
Medication
Rehydration Therapy. Rehydration is the cornerstone of treatment for cholera. Oral rehydration salts and, when necessary, intravenous fluids and electrolytes, if administered in a timely manner and in adequate volumes, will reduce fatalities to well under 1% of all patients.
Therapy
Please consult the current CDC Cholera page for current cholera treatment recommendations. Rehydration therapy, meaning prompt restoration of lost fluids and salts through rehydration therapy is the primary goal of treatment. Antibiotic treatment, which reduces fluid requirements and duration of illness, is indicated for severe cases of cholera.
Self-care
Oral rehydration therapy (ORT) is a type of fluid replacement used to prevent and treat dehydration, especially that due to diarrhea.
Nutrition
From 2006 to 2011, UNICEF estimated that worldwide about a third of children under 5 who had diarrhea received an oral rehydration solution, with estimates ranging from 30% to 41% depending on the region.
What is rehydration therapy for cholera?
What are the current CDC treatment recommendations for cholera?
What is oral rehydration therapy?
What is the global prevalence of oral rehydration solutions for diarrhea?
WHO recommended Oral Rehydration Solution?
For more than 25 years, WHO and UNICEF have recommended a single formulation of glucose-based oral rehydration salts to prevent or treat dehydration from diarrhoea irrespective of the cause or age group affected.
Is oral rehydration therapy used for cholera?
Cholera requires immediate treatment because the disease can cause death within hours. Rehydration. The goal is to replace lost fluids and electrolytes using a simple rehydration solution, oral rehydration salts (ORS). The ORS solution is available as a powder that can be made with boiled or bottled water.
What is the function of oral rehydration therapy in cholera?
This treatment facilitates safe and optimal absorption of water and essential electrolytes such as sodium chloride, sodium bicarbonate and potassium chloride in dehydrated patients.
Who discovered oral rehydration therapy for cholera?
Captain Phillips of the US Army in 1964 first successfully tried oral glucose saline on two cholera patients. Following this, scientists working at the Cholera Research Laboratory, Dhaka, and the Infectious Diseases Hospital, Calcutta, contributed to the development of modern oral rehydration salt (ORS) solution.
WHO guideline for dehydration management?
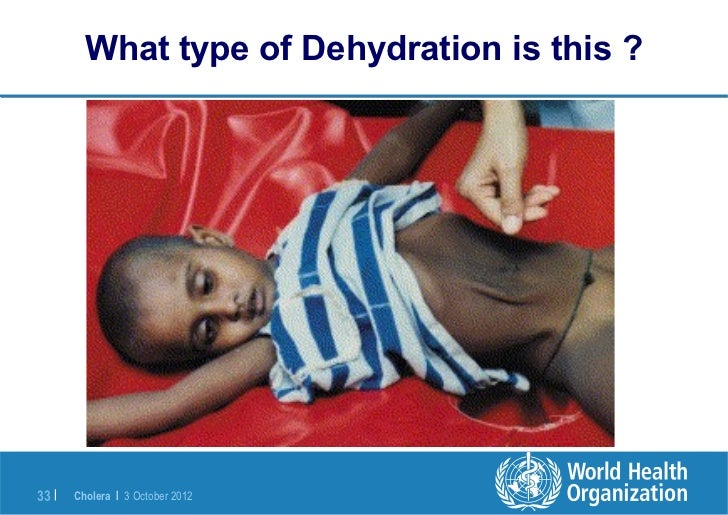
WHO (World Health Organisation) suggested management of dehydration secondary to diarrhoeal illnessassessmentfluid deficit as % of body weightfluid deficit in ml/kg body weightno signs of dehydration<5%<50 ml/kgsome dehydration5-10%50-100 ml/kgsevere dehydration>10%>100 ml/kg
Who dehydration treatment plan?
Prevent dehydration: – Encourage age-appropriate fluid intake, including breastfeeding in young children. – Administer ORS according to WHO Treatment Plan A after any loose stool....No dehydration.AgeQuantity of ORSChildren < 2 years50 to 100 ml (10 to 20 teaspoons)Children 2 to 10 years100 to 200 ml (½ to 1 glass)1 more row
What are the benefits of ORS?
An oral rehydration solution is used to treat moderate dehydration. It's made of water, glucose, sodium, and potassium. The combination optimizes the absorption of fluid in the intestines, which helps quickly replenish fluids. The solution is often used to treat dehydration due to diarrhea or vomiting.
What is the mechanism of oral rehydration therapy?
ORT uses the sodium-glucose cotransport mechanism to passively absorb water across the intestinal mucosa.
Who invented ORS in India?
Nonetheless, it was Hemendra Nath Chatterjee, a Bengali doctor, who first rehydrated his patients with “mild to moderately severe cholera … without intravenous or parenteral transfusions.” According to this paper, he “treated 186 patients with an oral glucose-sodium electrolyte solution” in 1953.
When was oral rehydration discovered?
Oral therapy was developed in the 1940s using electrolyte solutions with or without glucose on an empirical basis chiefly for mild or convalescent patients, but did not come into common use for rehydration and maintenance therapy until after the discovery that glucose promoted sodium and water absorption during cholera ...
When did oral rehydration therapy begin?
Since the World Health Organization began using ORT in 1978 as its primary means of fighting diarrhea, the annual death rate among children under 5 suffering from acute diarrhea has fallen from 5 million to fewer than 1 million.
What is the treatment for cholera?
Rehydration therapy, the primary treatment for cholera patients, refers to the prompt restoration of lost fluids and salts. Antibiotic treatment reduces fluid requirements and duration of illness, and is indicated for severe cases of cholera.
Can cholera cause diarrhea?
Most persons infected with the cholera bacterium have mild diarrhea or no symptoms at all. Only a small proportion, about 10%, of persons infected with Vibrio cholerae O1 may have illness requiring treatment at a health center.
What is the cause of cholera?
Cholera is an acute diarrhoeal infection caused by ingestion of food or water contaminated with the bacterium Vibrio cholerae. Cholera remains a global threat to public health and an indicator of inequity and lack of social development. Researchers have estimated that every year, there are roughly 1.3 to 4.0 million cases, ...
What is cholera outbreak?
In a country where cholera does not regularly occur, an outbreak is defined by the occurrence of at least 1 confirmed case of cholera with evidence of local transmission in an area where there is not usually cholera. Cholera transmission is closely linked to inadequate access to clean water and sanitation facilities.
How many people die from cholera annually?
Researchers have estimated that each year there are 1.3 to 4.0 million cases of cholera, and 21 000 to 143 000 deaths worldwide due to cholera (1) Most of those infected will have no or mild symptoms and can be successfully treated with oral rehydration solution.
How many cholera deaths were reported in 2019?
Uninfected dead bodies have never been reported as the source of epidemics. The number of cholera cases reported to WHO has continued to be high over the last few years. During 2019, 923 037 cases, 1911 deaths were notified from 31 countries (3).
When should OCV be used?
Based on the available evidence, the August 2017 WHO Position Paper on Vaccines against Cholera states that: OCV should be used in areas with endemic cholera, in humanitarian crises with high risk of cholera, and during cholera outbreaks; always in conjunction with other cholera prevention and control strategies;
How long does it take for cholera to show symptoms?
Symptoms. Cholera is an extremely virulent disease that can cause severe acute watery diarrhoea. It takes between 12 hours and 5 days for a person to show symptoms after ingesting contaminated food or water (2). Cholera affects both children and adults and can kill within hours if untreated.
What is the most at risk area for cholera?
Typical at-risk areas include peri-urban slums, and camps for internally displaced persons or refugees, where minimum requirements of clean water and sanitation are not been met.
When was oral rehydration therapy first used?
Oral rehydration therapy was developed in the 1940s, but did not come into common use until the 1970s. It is on the World Health Organization's List of Essential Medicines. Globally, as of 2015. [update] , oral rehydration therapy is used by 41% of children with diarrhea.
Who was the first person to use oral rehydration therapy?
In the early 1970s, Norbert Hirschhorn used oral rehydration therapy on the White River Apache Indian Reservation with a grant from the National Institute of Allergy and Infectious Diseases. He made the important observation that children would voluntarily drink as much of the solution as needed to restore hydration, and that rehydration and early re-feeding would protect their nutrition. This led to increased use of ORT for children with diarrhea, especially in developing countries.
How much osmolarity is needed for rehydration?
In 2003, WHO and UNICEF recommended that the osmolarity of oral rehydration solution be reduced from 311 to 245 mOsm/L . These guidelines were also updated in 2006. This recommendation was based on multiple clinical trials showing that the reduced osmolarity solution reduces stool volume in children with diarrhea by about twenty-five percent and the need for IV therapy by about thirty percent when compared to standard oral rehydration solution. The incidence of vomiting is also reduced. The reduced osmolarity oral rehydration solution has lower concentrations of glucose and sodium chloride than the original solution, but the concentrations of potassium and citrate are unchanged.
What is ORT for dehydration?
ORT is suitable for people who are not dehydrated and those who show signs and symptoms of mild to moderate dehydration. People who have severe dehydration should seek professional medical help immediately and receive intravenous rehydration as soon as possible to rapidly replenish fluid volume in the body.
What is ORT treatment?
eMedicine. 906999-treatment. [ edit on Wikidata] Oral rehydration therapy ( ORT) is a type of fluid replacement used to prevent and treat dehydration, especially due to diarrhea. It involves drinking water with modest amounts of sugar and salts, specifically sodium and potassium.
How long does zinc help with rehydration?
Zinc. As part of oral rehydration therapy, the WHO recommends supplemental zinc (10 to 20 mg daily) for ten to fourteen days, to reduce the severity and duration of the illness and make recurrent illness in the following two to three months less likely.
When did rehydration therapy become a part of the WHO?
In the early 1980s, "oral rehydration therapy" referred only to the preparation prescribed by the World Health Organization (WHO) and UNICEF. In 1988, the definition changed to encompass recommended home-made solutions, because the official preparation was not always readily available.
What is the rehydration phase of diarrhoea?
ORAL REHYDRATION THERAPY IN INFANTILE DIARRHOEA Infants (defined here as children under 2 years of age) with diarrhoea require special attention during; (a) the rehydration phase, i.e., the replacement of the water and electrolyte deficit present at the time of starting therapy; and (b) the maintenance phase, i.e., the replacement of continuing losses (due to diarrhoea and vomiting) and the provision of additional plain water requirements. The plain water requirement is due to the relatively larger surface area and higher metabolic rate per unit of body mass in infants, who therefore require about two and a half times more water per kilogram of body weight than adults.32
Does oral rehydration help with weight gain?
WP/05 page 5 that infants who received oral rehydration therapy together with proper dietary management (using the available foods) during and after the diarrhoea had a better appetite and gained significantly more weight than controls over a 7-month period of observation.52 Similar studies subsequently carried out in Egypt,53 Iran,54 Liberia55 and Turkey56 showed a similar trend in weight gain in children who received oral rehydration therapy and dietary management during episodes of acute diarrhoea. Prepackaged ORS was used in all these studies. The precise mechanism of the weight gain is not clear, although correction of acidosis and replacement of potassium losses probably played a role in hastening the improvement of appetite. All these studies indicate that oral rehydration therapy may have an important nutritional benefit, and emphasize the value of a complete rehydration formula and proper dietary education of mothers. 5. EXPERIENCE WITH ORAL THERAPY IN TREATMENT CENTRES Since the early studies in Bangladesh and India, oral rehydration has gained worldwide acceptance and use in treatment centres. One of the earliest and most dramatic demonstrations of its efficacy and benefit was its use, under the most difficult field conditions, in the maintenance of hydration in severely dehydrated Bangladesh refugees during the 1971 civil upheaval.57 Many countries in Africa and Asia had their initial experience with oral rehydration therapy in cholera outbreaks (during the present pandemic) and obtained remarkable successes, e.g., during the cholera outbreak in the Maldives in 1978.58 Studies in some countries have shown that the use of oral rehydration therapy can result in a great reduction in the amount of intravenous fluid used in the treatment centres. For example, two hospitals in India reported savings of 70% of the expenses previously incurred for intravenous fluid after appropriate use of oral fluid.45,59 There are also some data indicating that reduction in the use of intravenous therapy can be accompanied by a marked decrease in nosocomial infections and hoapital mortality in diarrhoea cases.60,61 There is no doubt that intravenous fluid will continue to be needed in treatment centres for the rehydration of diarrhoea cases with severe dehydration or other complications (e.g., persistent vomiting, poor mental state, concurrent infections), but these cases constitute no more than 5-10% of all cases seen at such centres. 6. DELIVERY OF ORAL REHYDRATION AT THE PERIPHERY Increasing attention is now being focused on extending the delivery of oral therapy, as a primary health care activity, to the village and household levels, where an even greater. impact on reducing the mortality in children under five years of age can be expected. Therapy at these levels, if applied properly and early in the course of the illness, can prevent the-development of.severe dehydration and thus reduce the need for intravenous therapy and hospitalization. Field evaluations of the effectiveness of early oral rehydration therapy are being undertaken. In a limited study carried out in Bangladesh, home delivery of oral rehydration solution by trained village health workers resulted in a reduction of 29%, over a 4-month period, in the number of cases seeking therapy at a rural treatment centre.62 A more recent study in Bangladesh, carried out over a longer period, showed a significant reduction in case-fatality rates when ORS packets were made easily available through trained village-based volunteer workers and after a short promotional campaign had been conducted to inform the village population.40 Other field evaluations of oral rehydration therapy are now being carried out or are planned as an integrated activity in populations served by multi-purpose village health workers in a number of countries, including Bangladesh, Coata Rica, Egypt, India, and Nepal.
What is oral rehydration solution?
Oral rehydration solution (ORS) was established as the cornerstone of therapy for dehydration secondary to acute infectious diarrhea approximately 40 years ago . The efficacy of ORS is based on the ability of glucose to stimulate Na and fluid absorption in the small intestine via a cyclic AMP-independent process. Despite the establishment that ORS is the primary reason for the substantial reduction in morbidity and mortality from diarrhea in children in developing countries, the use of ORS has lagged for many reasons. This review highlights efforts to establish a major reformulation of ORS following the demonstration that short-chain fatty acids (SCFA) stimulate colonic Na and fluid absorption by a cyclic AMP-independent mechanism. The addition of high-amylose maize starch (HAMS), a microbially-fermentable (or ‘resistant’) starch, to ORS results in delivery of non-absorbed carbohydrate to the colon where it is fermented to SCFA. To date, three randomized controlled trials with a HAMS-ORS in south India have demonstrated a substantial decrease in diarrhea duration in both adults and children hospitalized for acute diarrhea. Significant efforts are now underway to establish this dual-action, modified HAMS-hypoosmolar ORS solution as the standard ORS for the treatment of dehydration from acute diarrhea.
Can esterified starches be used in clinical trials?
In order to proceed to clinical trials with these esterified starches another problem required attention. Most of these starches when added to a glucose–electrolyte solution did not yield a clear solution but rather had an opaque appearance that, over a short period of time, often just 1 h, would settle out of suspension. As a result, efforts were required to identify one or more suspending agents that would ensure that, even without stirring, a child would receive the desired amount. These ORS formulations containing an anti-settling agent were also studied in the in vivo whole gut perfusion system. These studies demonstrated that there was no loss of the advantages provided by the esterified HAMS solutions with varying amounts of acetylation compared to the HAMS-ORS formulation (unpublished observations). As a consequence, clinical trials have been designed and recently started to determine which of these three HAMS-related ORS formulations each containing a suspending agent will result in greater efficacy in the treatment of acute diarrhea in adults. Such a compound will then be selected for more detailed studies including safety, efficacy in both adults and children, and, most importantly, in different areas of the developing world to establish its efficacy with several different pathogenic agents.
Does cholera cause diarrhea?
The second critical observation was the result of several studies that established that: (1) cholera enterotoxin caused diarrhea in clinical cholera by inducing fluid and electrolyte secretion via activation of adenylate cyclase resulting in an increase in cyclic AMP in intestinal epithelial cells [7]; and (2) the action of cyclic AMP on intestinal epithelial transport included both stimulation of active Cl secretion and inhibition of electroneutral Na-Cl absorption (which represents the coupling of parallel ion exchanges—Na-H and Cl-HCO3) [8]. However, most critical to the development of ORS was that cholera enterotoxin (i.e., cyclic AMP) did not inhibit glucose-stimulated Na and thus fluid absorption (Fig. 1). Thus, the physiological basis of ORS rests on the demonstration that absorptive and secretory processes in the mammalian small intestine are separate and independent; that cholera-toxin-mediated cyclic AMP-induced active Cl secretion does not affect glucose-induced Na absorption; and conversely and most important, glucose stimulates Na absorption via a cyclic AMP-independent transport process (despite the stimulation of active Cl secretion by cyclic AMP) [7–10]. In addition, it was recently shown that glucose has an additional effect that will increase Na and fluid absorption: glucose reverses cyclic AMP’s down-regulation of Na-H exchanger 3 (NHE3) [11].

Symptoms
History
Vibrio cholerae Strains
Epidemiology, Risk Factors, and Disease Burden
Specialist to consult
Prevention and Control
Surveillance
Water and Sanitation Interventions
Treatment
Community Engagement
Oral Cholera Vaccines