
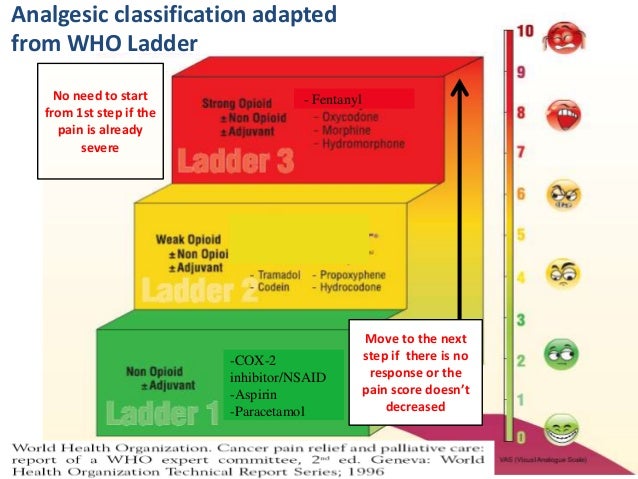
In 1986, the World Health Organization (WHO) established the first recommendations to trigger the treatment of cancer pain. These recommendations, which were insufficient, were based on the WHO “pain ladder,” a stepwise approach to the use of analgesics depending on pain severity. The regimen considered in a parallel manner the severity of pain and the presumed efficacy of analgesics. The WHO stratified three steps in this approach of analgesic drugs: Step I using non-opioid analgesics (acetaminophen or non-steroidal anti-inflammatory drugs—NSAIDs), Step II with weak”“ opioids (hydrocodone, codeine, or tramadol), and Step III with strong”“ opioids (morphine, hydromorphone, oxycodone, fentanyl, or methadone). Additional drugs (adjuvants) were to be used to decrease anxiety.
Full Answer
Should the who analgesic ladder be stepwise?
However, with concerns growing regarding opioid use, a shift in the stepwise approach of the WHO analgesic ladder in an age of developing technology and surgical offerings could have profound implications for patients and public health. Surgical interventions potentially provide a long-term, cost-effective management strategy to reduce opioid use.
What are the three principles of the analgesic ladder?
World Health Organization (WHO) Analgesic Ladder The three main principles of the WHO analgesic ladder are: “By the clock, by the mouth, by the ladder”. By the clock: To maintain freedom from pain, drugs should be given “by the clock” or “around the clock” rather than only “on demand” (i.e. PRN).
What is the first step in the pain ladder?
The original ladder mainly consisted of three steps[4]: First step. Mild pain: non-opioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen with or without adjuvants Second step. Moderate pain: weak opioids (hydrocodone, codeine, tramadol) with or without non-opioid analgesics, and with or without adjuvants
Does the World Health Organization’s 3-step analgesic ladder work for cancer pain management?
The opioid epidemic challenges current attitudes toward pain management and necessitates the reexamination of the World Health Organization (WHO) 3-step analgesic ladder, introduced in 1986 for cancer pain management.

WHO analgesic ladder explained?
The 1986 version of the WHO analgesic ladder proposes that treatment of pain should begin with a nonopioid medication (Figure 1). If the pain is not properly controlled, one should then introduce a weak opioid. If the use of this medication is insufficient to treat the pain, one can begin a more powerful opioid.
What is the WHO ladder?
The WHO analgesic ladder specifies treatment on pain intensity, from simple analgesics for mild pain to opioid analgesics for moderate and severe pain.
Who analgesia steps?
Its three steps are: Step 1 Non-opioid plus optional adjuvant analgesics for mild pain; Step 2 Weak opioid plus non-opioid and adjuvant analgesics for mild to moderate pain; Step 3 Strong opioid plus non-opioid and adjuvant analgesics for moderate to severe pain.
Which treatment would be found on the first rung of the WHO analgesic ladder?
The WHO pain ladder (Figure 1) describes pain in terms of intensity and recommends that analgesics be prescribed starting at Step 1 (nonopioid analgesics, such as acetaminophen or non-steroidal anti-inflammatory drugs [NSAIDs]).
How many steps are in the World Health Organization ladder?
The original ladder mainly consisted of three steps[4]: First step. Mild pain: non-opioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen with or without adjuvants.
What are the 3 types of analgesics?
There are three broad categories of analgesic medications: (1) nonopioid analgesics, which includes the nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, dipyrone, and others; (2) a diverse group of drugs known as the "adjuvant analgesics," which are defined as "drugs that have primary indications other ...
What are the pain pathways?
Thus there are two major ascending pathways for pain: a direct lateral spinothalamic pathway and an indirect medial spinoreticulothalamic pathway.
Which drug is analgesic?
Analgesics are a class of medications designed specifically to relieve pain. They include acetaminophen (Tylenol), which is available over the counter (OTC) or by prescription when combined with another drug, and opioids (narcotics), which are only available by prescription.
What is pain according to who?
The World Health Organisation defines pain as “an unpleasant sensory or emotional experience associated with actual or potential tissue damage, or described in terms of such damage”.
Which of the following would be an example of the progression of medication in ascending order according the World Health Organization WHO analgesic ladder?
By the ladder: If pain occurs there should be prompt administration of drugs in the following order: • non-opiods (e. g. acetaminophen) • as necessary, mild opiods (e. g. codeine) • then strong opiods (e. g. morphine or hydromorphone) until the patient is free of pain.
What is an example of adjuvant analgesic?
Commonly used drugs in this class include: baclofen (Lioresal), carisoprodol (Soma), cyclobenzaprine (Flexeril), diazepam (Valium), methocarbamol (Robaxin), orphenadine (Norflex), metaxalone (Skelaxin), and tizanidine (Zanaflex).
What is the preferred treatment plan for chronic pain?
1. Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient.
What is the WHO analgesic ladder?
The WHO analgesic ladder was a strategy proposed by the World Health Organization (WHO), in 1986, to provide adequate pain relief for cancer patients. [1] . The analgesic ladder was part of a vast health program termed the WHO Cancer Pain and Palliative Care Program aimed at improving strategies for cancer pain management ...
Why was the analgesic ladder designed?
[14] The lack of proper knowledge of drugs, underdosing and wrong timing of drugs, fear of addiction in patients, and lack of public awareness are severe limitations that limit the proper implementation of the strategy. [15]
What is the first step in pain management?
First step. Mild pain: non-opioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen with or without adjuvants. Second step. Moderate pain: weak opioids (hydrocodone, codeine, tramadol) with or without non-opioid analgesics, and with or without adjuvants. Third step.
What is the third step of opioids?
Third step. Severe and persistent pain: potent opioids (morphine, methadone, fentanyl, oxycodone, buprenorphine, tapentadol, hydromorphone, oxymorphone) with or without non-opioid analgesics, and with or without adjuvants. The term adjuvant refers to a vast set of drugs belonging to different classes.
What is the strongest analgesic?
For acute pain, the strongest analgesic (for that intensity of pain) is the initial therapy and later toned down, whereas, for chronic pain, employing a step-wise approach from bottom to top. However, clinicians should also provide de-escalation in the case of chronic pain resolution.
What are the non-pharmacological approaches to trolleys?
Consequently, a wide range of non-pharmacological approaches such as yoga, acupuncture, psychotherapy, and occupational therapy, are present in specific 'drawers' of the trolley and can be used according to the clinical needs and skills of the operator, as well as available resources.
What is the IASP?
For instance, the International Association For The Study Of Pain (IASP) suggested adopting a therapeutic approach more focused on the type of pain (i.e., mechanism) and on the mechanism of action of the drugs used to treat it.
What is the WHO 3-step analgesic ladder?
The opioid epidemic challenges current attitudes toward pain management and necessitates the reexamination of the World Health Organization (WHO) 3-step analgesic ladder, introduced in 1986 for cancer pain management. Surgical treatment of pain is a logical extension of the original guideline, which is often absent in conversations with patients about treatment options for their pain and consequentially underutilized. However, with concerns growing regarding opioid use, a shift in the stepwise approach of the WHO analgesic ladder in an age of developing technology and surgical offerings could have profound implications for patients and public health. Surgical interventions potentially provide a long-term, cost-effective management strategy to reduce opioid use. This review canvasses surgical options, highlights literature on failed back surgery syndrome and spinal cord stimulation and reconsiders the current ladder approach to pain management.
What is the 3 step ladder?
Presented in 1986, the World Health Organization (WHO) analgesic ladder provided a framework for the stepwise medical management of cancer-related pain. 1 This 3-step ladder begins with nonopioid analgesics with or without nonpharmacological approaches for mild pain, continues with weak opioid medications (eg, codeine) with or without nonopioid analgesics and adjuvants for mild-to-moderate pain, and progresses to strong opioids (eg, oxycodone) with or without nonopioid analgesics and adjuvants for moderate-to-severe pain. 1 The American Pain Society’s identification of pain as the “fifth vital sign” in 1995 portended the increased importance of not only adequate treatment of pain in patients but also education of health care professionals. 2, 3 Eventually, a modified version of the 3-step ladder placed interventional pain management as a fourth step. 4, 5 Development of this algorithmic approach aimed to control refractory or intractable pain in both an efficient and a safe manner, providing a rational and balanced method to maximize pain relief while minimizing side effects and risks.
Is neuromodulation reversible?
Each modality has advantages and disadvantages. Neuromodulation, both chemical and electrical, tends to be reversible, adjustable, testable, and nondestructive. It also provides patients with real or perceived ability to control the treatment using dedicated remote controllers.
Is surgical treatment of pain a logical extension of the original guideline?
Surgical treatment of pain is a logical extension of the original guideline, which is often absent in conversations with patients about treatment options for their pain and consequentially underutilized.
Is surgery a final step in pain management?
Despite advances, surgical treatments remain a final step in pain management, typically after all other approaches fail. 37 With concerns growing regarding complications of opioid use in an age of developing technology and surgical offerings, a paradigm shift in pain management away from the WHO analgesic ladder toward earlier surgical intervention could have profound implications for patients and public health. Over time, surgical procedures have become more precise, less invasive, and better understood and recognized by both patients and their physicians. The ethical dilemma of beneficence vs nonmaleficence is not limited to weighing the advantages and risks of surgery alone. The risks of surgery avoidance should also be considered, given that medical (“conservative”) treatments can cause tolerance, dependence, or clinical side effects, as seen with most analgesic regimens, opioid or otherwise. The possibility of long-term pain relief and associated increase in functionality and improvement in quality of life justifies surgery as an earlier treatment option, perhaps before opioids are introduced.
Why add a fourth step to the pain ladder?
Retaining the use of pain intensity as the differentiator between steps, a fourth step could be added to the original pain ladder to accommodate very severe pain, such as occurs in the palliative setting in certain patients with advanced, particularly egregious forms of cancer. Pain specialists treat “very severe” noncancer pain as well. Severe to very severe pain may not respond to conventional pharmacologic treatment and may require intervention. This proposed change reflects modern clinical practice and our growing understanding of pain syndromes (Figure 3).
What are the steps of the Pain Ladder?
Its simple, progressive steps of 1) anti-inflammatory agents, 2) weak opioids, and 3) strong opioids is still fundamentally sound. In this article, Pergolizzi and Raffa present a thoughtful and detailed set of recommendations to modify the 3-step process. No doubt all of us have some thoughts about modifying the “WHO Pain Ladder,” based on the many new physical, interventional, and pharmacologic measures that have come forward since 1986. My message is that too many purveyors of potent opioid pharmaceuticals and invasive interventions have promoted and championed the use of these therapies, which have well-known complications, without first attempting regimens that are less onerous. Practical Pain Management desires that all pain practitioners make 2014 a year in which they develop and practice a “WHO Pain Ladder” protocol that is modified with some new measures to give our patients their best chance at a wide range of safe alternatives before resorting to potent opioids and invasive interventions.
What is the first step in pain management?
Step 1: Nonopioid Analgesics. Nonopioid analgesics include acetylsalicylic acid, acetaminophen, and selective and non-selective NSAIDs. The original WHO pain ladder states that adjuvant agents may be included with these nonopioid agents, but it does not name those agents.
What are the auxiliary agents in Step 3?
The original Step 3 also mentioned, but did not specify, adjuvant agents. Such auxiliary agents are no longer acetaminophen or NSAIDs, but rather calcitonin, cortisone, anticonvulsants, antidepressants, selective serotonin reuptake inhibitors, and other agents recognized in the treatment of pain.
What is step 3 in cancer treatment?
Thus, when clinically appropriate and available, Step 3 may include “loose dose” combination therapy with a variety of other agents. Revising the third step to name some adjuvant medications may help clinicians be mindful of multimodal therapies that can be particularly beneficial in cancer pain.
What is the best treatment for neuropathic pain?
Pain with a neuropathic component may be effectively treated with anticonvulsants, such as pregabalin (Lyrica) and gabapentin. 14 More information on the identity and potential uses of such adjuvant agents should be included in Step 1 of an updated pain ladder.
What is leapfrogging over the middle step?
Another deviation allowed for leapfrogging over the middle step in the case of severe pain or breakthrough cancer pain, defined as a sudden, intense, short period of severe pain occurring against an ambient background of lower-level pain.
What is the ladder approach to cancer?
The ‘ladder’ approach encouraged use of adjunctive medicines at each rung of the ladder and use of strong opioids only at the top of the ladder. The analgesic ladder was validated as a tool for improving the treatment of cancer pain. Unlike acute pain and cancer pain at the end of life, persistent pain not associated with cancer has an ...
What is a stepwise approach to pain?
A stepped approach to pain prescribing. In 1986 the World Health Organization proposed a step-wise approach to use of medication in cancer related pain. The underlying principle was that medications should be used in an incremental fashion according to the patient’s reported pain intensity ie, for mild pain non-opioid medication should be ...
Introduction
- Presented in 1986, the World Health Organization (WHO) analgesic ladder provided a framework for the stepwise medical management of cancer-related pain.1 This 3-step ladder begins with nonopioid analgesics with or without nonpharmacological approaches for mild pain, continues with weak opioid medications (eg, codeine) with or without nonopioid anal...
Practical Considerations in Surgical Management of Pain
- Surgery for pain differs from many conventional operations, neurosurgical and others, aimed at elimination of the source of pain—such as, for example, appendectomy, spinal decompression, carpal tunnel release, or joint replacement. Instead, it is aimed at the pain-processing (nociceptive) system and includes destructive procedures (open or percutaneous ablations and …
Impact of Surgical Management of Pain
- Given the scope of the opioid crisis, the potential impact of surgical intervention for pain is far-reaching, extending from patient-level to systems-level outcomes. Of the pain interventions available, perhaps the most studied to date is spinal cord stimulation (SCS), particularly in patients with chronic low-back pain or failed back surgery syndrome (FBSS). The long-term succ…
Ethical Considerations and Paradigm Shift
- Despite advances, surgical treatments remain a final step in pain management, typically after all other approaches fail.37 With concerns growing regarding complications of opioid use in an age of developing technology and surgical offerings, a paradigm shift in pain management away from the WHO analgesic ladder toward earlier surgical intervention could have profound implications …