Table 2.
| Variables | Treatment cure | Treatment complete | Loss to follow-up | |
| Female | 30 (28.3%) | 59 (55.7%) | 13 (12.3%) | |
| Type of TB | SPPTB | 59 (78.8%) | 3 (4.1%) | 9 (12.0%) |
| SNPTB | 3 (3.8%) | 59 (75.6%) | 10 (12.8%) | |
| EPTB | 3 (3.8%) | 64 (81.0%) | 7 (8.9%) |
What are the benefits of successful treatment of tuberculosis (TB)?
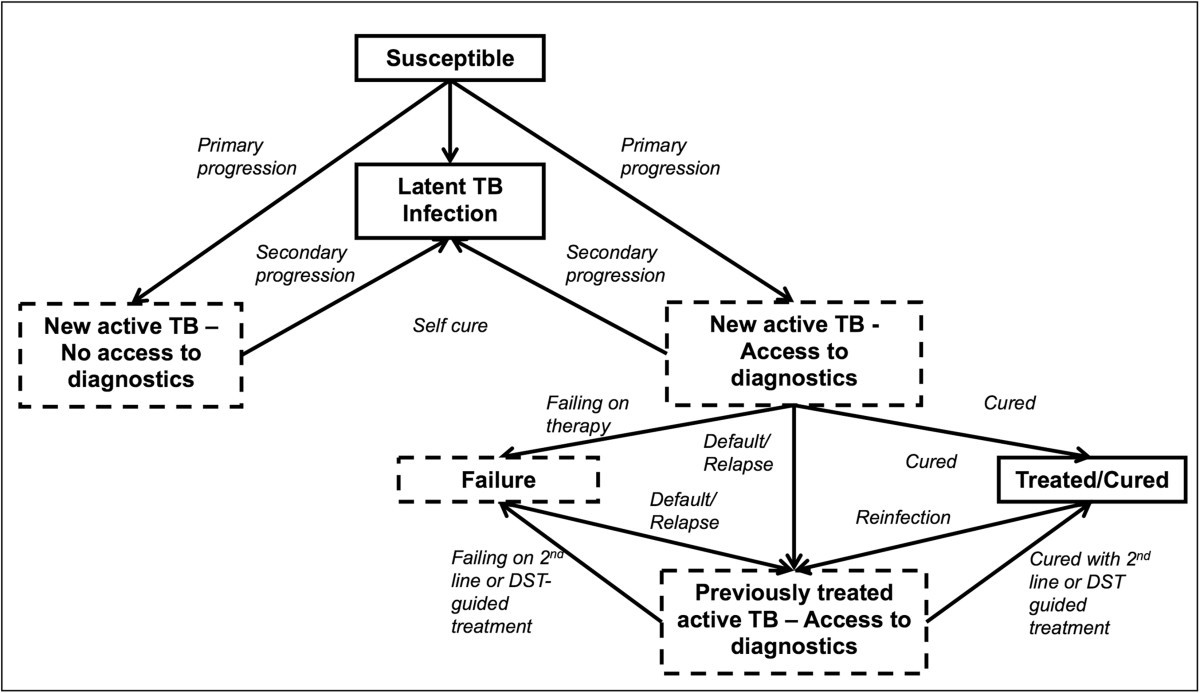
In addition to the obvious benefit to individual patients, successful treatment of infectious cases of TB is essential to prevent the spread of the infection. Detecting and successfully treating a large proportion of TB cases should have an immediate impact on TB prevalence and mortality.
What are the treatment options for TB?
Effective TB treatment for TB disease includes providing multiple anti-TB drugs given over a sufficient period of time to prevent development of drug resistance, minimize the risk of transmission to others, and ultimately, cure the patient of TB disease.
What is the latest guidance on the management of tuberculosis (TB)?
In May to June 2021, WHO convened a GDG to review updated evidence on the management of TB in children and adolescents (aged 0–9 and 10–19 years, respectively). A rapid communication that summarizes the main updates to guidance on the management of TB in children and adolescents was released by WHO in August 2021 (8).
What is the global impact of TB?
Global impact of TB. TB occurs in every part of the world. In 2019, the largest number of new TB cases occurred in the WHO South-East Asian region, with 44% of new cases, followed by the WHO African region, with 25% of new cases and the WHO Western Pacific with 18%. In 2019, 87% of new TB cases occurred in the 30 high TB burden countries.

WHO TB treatment success rate?
The WHO recommends that a good performing tuberculosis program should achieve at least 90% treatment success rate and 85% cure rate [2].
What are treatment outcomes?
5.1 Definition. Treatment outcome research was defined by Mowrer (1953) as a situation whereby the “emphasis is upon measuring significant aspects of personality before and after treatment and noting the nature and extent of the resulting changes” (p. 4).
Have there been any significant breakthroughs in treatment of tuberculosis?
Progress from no therapy to highly efficacious fully oral treatment within 40 years was impressive and for a brief time it seemed that the major obstacles to TB control had been overcome. However, no new first line drug has been developed since rifampicin in 1967.
WHO recommended treatment for tuberculosis?
The standardized regimens for anti-TB treatment recommended by WHO include five essential medicines designated as “first line”: isoniazid (H), rifampicin (R), pyrazinamide (Z), ethambutol (E) and streptomycin (S). Table 2.1 shows the recommended doses for adults and children.
What is a prediction about the outcome of treatment?
Prediction of treatment outcomes is a specific case of the broader and very vibrant field of prediction science. Fundamentally, a prediction is a statement about the way things will be in the future. Good predictions are based on experience and data, but these can be noisy sources of information.
What is a treatment outcome study?
research designed to evaluate the efficacy of interventions and to investigate the mechanism by which effective interventions produce change.
How effective is TB treatment?
TB treatment is effective. Worldwide, nearly 90% of cases of TB and 48% of cases of drug-resistant TB are cured. However, treatment is not quick or easy. The length of treatment and side effects from the drugs used pose huge problems for TB patients and for global efforts to tackle the disease.
How has the treatment for TB changed?
In 2020, CDC and the National Tuberculosis Controllers Association (NTCA) published new guidelines for the treatment of latent TB infection. CDC and NTCA preferentially recommend short-course, rifamycin-based, 3- or 4-month latent TB infection treatment regimens over 6- or 9-month isoniazid monotherapy.
What is the future outlook for tuberculosis?
Almost of TB cases occur in developing countries (95%). The global incidence of TB peaked around 2003 and appears to be declining, with a deceleration of around 2% per year [6]. Ending the TB epidemic by 2030 is among the health targets of the newly adopted Sustainable Development Goals.
Does TB reoccur after treatment?
The relapse rate differs by a country's incidence and control: 0–27% of TB relapses occur within 2 years after treatment completion and most relapses occur within 5 years; however, some relapses occur 15 years after treatment.
What is the duration of TB treatment?
RIPE regimens for treating TB disease have an intensive phase of 2 months, followed by a continuation phase of either 4 or 7 months (total of 6 to 9 months for treatment). This is the preferred regimen for patients with newly diagnosed pulmonary TB.
How do you know if TB treatment is working?
After taking TB medicine for several weeks, a doctor will be able to tell TB patients when they are no longer able to spread TB germs to others. Most people with TB disease will need to take TB medicine for at least 6 months to be cured.
How many people with TB infect other people?
This can lead to delays in seeking care, and results in transmission of the bacteria to others. People with active TB can infect 5–15 other people through close contact over the course of a year. Without proper treatment, 45% of HIV-negative people with TB on average and nearly all HIV-positive people with TB will die.
How many cases of TB are there in 2019?
Alcohol use disorder and tobacco smoking increase the risk of TB disease by a factor of 3.3 and 1.6, respectively. In 2019, 0.72 million new TB cases worldwide were attributable to alcohol use disorder and 0.70 million were attributable to smoking.
What is MDR TB?
Multidrug-resistant tuberculosis (MDR-TB) is a form of TB caused by bacteria that do not respond to isoniazid and rifampicin, the 2 most effective first-line anti-TB drugs. MDR-TB is treatable and curable by using second-line drugs.
How many people have multidrug resistant TB?
Multidrug-resistant TB (MDR-TB) remains a public health crisis and a health security threat. A global total of 206 030 people with multidrug- or rifampicin-resistant TB (MDR/RR-TB) were detected and notified in 2019, a 10% increase from 186 883 in 2018. Globally, TB incidence is falling at about 2% per year and between 2015 and 2019 ...
What are the symptoms of TB in the lung?
Common symptoms of active lung TB are cough with sputum and blood at times, chest pains, weakness, weight loss, fever and night sweats. WHO recommends the use of rapid molecular diagnostic tests as the initial diagnostic test in all persons with signs and symptoms of TB as they have high diagnostic accuracy and will lead to major improvements in the early detection of TB and drug-resistant TB. Rapid tests recommended by WHO are the Xpert MTB/RIF, Xpert Ultra and Truenat assays.
How many lives have been saved from TB?
An estimated 60 million lives were saved through TB diagnosis and treatment between 2000 and 2019. Ending the TB epidemic by 2030 is among the health targets of the United Nations Sustainable Development Goals (SDGs). Tuberculosis (TB) is caused by bacteria (Mycobacterium tuberculosis) that most often affect the lungs.
How many people have TB?
People infected with TB bacteria have a 5–10% lifetime risk of falling ill with TB.
Screening
In March 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 2: Screening – systematic screening for tuberculosis disease (1). These guidelines include 17 new and updated recommendations for the screening of TB disease.
Diagnosis
In July 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 3: Diagnosis – rapid diagnostics for tuberculosis detection 2021 update (3). Three new classes of nucleic acid amplification test (NAAT) are now endorsed by WHO:
Treatment
In April 2021, WHO convened a guideline development group (GDG) to review data from a trial conducted in 13 countries that compared 4-month rifapentine-based regimens with a standard 6-month regimen in people with drug-susceptible TB (6).
Comorbidities, vulnerable populations and people-centred care
In May to June 2021, WHO convened a GDG to review updated evidence on the management of TB in children and adolescents (aged 0–9 and 10–19 years, respectively). A rapid communication that summarizes the main updates to guidance on the management of TB in children and adolescents was released by WHO in August 2021 (8).
Other actions to support TB policy guidance
To exchange views on emerging areas where there is a need for global TB policy guidance, in March 2021, WHO convened a consultation on the translation of TB research into global policy guidelines, attended by scientists, public health experts, partners, civil society and countries (9).
How many people are affected by TB annually?
Drug susceptible TB affects approximately 7 million people annually. It is currently treated with four first line TB medicines for a period of six months.
When did WHO last update its guidance on the treatment of drug susceptible TB?
WHO last updated its guidance on the treatment of drug susceptible TB in 2017. At this time WHO issued a recommendation against the use of shorter fluoroquinolone containing regimens as the evidence did not support that these regimens were more effective than the six-month regimen. However, it is now time to review the evidence on shorter regimens ...
Extract
Tuberculosis (TB) remains an important global health concern, even though it is largely curable with treatment that is affordable and widely accessible for diagnosed and notified TB patients.
Acknowledgements
We would like to acknowledge and thank the two co-chairs of this meeting, Charles Daley and Cathy Hewison, as well as the numerous experts who attended the meeting and who contributed to the discussions.
Footnotes
All authors are staff members of the World Health Organization (WHO). They alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of WHO.
Who Is Most at Risk?
Global Impact of TB
- TB occurs in every part of the world. In 2020, the largest number of new TB cases occurred in the WHO South-East Asian Region, with 43% of new cases, followed by the WHO African Region, with 25% of new cases and the WHO Western Pacific with 18%. In 2020, 86% of new TB cases occurred in the 30 high TB burden countries. Eight countries accounted for ...
Symptoms and Diagnosis
- Common symptoms of active lung TB are cough with sputum and blood at times, chest pains, weakness, weight loss, fever and night sweats. WHO recommends the use of rapid molecular diagnostic tests as the initial diagnostic test in all persons with signs and symptoms of TB as they have high diagnostic accuracy and will lead to major improvements in the early detection of TB …
Treatment
- TB is a treatable and curable disease. Active, drug-susceptible TB disease is treated with a standard 6-month course of 4 antimicrobial drugs that are provided with information and support to the patient by a health worker or trained volunteer. Without such support, treatment adherence is more difficult. Since 2000, an estimated 66 million lives were saved through TB diagnosis an…
TB and HIV
- People living with HIV are 18 (Uncertainty interval: 15-21) times more likely to develop active TB disease than people without HIV. HIV and TB form a lethal combination, each speeding the other's progress. In 2020, about 215 000 people died of HIV-associated TB. The percentage of notified TB patients who had a documented HIV test result in 2020 was only 73%, up from 70% in 2019. In th…
Multidrug-Resistant TB
- Anti-TB medicines have been used for decades and strains that are resistant to one or more of the medicines have been documented in every country surveyed. Drug resistance emerges when anti-TB medicines are used inappropriately, through incorrect prescription by health care providers, poor quality drugs, and patients stopping treatment prematurely. Multidrug-resistant tuberculosi…
Catastrophic Cost
- WHO’s End TB Strategy target of “No TB patients and their households facing catastrophic costs as a result of TB disease”, monitored by countries and WHO since WHA67.1 End TB Strategy was adopted in 2015, shows that the world did not reach the milestone of 0% by 2020. According to the results of 23 national surveys on costs faced by TB patients and their families, the percentag…
Investments in TB Prevention, Diagnosis and Treatment and Research
- US$ 13 billion are needed annually for TB prevention, diagnosis, treatment and care to achieve global targets agreed on UN high level-TB meeting. 1. Investments in TB prevention, diagnosis and care for tuberculosis in low- and middle-income countries (LMICs) accounting for 98% of reported TB cases, fall far short of what is needed. Less than half (41%) of the global TB funding target is …
Global Commitments and The Who Response
- On 26 September 2018, the United Nations (UN) held its first- ever high-level meeting on TB, elevating discussion about the status of the TB epidemic and how to end it to the level of heads of state and government. It followed the first global ministerial conference on TB hosted by WHO and the Russian government in November 2017. The outcome was a political declaration agree…
Screening
- In March 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 2: Screening – systematic screening for tuberculosis disease (1). These guidelines include 17 new and updated recommendations for the screening of TB disease. Populations identified as priorities for TB screening include contacts of TB patients, people living with HIV, people expose…
Diagnosis
- In July 2021, WHO released the WHO consolidated guidelines on tuberculosis. Module 3: Diagnosis – rapid diagnostics for tuberculosis detection 2021 update (3).Three new classes of nucleic acid amplification test (NAAT) are now endorsed by WHO: 1. moderate complexity automated NAATs, which are recommended for the initial detection of TB and resistance to rifa…
Treatment
- In April 2021, WHO convened a guideline development group (GDG) to review data from a trial conducted in 13 countries that compared 4-month rifapentine-based regimens with a standard 6-month regimen in people with drug-susceptible TB (6). The GDG considereda 4-month regimen composed of rifapentine, isoniazid, pyrazinamide and moxifloxacin that met ...
Comorbidities, Vulnerable Populations and People-Centred Care
- In May to June 2021, WHO convened a GDG to review updated evidence on the management of TB in children and adolescents (aged 0–9 and 10–19 years, respectively). A rapid communication thatsummarizes the main updates to guidance on the management of TB in children and adolescents was released by WHO in August 2021 (8). The communication includes new inform…
Other Actions to Support TB Policy Guidance
- To exchange views on emerging areas where there is a need for global TB policy guidance, in March 2021, WHO convened a consultation on the translation of TB research into global policy guidelines, attended by scientists, public health experts, partners,civil society and countries (9). In June 2021, WHO launched a TB Knowledge Sharing Platform to bring all WHO TB guidelines, op…