Why is it so difficult to manage medical claims?
Managing medical claims effectively is an extremely complex task. Each process has numerous steps and variations which makes it difficult for insurers to bring about consistent improvements in the claims operations.
How can you make a success out of medical claims processing?
From improving your accuracy and productivity to preventing operational issues and errors, here is how you can make a success out of medical claims processing. Electronic claims process in one-third the time required for paper claims.
How can medical insurers reduce claims processing expenses?
Medical Insurers also need to find a better way of reducing claims processing expenses as insurance payouts forms a substantial part of an insurer’s costs. But an insurance policy holder’s service needs and their right to receive an equitable and fair settlement must never be compromised for cost efficiencies.
Why is my health insurance claim taking so long to process?
Especially when you have to work through phone menus require you to enter insurance ID’s, provider ID’s, dates of service, etc. Many reoccurring health claim processing errors fall into the “80/20” rule which means that 80% of your problems are caused by 20% of the coding.

How are medical claims processed?
How Does Claims Processing Work? After your visit, either your doctor sends a bill to your insurance company for any charges you didn't pay at the visit or you submit a claim for the services you received. A claims processor will check it for completeness, accuracy and whether the service is covered under your plan.
What does it mean to process medical claims?
In essence, claims processing refers to the insurance company's procedure to check the claim requests for adequate information, validation, justification and authenticity. At the end of this process, the insurance company may reimburse the money to the healthcare provider in whole or in part.
What is the purpose of a medical claim?
A medical claim is a bill that healthcare providers submit to a patient's insurance provider. This bill contains unique medical codes detailing the care administered during a patient visit. The medical codes describe any service that a provider used to render care, including: A diagnosis.
What is the first key to successful claims processing?
Insurance companies usually have no time limits for filing appeals. What is the first key to successful claims processing? provider's office. HIPAA has developed a transaction that allows payers to request additional information to support claims.
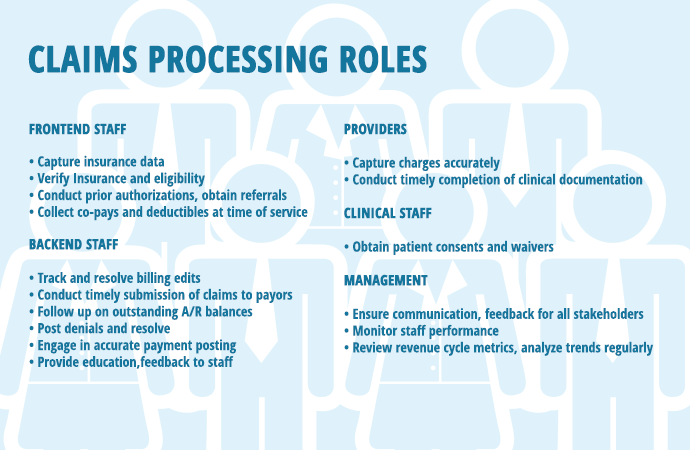
Who processes the medical claims?
Clearinghouses: The next step in medical claim billing is clearinghouses to which processed claims are sent to. It is a third-party hub that operates between the Provider and the Payor. Clearinghouses sort out all claims, scrub them for errors, format as per industry standards, and send to various insurance carriers.
How do you improve claims handling?
5 proven Ways to Improve Claims Management ProcessPreserve and Refresh Patient Data. Accurate patient data is the key to obtaining best coverage limits. ... Train and Retrain Agents to File Claims Without Error. ... Streamline Healthcare Claims Denial Management. ... Analyze Quality Control Measures. ... Investigate Faulty Claims.
What are the 3 most important aspects to a medical claim?
Three important aspects of medical billing are claims validation, the migration of crucial software from local servers to cloud computing service providers and staying current on codes.Claims Validation. ... Cloud Computing. ... Codes and Compliance.
What are the types of medical claims?
The two most common claim forms are the CMS-1500 and the UB-04. These two forms look and operate similarly, but they are not interchangeable. The UB-04 is based on the CMS-1500, but is actually a variation on it—it's also known as the CMS-1450 form.
How do you process an insurance claim?
Your insurance claim, step-by-stepConnect with your broker. Your broker is your primary contact when it comes to your insurance policy – they should understand your situation and how to proceed. ... Claim investigation begins. ... Your policy is reviewed. ... Damage evaluation is conducted. ... Payment is arranged.
How long does it take to process a health insurance claim?
After the discharge the policyholder can submit all the relevant documents within 7-15 days," says Goyal. Once you submit the claim, the insurer will take few weeks to process your claim. However, on many occasions the process of clarification for queries raised by the claim department can take long.
What is healthcare claim management?
The medical claims management meaning is the organization, billing, filing, updating and processing of medical claims related to patient diagnoses, treatments and medications.
What is a Medical Claim?
A medical claim is a request for payment that your healthcare provider sends to your health insurance company. that lists services rendered. It ensures the doctor gets paid, your insurance pays covered benefits, and you get billed for the remainder. A claim is started the second a patient checks in to an appointment.
How to File a Claim
Healthcare providers will, more often than not, send the claims to be processed themselves. After a service, the doctor’s office will gather your claim, along with all relevant information from any insurance forms you filled out plus the medical codes, and send it to a claims processing department or third-party administrator.
What are the Steps of Claims Processing?
Healthcare claims processing goes through a series of steps to ensure accuracy and approval. A claim’s journey actually begins even before you make an appointment. Because insurance may not always cover all services or procedures, it’s important to look over your health insurance to know what is covered and where to go to get in-network care.
What Happens if a Claim is Denied?
An insurance claim can be denied for several reasons, but just because it was denied does not mean that it can’t be remedied. If you receive a notification that a claim was denied, call the appropriate billing provider to discuss the reasons behind the denial. Here are some common reasons for claims denial.
What Does SDS Offer for Claims Processing?
Claims routing specific to your needs. We can configure routes based on member, provider, location, etc.
What is an HMO?
Health Management Organization (HMO) At one time, HMOs were the most popular MCO option. HMOs operate by providing subscribers with a low premium and a strict network of providers a subscriber can see.
What is CDHP in health insurance?
Consumer-Driven Health Plan (CDHP) A relatively recent development in the world of MCOs, CDHPs enable subscribers to receive PPO-like benefits only after they’ve paid a certain deductible. This deductible is usually quite high, but comes with low premiums and a “savings account” that works like a retirement fund.
What is a copay?
A copay is a relatively small, fixed sum that must be paid before any medical service is rendered. The co-pay does not count against the deductible. A co-insurance is a type of arrangement with the insurance company that divides the responsibility for payment by percentage. Co-insurances are listed with the payer (insurance company)’s portion ...
What is indemnity insurance?
Indemnity is the most basic and straightforward kind of insurance, in that you pay a premium to an insurance company to insulate you from medical expenses. You’ll likely have a deductible and, depending on your insurance plan, a co-pay or co-insurance. Subscribers to indemnity plans have no restrictions on which providers they can see, but indemnity plans are typically much more expensive than managed care options, which we’ll review now.
Why is it so difficult to summarize the billing process?
The process of billing an insurance company or other third-party payer is difficult to summarize because so much of it depends on variables. These variables include things like the patient’s insurance plan, the payer’s guidelines for claim submission, and the provider’s contract with the payer.
What is a UB-04?
These two forms look and operate similarly, but they are not interchangeable. The UB-04 is based on the CMS-1500, but is actually a variation on it—it’s also known as the CMS-1450 form.
What is managed care organization?
Managed care organizations (MCOs) are groups, organizations, or other bodies that seek to reduce the cost of healthcare and increase the efficacy or health services through a number of means.
Why are clearinghouses important?
The service that clearinghouses provide is also beneficial for payers. Clearinghouses format medical claims data according to the unique requirements of each payer. Standardizing the data in this way helps payers streamline their medical billing process.
What is the process of clearinghouses?
Healthcare providers transmit their medical claims to a clearinghouse. Clearinghouses then scrub, standardize, and screen medical claims before sending them to the payer. This process helps mitigate errors in medical coding and reduce the time to receive provider reimbursement.
What is a patient statement?
Patient statement. Patient statement is the final step in the medical billing process. Once the payer has reviewed a medical claim and agreed to pay a certain amount, the payer bills the patient for any remaining costs.
Why are medical claims important?
All-payer claims contain detailed diagnosis and procedure information for any billable patient visit. Healthcare organizations can use this claims information to: Trace referral patterns. Improve population health.
What is medical supplies?
Medical supplies. Medical devices. Pharmaceuticals, and. Medical transportation. When a provider submits a claim, they include all relevant medical codes and the charges for that visit. Insurance providers, or payers, assess the medical codes to determine how they will reimburse a provider for their services.
Where are medical claims transmitted?
In most cases, claims are first transmitted to a clearinghouse. The clearinghouse reviews and reformats medical claims before sending them to the payer. In some cases, healthcare providers send medical claims directly to a payer. High-volume payers like Medicare or Medicaid may receive bills directly from providers.
What causes a claim to be rejected?
Some of the more common causes of claim rejections are: 1 Errors to patient demographic data - age, date of birth, sex, etc. or address. 2 Errors to provider data. 3 Incorrect patient insurance ID. 4 Patient no longer covered by policy - insurance info is not up to date. 5 Incorrect, omitted, or invalid ICD or CPT codes. 6 Treatment code doesn’t match the diagnosis code. 7 Incorrect modifiers. 8 Lack of pre-authorization. 9 Incorrect place of service code. 10 Lack of medical necessity. 11 No referring provider ID or NPI number.
Why is it important to communicate with the billing department?
When processes or employee issues are identified as the root cause of the medical billing errors, it’s important to communicate this to the billers and coders. Likewise asking for their input from the beginning can be a valuable way to identify and improve healthcare claim processing.
What is a superbill?
Superbills that are difficult or impossible to read for the employee (s) responsible for entering the information into the practice management system. If the provider is not readily available to answer questions and clarify, sometime its up to the employee to determine. Getting up-to-date patient info.
What is a denied claim?
A denied claim is one that has been through healthcare claim processing and determined by the insurance company that it cannot be paid. A denied claim can be appealed by submitting the required information or correcting the claim and resubmitting. Causes of Medical Billing Errors.
How accurate is healthcare claim processing?
The American Medical Association has determined that insurers electronic healthcare claim processing accuracy ranges from 88% to 73% depending on the payer.
What is the 80/20 rule?
Many reoccurring health claim processing errors fall into the “80/20” rule which means that 80% of your problems are caused by 20% of the coding.
Why are insurance claims rejected?
Claims are typically rejected for incorrect patient names, date of birth, insurance ID’s, address, etc. Since rejected claims have not been processed yet, there is no appeal - the claim just has to be corrected and resubmitted.
What does it mean to adjudicate a claim?
To adjudicate claims, in short, means to automate how the responsibility of the payer is determined. When a claim reaches them, it will be paid in full, denied, or the price will be negotiated based on the member’s health insurance coverage. You can read more about auto-adjudication here.
Why is automation important in healthcare?
Automation is the key to improving efficiency and accuracy, especially in the healthcare industry. Advancements in OCR (optical character recognition) alleviates the struggle of having to use different templates for different forms.
Why is outsourcing claims management important?
Outsourcing claims management can free up time and space for other tasks within your facility. It can also save you money as well as help you avoid issues like turnover and training. Outsourced teams can also take the pain out of the negotiation processes.
What is EOB in medical billing?
The provider/doctor gets paid. An explanation of benefits (EOB) is sent out to the member. This is not a bill but shows what was or wasn’t covered, and what they can expect on their bill. The member is billed for the remaining balance of what insurance didn’t cover.
How many steps are there in a medical bill?
There are at least a dozen steps that a piece of data must go through to get the bill to the payer accurately. Some processes used currently are still a little outdated such as paper medical records, however, there are ways to ensure accuracy while also improving efficiency during this complex workflow.
What is the difference between a CMS-1500 and a UB-04?
The main difference is that UB-04 forms are used in facilities like hospitals and larger institutions whereas the CMS-1500 forms would come from a smaller facility like private practices.
Why hire a BPO agency?
Hiring a BPO agency to take care of your claims management services can be highly beneficial when it comes to processing medical claims for your members. Smart Data Solutions’ claims management services take care of everything from the health insurance correspondence to provider and member matching and quality control.
The USPTO Guidance
Under the USPTO’s ”Guidance For Determining Subject Matter Eligibility Of Claims Reciting Or Involving Laws of Nature, Natural Phenomena, and Natural Products” issued on March 4, 2014, all claims directed to methods that “recite or involve” a “natural product” are subject to scrutiny under § 101.
Supreme Court Guidance
In Myriad, the Supreme Court made clear that it was not addressing the patent eligibility of method claims:
Method of Treatment Claims
The analysis of Example B, claim 3, of the USPTO Guidance has left examiners believing that only very detailed therapeutic method claims are patent eligible:
Method of Manufacture Claims
The USPTO Guidance does not include any examples of method of manufacture claims, but examiners are subjecting such claims to the multi-factored analysis if the claims recite the use of “natural products.” While such claims should satisfy at least factor (e) (“transformation of a particular article”), because the Guidance instructs examiners to identify elements in addition to the natural product (s) that support eligibility, claims that recite only the manipulation of natural products are being rejected..
Submit Your Comments by July 31
If you agree that the USPTO Guidance goes too far and holds ineligible subject matter that the Supreme Court would not invalidate, please consider submitting written comments by July 31, 2014, by email to [email protected].