Full Answer
Who guidelines on tuberculosis infection prevention and control?
Infection prevention and control consists of evidence-based measures intended to prevent exposure and reduce the risk of transmission of infectious agents. The revised guidelines contain recommendations for specific administrative, environmental controls and respiratory protection, following the assessment made by an external group of experts convened as members of the Guideline Development Group.
Who TB treatment guidelines?
Treatment of tuberculosis: guidelines – 4th ed. WHO/HTM/TB/2009.420 1.Antitubercular agents – administration and dosage. 2.Tuberculosis, Pulmonary – drug therapy. 3.National health programs. 4.Patient compliance. 5.Guidelines. I.World Health Organization. Stop TB Dept. ISBN 978 92 4 154783 3 (NLM classification: WF 360)
Who is most likely to contract tuberculosis?
Tibetan carpet weavers have high TB rates. Globally men are significantly more at risk of contracting and dying from TB than women. In 2017 close to 6 million adult men contracted TB and around 840,000 died from it.
Who is most likely to get tuberculosis?
Who is most at risk? Tuberculosis mostly affects adults in their most productive years. However, all age groups are at risk. Over 95% of cases and deaths are in developing countries. People who are infected with HIV are 18 times more likely to develop active TB (see TB and HIV section below).
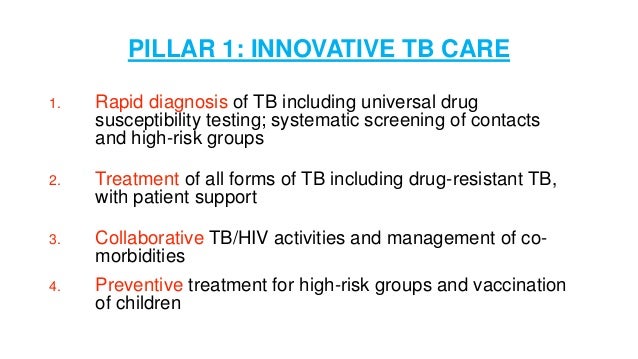
WHO recommended treatment for tuberculosis?
The standardized regimens for anti-TB treatment recommended by WHO include five essential medicines designated as “first line”: isoniazid (H), rifampicin (R), pyrazinamide (Z), ethambutol (E) and streptomycin (S). Table 2.1 shows the recommended doses for adults and children.
What is the first line treatment for TB?
Of the approved drugs, isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA) are considered first-line anti-TB drugs and form the core of standard treatment regimens (Figure 6.4) (Table 6.2).
WHO TB prevention guidelines?
The World Health Organization has updated its guidelines on tuberculosis preventive treatment. Among the 18 recommendations, the group now conditionally recommends shorter regimens as alternative treatment options: 1 month of daily rifapentine and isoniazid, or 4 months of daily rifampicin.
Why is isoniazid and rifampin given together?
Descriptions. Rifampin and isoniazid combination is used to treat tuberculosis (TB) infection. It may be taken alone or with one or more other medicines for TB. Rifampin belongs to the class of medicines called antibiotics and works to kill or prevent the growth of bacteria.
What are the 3 types of tuberculosis?
Tuberculosis: TypesActive TB Disease. Active TB is an illness in which the TB bacteria are rapidly multiplying and invading different organs of the body. ... Miliary TB. Miliary TB is a rare form of active disease that occurs when TB bacteria find their way into the bloodstream. ... Latent TB Infection.
What is the treatment protocol for tuberculosis?
The preferred regimen for treating adults with TB remains a regimen consisting of an intensive phase of 2 months of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB) followed by a continuation phase of 4 months of INH and RIF.
WHO isoniazid preventive therapy guidelines?
The usual preventive therapy regimen is isoniazid (10 mg/kg daily for children, up to a maximum adult dose of 300 mg daily). The recommended duration of isoniazid preventive treatment varies from 6 to 12 months of continuous therapy (9).
What is prophylactic treatment for TB?
Prophylactic TB therapy is effective at preventing the development of active TB disease, according to researchers, but 6- to 9-month courses of daily isoniazid, which are standard in most countries, carry the risk of adverse events, such as liver damage.
How long does it take to treat TB?
TB disease can be treated by taking several drugs for 6 to 9 months. There are 10 drugs currently approved by the U.S. Food and Drug Administration (FDA) for treating TB. Of the approved drugs, the first-line anti-TB agents that form the core of treatment regimens are: isoniazid (INH) rifampin (RIF)
What is it called when TB bacteria multiply?
When TB bacteria become active (multiplying in the body) and the immune system can’t stop the bacteria from growing, this is called TB disease. TB disease will make a person sick. People with TB disease may spread the bacteria to people with whom they spend many hours.
What is XDR TB?
Extensively drug-resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). Treating and curing drug-resistant TB is complicated.
Can TB be treated?
It is very important that people who have TB disease are treated, finish the medicine, and take the drugs exactly as prescribed. If they stop taking the drugs too soon, they can become sick again; if they do not take the drugs correctly, the TB bacteria that are still alive may become resistant to those drugs.
What is the treatment of tuberculosis?
Treatment of tuberculosis is focused on both curing the individual patient and minimizing the transmission of Mycobacterium tuberculosis to other persons; successful treatment of tuberculosis has benefits both for the individual patient and the community in which the patient resides.
What is the decision to initiate combination chemotherapy for tuberculosis?
The decision to initiate combination chemotherapy for tuberculosis is based on clinical, radiographic, laboratory, patient, and public health factors (Figure 1). In addition, clinical judgment and the index of suspicion for tuberculosis are critical in making a decision to initiate treatment.
What is the ATS guideline?
The American Thoracic Society (ATS), Centers for Disease Control and Prevention (CDC), and Infectious Diseases Society of America (IDSA) jointly sponsored the development of this guideline on the treatment of drug-susceptible tuberculosis, which is also endorsed by the European Respiratory Society (ERS) and the US National Tuberculosis Controllers Association (NTCA). This guideline provides recommendations on the clinical and public health management of tuberculosis in children and adults in settings in which mycobacterial cultures, molecular and phenotypic drug susceptibility tests, and radiographic studies, among other diagnostic tools, are available on a routine basis. Nine PICO (population, intervention, comparators, outcomes) questions and associated recommendations, developed based on the evidence that was appraised using GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology [1, 2], are summarized below. A carefully selected panel of experts, screened for conflicts of interest, including specialists in pulmonary medicine, infectious diseases, pharmacokinetics, pediatrics, primary care, public health, and systematic review methodology were assembled and used GRADE methods to assess the certainty in the evidence (also known as the quality of evidence) and strength of the recommendations (see Supplementary Appendix A: Methods and Table 1). This executive summary is a condensed version of the panel's recommendations. Additional detailed discussion of the management of pulmonary and extrapulmonary tuberculosis is available in the full-text version of this guideline.
Is co-trimoxazole used for HIV?
Whereas the WHO recommends routine co-trimoxazole prophylaxis for all HIV-infected people with active tuberculosis disease regardless of the CD4 cell count [66], in high-income countries, co-trimoxazole prophylaxis is primarily used in tuberculosis patients coinfected with HIV with CD4 counts <200 cells/µL [67].