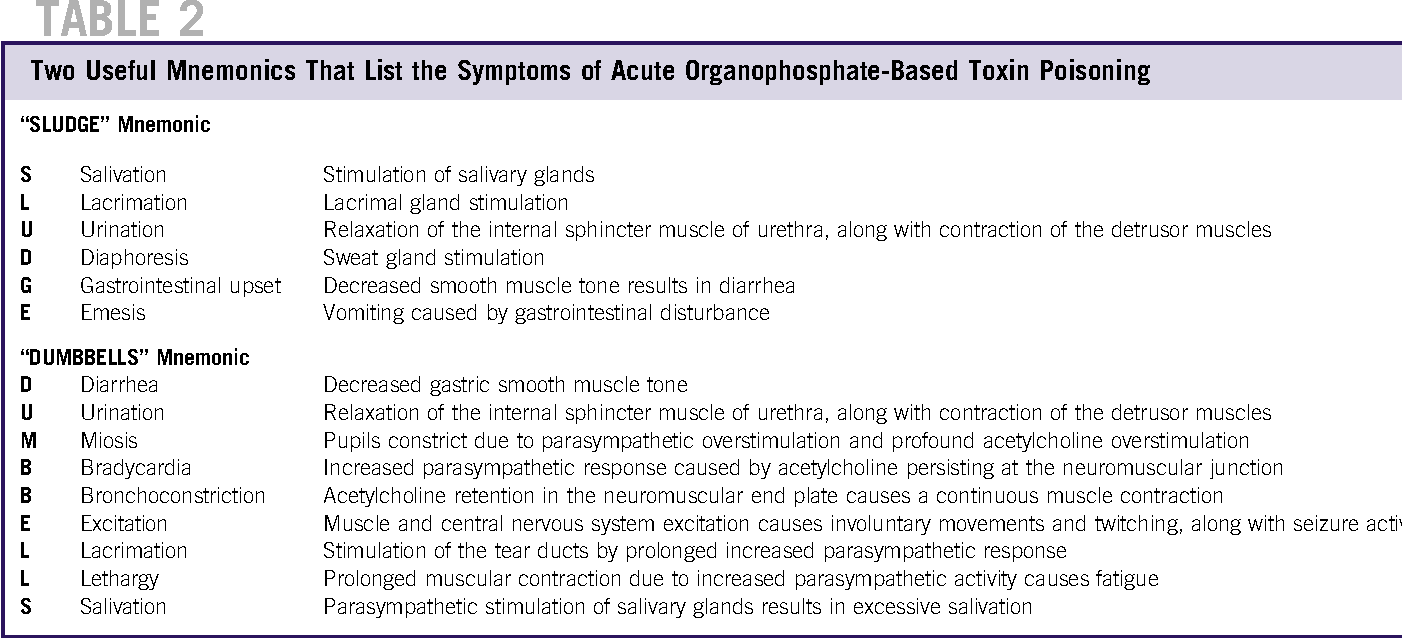
How long does it take for organophosphate poisoning to show symptoms?
What are the symptoms of organophosphate poisoning? Organophosphate poisoning can be short- or long-term. It can be caused by large or small doses. The longer the exposure and the larger the dose, the more toxic the effects. Symptoms can occur within several minutes or hours of exposure.
What is the color of organophosphate?
Organophosphates are typically colorless-to-brown liquids at room temperature. Some may be unscented, while others have a fruit-like smell. say as many as 25 million agricultural workers across the developing world have at least one episode of organophosphate poisoning per year.
Can organophosphates harm animals?
Organophosphates are a common class of insecticides. But large doses of organophosphates can also harm people and other animals. Organophosphate poisoning can occur when you’re exposed to them for too long or at high levels.
How long does it take for organophosphate poisoning to cause seizures?
Organophosphate poisoning may cause significant morbidity and mortality due to seizure activity. Organophosphates (i.e., nerve agents) induce seizures that progress through three stages. The first 5 minutes of exposure precipitates seizures due to cholinergic overstimulation. During this period, agents with central anticholinergic properties can abort or prevent these seizures. Beyond 5 minutes of exposure, other changes are noted, such as decreased brain norepinephrine levels, increased glutaminergic response, and NMDA receptor activation. In this mixed cholinergic and noncholinergic stage, anticholinergic treatment alone will not terminate seizures. Seizure activity continuing 40 minutes after exposure is mediated by noncholinergic mechanisms and results in structural neuronal injury that is difficult to stop with pharmaceutical agents.58–60
What is OP poisoning?
Organophosphate (OP) poisoning is a complex clinical condition. Increased acetylcholine (ACh) concentration in the cholinergic synapses attributable to acetylcholinesterase (AChE) inhibition leads to altered signaling in these synapses, causing various pathological effects, including failure of respiratory muscles and cardiac arrhythmias. Hypoxia that develops as a combination of impaired exchange of gases in the lungs and bradycardia is an especially threatening complication. However, there is now substantial evidence that inhibition of AChE is not the exclusive mechanism underlying a wide variety of adverse consequences of OP exposure described previously ( Terry, 2012 ). It is known that cholinesterases (ChEs) are not the only targets of OPs and that various intracellular mechanisms are modified because of direct or indirect OP actions ( Jett and Lein, 2006; Terry, 2012; Lima et al., 2013 ). For instance, DNA microarray analysis of cells treated with OP diazinon disclosed overwhelming modulation (upregulation or downregulation) of a wide range of genes ( Mankame et al., 2006 ). Although still poorly understood, such noncholinergic OP actions might directly or indirectly modify functioning of the complex intracellular mechanisms and importantly contribute to the effects of OP poisoning.
What happens if you have OP poisoning?
Severe OP poisoning can result in respiratory failure with arterial oxygen partial pressures below 50–60 mm Hg (6.65–7.99 kPa) ( Tsao et al., 1990 ). In such circumstances peripheral tissues, including skeletal muscle, become extremely hypoxic which might have an important effect on the cellular precursors of human muscle regeneration. As known from the extensive studies in other systems, central to the cellular response to hypoxia is hypoxia-inducible factor-1 (HIF-1), a heterodimeric transcription factor, consisting of an oxygen-regulated α-subunit (HIF-1α) and an oxygen-independent β-subunit (HIF-1β). HIF-1α, which is normally almost undetectable due to its continuous degradation in the ubiquitin–proteosome pathway, rapidly accumulates in hypoxia and translocates to the nucleus where it dimerizes with HIF-1β to form a functional transcription factor that controls expression of hundreds of genes ( Manalo et al., 2005; Semenza, 2007a ). Through its effects on gene expression HIF-1 not only increases oxygen delivery to hypoxic tissues by stimulating erythropoiesis and angiogenesis but also promotes cell survival by redirecting cellular energy metabolism towards glycolysis (Pasteur effect) ( Seagroves et al., 2001; Semenza, 2007b ). Due to its central role in response to hypoxia, we tested whether such adaptation also takes place in human myoblasts in vitro. We exposed human myoblasts to acute hypoxia (1% O 2, 4 h) and found a 6.2-fold increase in HIF-1α level compared to normoxic control ( Figure 45.4 ). This means that human myoblasts respond to hypoxia in a similar fashion to other cell types. Investigations are under way in our laboratory with the aim of finding out whether myoblast response by increased HIF-1α leads to modifications in IL-6 secretion and in this way also in muscle regeneration.
How long after cholinesterase injection can you administer a cholinesterase inhibitor?
Do not administer within 2 days of administration of a cholinesterase-inhibiting drug. Use a split-dosage schedule in animals that are old, heavily parasitized, anemic, or otherwise debilitated. Do not use in young foals, kittens, or puppies less than 2 pounds.
Does diazepam help with seizure?
Ongoing seizure activity is due to subsequent glutamate release and is not responsive to atropine. Diazepam, which is known to potentiate effects of gamma-aminobutyrate (GABA) and facilitate inhibitory GABA neurotransmission, has been effectively used for control of OP poisoning.
Can OP poisoning cause seizures?
Seizures from OP poisoning are rare. Although seizures are more commonly associated with the chemical nerve agents, in one case series of pesticide poisoning seizures occurred in as many as 13% of patients.162 Seizures from OP poisoning are thought to be initiated by increased ACh levels and are atropine-responsive.
Does OP poisoning cause polyneuropathy?
OP poisoning may lead to delayed polyneuropathy, which is thought to result from inhibition of neuropathy target esterase (NTE) ( Glynn, 2006; Richardson et al., 2013; Johnson, 1969a,b ). NTE-related esterase (NRE, PNPLA7), a trans -membrane serine esterase linked to the endoplasmic reticulum, has been identified as a member of the patatin domain-containing enzymes family ( Kienesberger et al., 2008 ). Several isoforms of NRE were detected in different stages of skeletal muscle regeneration in vitro ( Fig. 49.6A ). Notably, the 150 kDa isoform was markedly upregulated on fusion of myoblasts into myotubes, suggesting NRE might have a role in differentiation of myogenic precursors. NRE activity was decreased in human myoblasts exposed to DFP ( Fig. 49.6B ). Taken together, these results indicate that OPs may impair myogenesis via NRE inhibition. Inhibition of NRE may represent a novel mechanism underlying OP poisoning-related myopathy.