
Is PRP approved by the FDA?
*Research for the different applications of PRP is promising and rapidly growing. Although the equipment used to produce PRP and the injections themselves have been cleared by the FDA, this procedure is considered investigational and has not been officially approved by the FDA for most uses.
What is the theoretical basis for the use of PRP?
The efficacy of certain growth factors in healing various injuries and the concentrations of these growth factors found within PRP are the theoretical basis for the use of PRP in tissue repair.
What can PRP treatments treat?
PRP treatments can enhance hair restoration and other cosmetic plastic surgery procedures. The platelets, one type of blood cells, contain growth factors that can trigger cell proliferation, speed healing and stimulate tissue regeneration in the treated area. PRP treatment has been used to support wound healing in trauma and joint injury.
Is there any peer reviewed literature on platelet rich plasma (PRP)?
There is presently no information in peer reviewed literature. ^ Knoepfler, Paul (2020-05-19). "Dr. Drew Lansdown Platelet Rich Plasma (PRP) Interview". The Niche. Retrieved 2021-02-07.
When was PRP found?
People's Redemption PartyChairpersonAlhaji Falalu BelloFounded1978HeadquartersAbujaIdeologySocial democracy Social liberalism Democratic humanism6 more rows
Is PRP medically proven?
Although the equipment used to produce PRP and the injections themselves have been cleared by the FDA, this procedure is considered investigational and has not been officially approved by the FDA for most uses. Since PRP is a substance derived from one's own blood, it is not considered a drug.
How old is PRP treatment?
However, PRP therapy has been in use since the 1980s. It's been used for problems such as healing injured tendons, ligaments, and muscles.
Has PRP been approved by the FDA?
PRP is not FDA-approved but it can be legally offered 'off-label' for musculoskeletal conditions including muscle strains and soft tissue injuries. Texas Orthopedics physicians may recommend PRP injections for certain injuries, arthritis, or after surgery to aid in your recovery.
Can PRP regrow hairline?
PRP therapy can help your hair grow back by stimulating the weakened hair follicles that are causing your hairline to recede. Platelet-rich plasma from your body will trigger tissue and cell repair in the region. The PRP also produces collagen and elastin for the skin in the area.
Is PRP FDA approved for hair?
PRP therapy is cleared by the FDA for use in orthopedics, but it's considered off-label for skin and hair procedures, says Dr. Amelia K. Hausauer, a California-based dermatologist who's published research on PRP therapy for hair loss. The devices that separate cells from plasma are FDA-approved, notes Dr.
Can a 17 year old get PRP?
Prp can be done for both females and males and at any age after 18 years . Ofcourse sooner it's started better is the outcome . Maintenance sessions are required and interval may vary from patient to patient as hair loss issue is a continuing process and thus patient may need multiple touch up sessions . Dr.
Is PRP good for face?
PRP stimulates collagen and elastin production which thickens and tightens thinning skin, effectively smoothing wrinkles and fine lines. Because it boosts collagen, it's also a great treatment for improving overall skin texture and tone. It's particularly good for people who suffer from rosacea or acne.
Is PRP safe for face?
PRP injections are safe and may be modestly beneficial for aging skin. The evidence is most convincing for improvement of facial skin texture. The persistence of these effects is not known. More high-quality trials with sufficient follow-up are needed to optimize treatment regimens.
Is PRP approved in Europe?
Since PRP is a blood-derived product, its use is strictly regulated in Europe, to ensure the control of all the aspects related to preparations, storage, and distribution, and therefore the quality and safety of PRP products.
Is PRP treatment safe?
PRP injections are considered safe when performed by a trained medical provider. Mild risks include pain, redness, headaches, and temporary hair shedding. PRP may not be appropriate for those with a history of bleeding disorders or autoimmune disease.
Why is PRP so painful?
Platelets release many chemicals that summon or call other reparative cells to the area of injury. When the platelets release their chemicals, it causes an inflammatory response. This inflammation is also why PRP injections into the tendons, muscles, and ligaments will hurt.
When was PRP first used?
The concept of PRP began in the 1970s in the field of hematology, which is the study of blood. This term was coined so that hematologists could define blood that had a higher platelet count than normal blood. This platelet-rich blood was mainly used for blood transfusions for individuals who suffered from low platelet count in their blood.
What is PRP used for?
Since then, PRP began to be used in orthopedics to help with bone grafts and fractures, connective tissue repair, cardiac surgery, sports injuries, plastic surgery, gynecology, urology, and more.
How does PRP work?
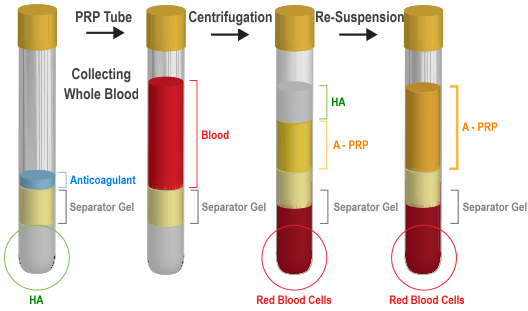
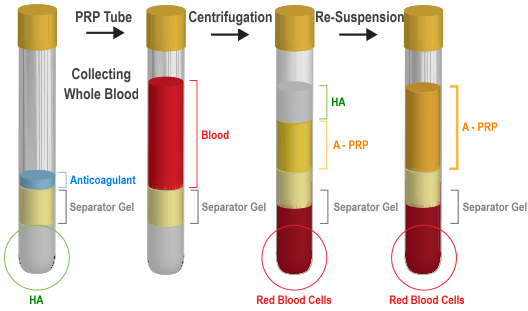
Like we mentioned above, PRP is derived from your own blood. A vial of blood is drawn, and then it is centrifuged to separate the different components. This isolates the red blood cells, platelet-rich plasma, and platelet-poor plasma. The plasma rich in platelets is then removed from the vial to be used for PRP therapy.
Why is PRP important?
These platelets are important in the body because they are able to improve and speed up the healing processes in the body. This is possible because of the many proteins, immune system cells, and other bioactive factors that PRP is composed of.
Why do people need PRP injections?
PRP injections have been shown to improve the healing process, reducing the risk of developing an infection. Excess bleeding can also sometimes occur during cardiac surgery. Because of this, blood transfusions are needed during surgery by some of the patients.
What is the history of platelet rich plasma?
What is the History of Platelet-Rich Plasma - SRMC. Platelet-rich plasma, also known as PRP, contains a high concentration of growth factors and platelets. PRP that is used in regenerative medicine is autologous, meaning that it is generated from a person’s own body. About six percent of normal blood is made up of platelets.
What are the advantages of PRP?
One of the biggest advantages of PRP is that it is able to be delivered directly into the injury site. It is also easy to obtain, comes at a low price point, and comes with very few potential negative side effects. Because of these advantages, PRP can be used for many different medical treatments.
Platelet Rich Plasma referred to as Autologous
Platelet Rich Plasma (PRP) sometimes referred to as Autologous (using patient’s own blood) is exactly that, a component harvested from someone’s blood whereby a high number of platelets are concentrated. Blood is made up of red blood cells, white blood cells, plasma and platelets.
Platelet Rich Plasma – PRP – History
Platelets are responsible for the process of hemostasis, development of new connective tissue, and restoration of blood circulation. A blood specimen typically contains 93% RBC, 6% Platelets, and 1% WBC.
How is PRP prepared?
PRP is prepared by taking blood from the person, and then putting it through two stages of centrifugation designed to separate PRP from platelet-poor plasma and red blood cells. This is usually done by the clinic offering the treatment, using commercially available kits and equipment.
What is PRP used for?
Besides the use in clinical practice PRP has been utilized for various tissue engineering applications in the context of bone, cartilage, skin, and soft tissue repair. It has been reviewed to serve as a source for the "delivery of growth factors and/or cells within tissue-engineered constructs, often in combination with biomaterials".
What is PRP plasma?
Platelet-rich plasma. Platelet-rich plasma ( PRP ), also known as autologous conditioned plasma, is a concentrate of platelet -rich plasma protein derived from whole blood, centrifuged to remove red blood cells. Though promoted to treat an array of medical problems, evidence for benefit is mixed as of 2020, with some evidence for use in certain ...
What is the classification of PRP?
There are four general categories of preparation of PRP based on its leukocyte and fibrin content: leukocyte-rich PRP (L-PRP), leukocyte reduced PRP (P-PRP; leukocyte reduced or pure PRP), leukocyte platelet-rich fibrin and pure platelet-rich fibrin.
How much does PRP cost?
The cost of a PRP treatment in the U.S. has been quoted as $1000 out-of-pocket expenses, as it is usually not covered by health insurance. PRP has received attention in the popular media as a result of its use by athletes. Use in an office setting is not approved by the FDA.
What are the growth factors in PRP?
The growth factors and other cytokines present in PRP include: platelet-derived growth factor. transforming growth factor beta. fibroblast growth factor.
Is PRP good for musculoskeletal pain?
A 2014 Cochrane review of PRP in musculoskeletal injuries found very weak evidence for a decrease in pain in the short term, and no difference in function in the short, medium or long term. There was weak evidence that suggested that harm occurred at comparable, low rates in treated and untreated people. Similarly, another 2017 review for treating pain on skin graft donor sites found the evidence for benefit was poor.
When was platelet therapy discovered?
In the 1970s, when a lot of medical discovery was happening, was also the time when platelet-rich plasma therapy was discovered and applied in regenerative medicine (4).
When was platelet rich plasma first used?
In the 1970s , hematologists first started the concept of platelet-rich plasma. They created the term to describe plasma with platelet count that surpassed the number of that from peripheral blood, which was used for patients with thrombocytopenia or low platelet count. (5)
Why is plasma used?
Plasma is amazing because it is used in a lot of ways. Fresh frozen plasma helps in the treatment of people who have massive bleeding that results in shock— like seen in burns or those with trauma. It can also help in clotting especially in those suffering from massive internal bleeding or for people with clotting abnormalities.
Why are platelets important?
In simple words, they are important in maintaining balance to our body when problems arise. They also store antibacterial and even fungicidal proteins which help in activating other processes in the body that deals with inflammation. This is where the healing property of platelets lies — they help deal with the pain because they help with the inflammation and they facilitate the recovery of the body through the growth factors that are associated with healing.
How is plasma extracted?
Plasma can be extracted and separated by centrifugation which we will tackle later on. 55% of our blood is plasma and it is formed from the water and salt that has been absorbed by our stomach and intestines. The bone marrow, dead blood cells, and the other tissues of the body also help in the formation of plasma.
What are the proteins in a plasma?
It also has proteins like albumin and globulin that help maintain the balance in the blood. Sodium, potassium, bicarbonate, chloride, and calcium are also present in the plasma to help maintain the normal value of blood pH. Lastly, it also contains immunoglobulins that protect our body from both viral and bacterial infections.
Is platelet rich plasma safe?
Platelet-rich plasma is just as the name suggests— millions of platelets in the plasma, extracted from the patient himself or through commercially-prepared PRPs, thus making it 100% safe from any allergic reaction or infection, given to areas in the body with injuries or problems.
What is PRP therapy?
PRP Therapy, Hair Loss and Hair Transplants. PRP therapy is becoming a popular complement to hair transplants. PRP can help accelerate the growth of transplanted hair roots while also thickening existing hair.
How does a doctor inject PRP?
First, the doctor draws blood from the patient’s arm and then separates the PRP from the rest of the blood’s components. After injecting lidocaine to numb the treatment area, the doctor carefully injects the PRP into multiple places under the skin.
What is a PRP injection?
Platelet-rich plasma (PRP) injections are gaining popularity for a variety of conditions, from sports injuries to hair loss. The treatment uses a patient’s own blood cells to accelerate healing in a specific area.
What is the purpose of platelet injections at Johns Hopkins?
Our team of experts at the Johns Hopkins Musculoskeletal Center offers platelet-rich plasma injections to help alleviate pain, improve mobility and decrease inflammation.
How to make platelet rich plasma?
To create platelet-rich plasma, clinicians take a blood sample from the patient and place it into a device called a centrifuge that rapidly spins the sample, separating out the other components of the blood from the platelets and concentrating them within the plasma.
How long does it take for PRP to work?
The results of PRP treatment are most noticeable after several weeks for joint injections and six months for scalp injections, and are not permanent; patients may require additional injections at the direction of their doctor.
What to do if you are considering PRP injections?
If you are considering PRP injections, be sure to talk with your health care provider about all the benefits and risks.
What is PRP treatment?
Because the mechanisms of tendinopathy are not completely understood, the current treatment options for this tendon disease remain largely palliative. PRP is a popular cell-free therapy that is used worldwide to treat tendinopathy. Basic science studies have consistently shown the beneficial effects of PRP on tendons including increased tendon cell proliferation, increased expression of anabolic genes and proteins, and reduced tendon inflammation. However, the efficacy of PRP in clinical trials is not consistent leading to the controversies regarding the PRP treatment efficacy. Among clinical studies, RCTs are considered to be the gold standard in assessing the efficacy of PRP treatments in clinical settings. However, when an RCT study yields negative results on PRP treatment of tendinopathy, the reasons for the negative results should be carefully analyzed. A number of factors could cause the negative results in RCTs. The most common is the relatively small sample size. Considering the fact that the extremely variable responses of humans to any treatment are unavoidable, the use of a small number of subjects in an RCT study will surely reduce the statistical power to detect the treatment effects by PRP. Another major factor in RCTs is the undefined PRP composition in the preparations used in RCT studies. Most clinical studies use PRP, prepared from a commercial kit, and a predetermined dose is administered for all types of tendon injuries and all patients irrespective of age, gender, disease history, and so forth. Basic science studies on the other hand indicate that stem cells could be used to promote tendon wound healing only in early stages but not so effectively in later stages that may be dominated by the presence of degenerative tissues. Therefore, the so-called “one-size-fits-all” approach may be the main reason for the conflicting results observed in the PRP treatment of tendinopathy in clinical studies. Instead of this, we propose the use of an individualized approach based on the conditions of individual patients. Such efforts may improve the efficacy of PRP for the treatment of tendon injuries and may effectively address the controversies on the PRP treatment efficacy in clinical trials.
Why is PRP used in medicine?
PRP is safe because it is an autologous product derived from a patients' own blood and contains platelets and bioactive factors that can modify the biological microenvironment at injury sites, thus enhancing tissue healing. More importantly, PRP is not known to have any adverse effects unlike the commonly used nonsteroid anti-inflammatory drugs (NSAIDs) that are known to affect the gastrointestinal, cardiovascular, and renal systems [19, 20]. PRP is easy to use because of the simple preparation protocols; in fact, a number of PRP preparation kits are commercially available that are widely used in orthopaedic clinics. Besides, the application of PRP in the form of injections is also noninvasive and allows easy administration in clinical settings.
What is PRP used for?
Platelet-Rich Plasma (PRP) has been widely used in orthopaedic surgery and sport medicine to treat tendon injuries. However, the efficacy of PRP treatment for tendinopathy is controversial. This paper focuses on reviewing the basic science studies on PRP performed under well-controlled conditions. Bothin vitro andin vivo studies describe PRP's anabolic and anti-inflammatory effects on tendons. While some clinical trials support these findings, others refute them. In this review, we discuss the effectiveness of PRP to treat tendon injuries with evidence presented in basic science studies and the potential reasons for the controversial results in clinical trials. Finally, we comment on the approaches that may be required to improve the efficacy of PRP treatment for tendinopathy.
Does PRP increase inflammation?
However, leukocytes in PRP could potentially increase inflammation because they significantly increased the gene and protein expression of IL-1β, IL-6, and TNF-αin tendon cells [39]. This demonstrates that leukocytes can exacerbate inflammation in tendon cells but P-PRP without leukocytes can be anti-inflammatory because it decreased the gene expression of IL-6 when compared to untreated controls [39]. Similarly, PRP also reduced the gene expression and production of IL-6 in tendon cells when compared to cells treated with IL-1β[50]. It should be noted that IL-6 levels in tendon cells cultured in 2D and 3D hydrogels were increased by P-PRP [56]; therefore, future study may be still needed to determine the precise effects of P-PRP on IL-6. McCarrel et al. [45, 57] also showed that high concentration of leukocytes in PRP could induce higher expression of IL-1βand TNF-αwhen compared to P-PRP. Because platelets recruit leukocytes and progenitor cells to the sites of vascular injury and inflammation, they induce changes in cell permeability and promote chemotaxis and cell proliferation, which are essential steps in tissue repair. Macrophage, a kind of leukocyte, was reported to be involved in the maintenance of inflammatory state or innate immune response. It also induced tenocytes to synthesize relevant amounts of MCP-1/CCL2 and RANTES/CCL5, which could mediate migration of more monocytes/macrophages that can trigger inflammatory and angiogenic mechanisms [56, 58]. L-PRP can be directly involved in the inflammatory response by producing and releasing inflammatory mediators such as the cytokines, IL-1βand CD40L, and chemokines, CXCL1 and CCL2. Besides, PRP induces the expression of chemokine receptors, particularly CCR1, CCR3, CCR4, and CXCR4, thus regulating the inflammatory response associated with the healing process [55].
Does PRP affect tenocytes?
Pure-PRP has not been implicated in much catabolic activities while L-PRP is known to induce catabolic effects. Treatment of tenocytes with PRP, likely P-PRP, did not influence the catabolic molecules, MMP-3 and MMP-13 [41]. In fact, the expression of MMP-13 in tenocytes decreased after PRP treatmentin vitro, and the platelet concentration negatively correlated with MMP-3 and MMP-13 levels [46]. However, PRCR upregulated MMP-1 and MMP-3 expression [44] likely because of the presence of large amounts of leukocytes in PRCR. In a recent study, we showed that L-PRP significantly induced the expression of MMP-1 and MMP-13 while P-PRP only slightly increased the expression of MMP-1 when compared to the control [39]. These studies clearly indicate that leukocytes in PRP are the key factors that induce catabolic actions in tendons/tendon cells.
Does PRP help tendon healing?
Thus far, numerous basic science studies have shown the beneficial effects of PRP in healing tendon injuries. Specifically, growth factors in PRP have significantly enhanced the healing of tendon injuries such as tendinopathy [21–24]. These include PDGF, TGF-β, VEGF, EGF, IGF-I, FGF, and HGF [24–26]. When platelets are activated, not only are the growth factors released, but PRP also forms a fibrin gel, which provides a conducive bioscaffold for migrating cells thus incorporating new cells for tendon healing [27]. Therefore, PRP can be regarded as a promising treatment option for tendinopathy. However, the efficacy of PRP to treat tendinopathy in clinical trials is still controversial. Therefore, in this review we discuss evidence for the use of PRP presented in basic science studies conductedin vitroandin vivo under well-controlled conditions to determine the basis of PRP applications in clinical settings.
Does PRP affect collagen?
PRP not only affects collagen but also affects the expression of other tendon related genes and proteins. For example, PRP treatment increased the mRNA and protein expression of tenocyte-related genes (scleraxis (SCX) and tenascin-C) by activating the focal adhesion kinase (FAK) and extracellular-regulated kinase (ERK) 1/2 signaling pathways [43]. Furthermore, PRP treatment has been shown to enhance the expression of COMP, decorin, and tenascin-C [35, 42–46]. COMP is a tendon healing related glycoprotein, which is abundant in the normal tendon but is depleted in fibrous scar tissue. Decorin is a matrix proteoglycan and is also abundant in the tendon and plays a role in matrix assembly by binding to collagen type I fibrils. Tenascin-C is also a glycoprotein abundant in developing tendons. These noncollagenous matrix markers are the indicators of matrix synthesis, and an increase in their expression by PRP treatment also signifies the beneficial anabolic effects of PRP on tendons.
Why do doctors use PRP?
Doctors may use PRP to reduce inflammation in people with OA and rheumatoid arthritis. This inflammation can lead to joints becoming painful and stiff.
What tissue is PRP used for?
Doctors first used PRP to help people heal after jaw and plastic surgeries. Examples of tissues that PRP has been used on include: tendons. ligaments. muscles. Ligaments can take time and be difficult to heal, which can make PRP an attractive option for some of those who have experienced injuries to this tissue group.
How many rounds of PRP injections are needed for knee injury?
A paper published in 2014, again in the American Journal of Sports Medicine, found that 3 rounds of PRP injections reduced symptoms in those with the knee injury chronic patellar tendinopathy. The researchers used 28 athletes in the study.
How much does a PRP treatment cost?
The cost of a single PRP treatment will typically be in the range of $ 500–2,500. People may also require repeat treatments.
Why do athletes need platelet rich plasma?
Platelet-rich plasma therapy has made headlines, often because it is favored by elite athletes to help them recover from injury. Some doctors are now using platelet-rich plasma therapy or PRP injections for several reasons, from encouraging hair growth to promoting soft tissue-healing. However, research studies have not definitively proved ...
How is platelet rich plasma administered?
Platelet-rich plasma therapy is administered through injections. Platelets are blood cells with several roles to play in the body. One is to promote blood clotting so that a person does not excessively bleed when they are cut. Another is to contain proteins in the blood that help wounds to heal. Researchers theorize that by injecting areas ...
Does PRP help with tendon damage?
A 2018 review also notes that PRP therapies may help reduce pain and improve healing in ligament and tendon damage cases. Still, the authors conclude that more research is necessary to fully assess the efficacy of the treatment.
Overview
Platelet-rich plasma (PRP), also known as autologous conditioned plasma, is a concentrate of platelet-rich plasma protein derived from whole blood, centrifuged to remove red blood cells. Though promoted to treat an array of medical problems, evidence for benefit is mixed as of 2020, with some evidence for use in certain conditions and against use in other conditions. The cost per injectio…
Medical use
Evidence for benefit of PRP is mixed, with some evidence for use in certain conditions and against use in other conditions. It has been investigated for chronic tendinitis, osteoarthritis, in oral surgery, and in plastic surgery.
A 2019 review found it not to be useful in rotator cuff disease. While an older review found that it may be useful. Tentative evidence supports its use in osteoarthritis (OA) of the knee. A 2019 met…
Adverse effects
Adverse effects have been poorly studied. The single systematic review of the literature did not report of the types and number of adverse events. In 2019, Health Canada stated that most autologous cell therapies have little evidence showing they work and can pose risks, such as cross-contamination between people if equipment is not sterilized properly or potentially dangerous immune reactions. Health Canada stopped Canadian clinics from offering these type…
Composition
There are four general categories of preparation of PRP based on its leukocyte and fibrin content: leukocyte-rich PRP (L-PRP), leukocyte reduced PRP (P-PRP; leukocyte reduced or pure PRP), leukocyte platelet-rich fibrin and pure platelet-rich fibrin.
The efficacy of certain growth factors in healing various injuries and the conce…
Manufacturing
PRP is prepared by taking blood from the person, and then putting it through two stages of centrifugation designed to separate PRP from platelet-poor plasma and red blood cells. This is usually done by the clinic offering the treatment, using commercially available kits and equipment. The resulting substance varies from person to person and from facility to facility, making it difficult to understand how safe and effective any specific use is.
Society and culture
The cost of a PRP treatment in the U.S. has been quoted as $1,000 out-of-pocket expenses, as it is usually not covered by health insurance. PRP has received attention in the popular media as a result of its use by athletes. Use in an office setting is not approved by the FDA.
In the 2010s, contentious cosmetic procedures marketed under the name of "vampire facials" grew in popularity, fueled by celebrity endorsement. These "vampire facials" generally center on …
See also
• Autologous blood injection
• Autologous conditioned serum
• Hypoxia preconditioned plasma
• Platelet-rich fibrin matrix
Platelet- Rich Plasma, A Brief History
What Is Plasma?
- Now that you have read a little on platelet-rich plasma, let’s deconstruct them one by one. So what is plasma? You’ve heard it before but what is it really and why is it relevant as a treatment to a lot of injuries? Plasma or blood plasma is the light- yellow to straw yellow liquid found in our blood. When we say “whole blood” this includes the red blood cells, the white blood cells, and the platel…
What Are Platelets?
- To understand platelet-rich plasma therapies, we must know the star of the show first, the platelet! You have heard it before in 3rdgrade but have you ever wondered why platelets are such important factors and why it has become one of the most studied cells of the body? Platelets are very small but despite the size, they have a lot of purpose in our bodies. The normal platelet cou…
What Is Platelet- Rich Plasma?
- Now, the part that I am excited to talk about— what is platelet-rich plasma and why all the fuss? Platelet-rich plasma is an efficient and minimally invasive (meaning there’s almost no pain and it is a very fast procedure!) method that is done by getting your own blood and separating the red blood cells from the plasma through the process, centrifuging. I promised to discuss centrifugin…
What Is It Used for?
- Since it has been around for more than 50 years, platelet-rich plasma has been used in medicine countless of ways:
How Is The Procedure done?
- As mentioned earlier, platelet-rich plasma is done in the office. A few tubes of your blood is extracted, and run on a centrifuge machine for 10 minutes. Once the platelet-rich plasma has been separated from the red blood cells, it will be extracted. We will then slowly inject the platelet-rich plasma that we have taken using very thin needles into the areas where you feel pain. Once thes…
Conclusion
- As discussed, PRP has become one of the emerging treatments for pain, especially of the tendons and bones. This is important especially when your injury is not only giving you pain but limiting you from doing all the things you love! To recap our discussion of platelet-rich plasma therapy here is what we covered: 1. Platelet- Rich Plasma, A Brief History 2. What is plasma? 3. What ar…