A parent or guardian can give consent (in most cases) or a child can give their consent to medical treatment if they’re capable of understanding its significance. Someone else may consent to medical treatment on behalf of an adult if there is: Some decisions about special medical procedures must be made by a court or tribunal.
Who may consent to medical treatment?
There physicians are often faced with the question of just who may consent to treatment and under what circumstances? In most states, age 18 is the age of majority and thus, before treating a patient under the age of 18, consent must be obtained from the patient’s parent or legal guardian.
What are the essentials of a valid medical consent?
Medical ethics and international human rights law necessitate consent as a prerequisite for initiating medical treatment. The essentials of a valid consent are: The patient must be informed of all the information regarding the treatment before the application; and The patient must be capable of giving consent.
Who can give consent on the behalf of a minor?
In these cases, the parent or guardian of the child must give consent on the minor’s behalf.
When can a child give consent to a medical procedure?
In general, children aged 16 or over may themselves give consent to surgical, medical or dental procedures, without requiring the consent of their parents or guardians. This is provided for in the Non-Fatal Offences Against the Person Act 1997.
Who can provide informed consent?
Informed consent can only be obtained from an adult patient who is mentally competent to do so except under some circumstances and situations.
Can family members make medical decisions?
A legal surrogate. Even when nobody has named you as a health care agent, you may still be asked to make medical decisions for someone else. If you are a family member or possibly a close friend, you may be called upon to make decisions as the default decision-maker.
What criteria is needed for someone to give consent to a procedure?
Valid informed consent for research must include three major elements: (1) disclosure of information, (2) competency of the patient (or surrogate) to make a decision, and (3) voluntary nature of the decision. US federal regulations require a full, detailed explanation of the study and its potential risks.
Can nurses give informed consent?
As nurses, we deal with informed consent a lot—on admission to a hospital/clinic or before a procedure/surgery. Nurses typically are assigned the task of obtaining and witnessing written consent for healthcare treatment.
Who can make decisions for patients?
When a patient lacks decision-making capacity, the physician has an ethical responsibility to: Identify an appropriate surrogate to make decisions on the patient's behalf: The person the patient designated as surrogate through a durable power of attorney for health care or other mechanism.
Who is next of kin to make medical decisions?
In most states, the default surrogate decision maker for adults is normally the next of kin, specified in a priority order by state statute, typically starting with the person's spouse or domestic partner, then an adult child, a parent, a sibling, and then possibly other relatives.
Who can witness informed consent?
Any member of the healthcare team may sign as a witness to the patient's signature, although this serves only to verify that it was the patient who signed the form. The witness does not obtain consent or verify the patient's competency to give consent.
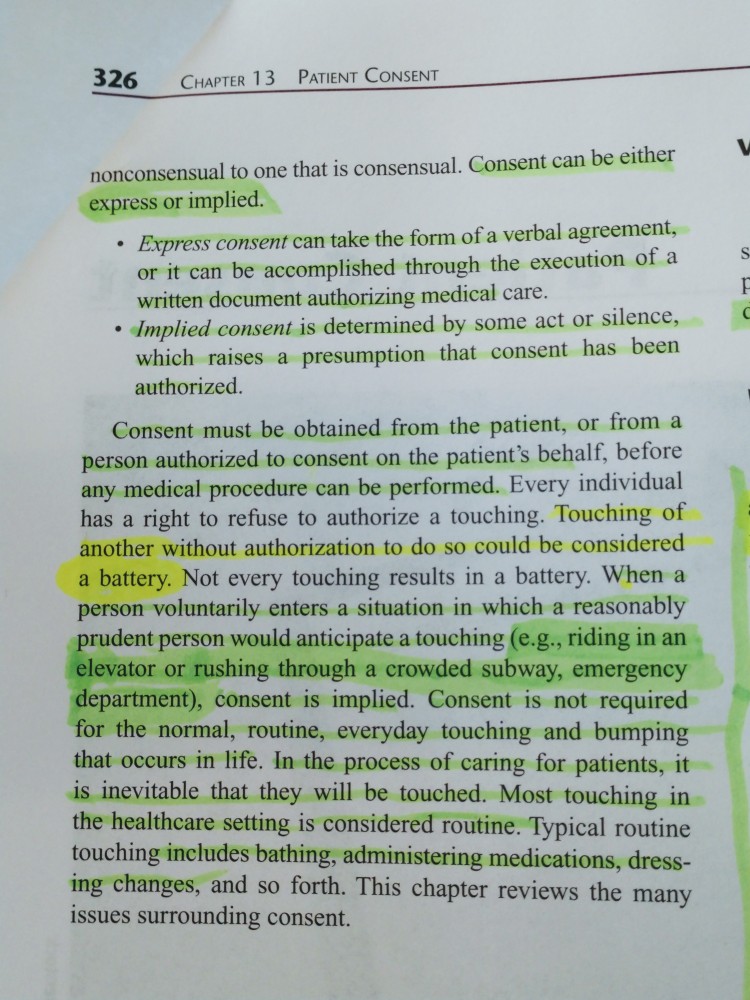
What are the 4 types of consent?
Implied Consent. Participation in a certain situation is sometimes considered proof of consent. ... Explicit Consent. ... Active Consent. ... Passive Consent. ... Opt-Out Consent. ... Key Takeaway.
Can next of kin give consent in an emergency?
What does a next of kin do? They act on your behalf if you are unable to communicate due to illness or being unconscious. They will be asked for advice and guidance on your wishes. In the event of your death, they may need to give permission for a 'consented postmortem'.
Who is responsible for obtaining informed consent in a clinical trial?
For all FDA-regulated clinical investigations (except as provided in 21 CFR 50.23 and 50.24 5), legally effective informed consent must be obtained from the subject or the subject's legally authorized representative.
Can a physician delegate informed consent?
Court Rules Informed Consent Cannot Be Delegated The duty to obtain informed consent belongs solely to the physician and cannot be delegated." The court held that a physician cannot rely upon a subordinate to disclose vital information and obtain informed consent.
Who provides informed consent for treatment?
As a result, it is the minor’s parents who provide the informed consent for treatment. There are exceptions to this rule, however, and they include if the minor is married, if the minor is pregnant, or if the minor is considered “emancipated”. 2 Each state has its own laws concerning exceptions to the general rule, ...
What is the role of informed consent?
So, with your employer’s policy as a guide, what is your role in obtaining the informed consent of the patient? Generally, you are responsible for: 1 Ensuring that the consent form is signed by the appropriate person—e.g., the patient, the guardian, the agent under a durable attorney for health care. Your only role is as a witness to the person putting his or her signature on the form and dating the form. The forms provide a place for your signature as the witness and the date as well; 2 Document that the signature was obtained, including the date and time in the nursing notes; 3 If the patient seems confused about the procedure or has additional questions, your role is one of an advocate for the patient. Instruct the patient not to sign the form until the requested information is obtained, notify the appropriate health care provider (e.g., physician, surgeon, nurse practitioner) and document same; 4 You can explain the nursing care that will take place after the procedure or treatment, what medications you administered or will administer, and any other aspect of nursing care; and 5 Provide comfort and support to the patient and his family or guardian while waiting for the procedure or treatment to begin.
What is the role of a witness in a medical form?
Your only role is as a witness to the person putting his or her signature on the form and dating the form. The forms provide a place for your signature as the witness and the date as well; If the patient seems confused about the procedure or has additional questions, your role is one of an advocate for the patient.
What is the National Consent Policy?
The National Consent Policy app lies to services provided by or on behalf of the Health Service Executive (HSE). The National Consent Policy and guides are available for download. These include guides for patients, professionals and young people.
What happens if you don't give consent to a procedure?
If there is no consent. If a person carries out medical or surgical procedures without consent, they could be charged with the crime of assault - the decision on charges is made by the Director of Public Prosecutions. They could also be sued for the torts (civil wrongs) of assault and/or battery and possibly for breach of constitutional rights.
What happens if you are not mentally competent?
If you are not mentally competent, you are not in a position to make a decision about refusing or discontinuing medical treatment. The law is not clear on exactly who is competent to do this.
What is informed consent?
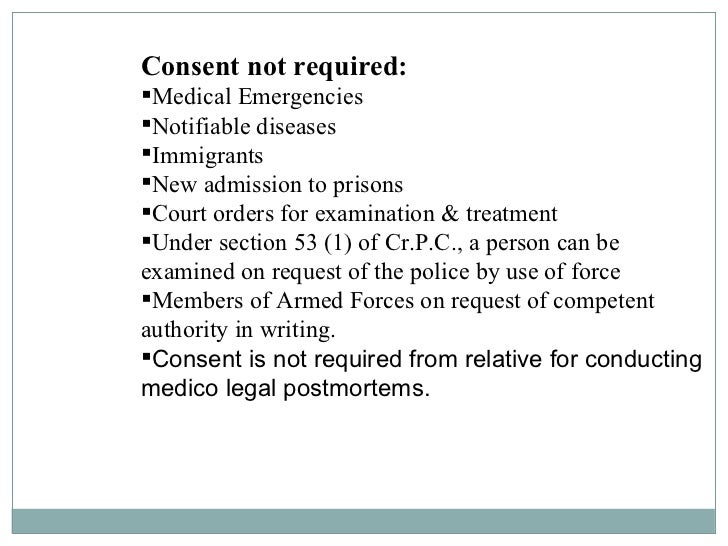
In general, valid consent must be informed consent, where the patient has enough information to be able to understand what is proposed and the potential risks and benefits. The patient must have the capacity to make the decision and must be free to do so without threat or pressure from others. The Assisted Decision-Making (Capacity) ...
Can a doctor give or withhold consent?
If you are seriously ill and not in a position to give or withhold consent, the doctor may carry out what would be considered usual procedures arising from necessity. Sometimes doctors may consult with your family or nearest relatives but they really have no legal right to give or withhold consent.
Can a 16 year old give consent to a dental procedure?
In general, children aged 16 or over may themselves give consent to surgical, medical or dental procedures, without requiring the consent of their parents or guardians. This is provided for in the Non-Fatal Offences Against the Person Act 1997.
Does the Advance Healthcare Directive Act have a power of attorney?
The Act also provides a statutory framework for Advance Healthcare Directives. The Act has not yet been commenced to bring it into effect in these areas. An enduring power of attorney does not presently give the attorney the power to make decisions of this nature on behalf of the person granting the power.
What happens if a doctor doesn't give consent?
If a doctor fails to obtain informed consent for non-emergency treatment, he or she may be charged with a civil offense like gross negligence and/or a criminal offense such as battery or gross negligence which is the unauthorized touching of the plaintiff's person. In a civil suit, the patient would have to show two elements. Medical treatment could be unauthorized because the doctor didn’t fully explain either the procedure or the risks associated with the procedure. First, the patient must show that the doctor performed the treatment or procedure without her informed consent. Second, the patient has to show that had she known about the risks of the procedure, she would’ve decided not to have it done and, therefore, avoided the injury.
What is informed consent?
Informed Consent. Virtually all states have recognized, either by legislation or by common law, the right to receive information about one's medical condition, treatment choices, risks associated with the treatments, and prognosis.
Why is medical treatment unauthorized?
Medical treatment could be unauthorized because the doctor didn’t fully explain either the procedure or the risks associated with the procedure. First, the patient must show that the doctor performed the treatment or procedure without her informed consent.
Is informed consent legal?
The informed consent process isn’t only an ethical obligation for doctors -- it is also a legal one. State laws often take a patient-centered approach.
Can a minor give consent to medical treatment?
Minors, unlike adults, are generally presumed to be incompetent. Therefore, they are unable to give consent to medical treatment and procedures. In these cases, the parent or guardian of the child must give consent on the minor’s behalf.
Is a patient considered competent?
In order to give his or her informed consent, a patient must be competent. Generally, adults are presumed to be competent. However, this presumption can be challenged in cases of mental illness or other impairments. Minors, unlike adults, are generally presumed to be incompetent.
What is the law that allows a minor to give consent to HIV testing?
Laws that explicitly allow a minor to give informed consent to HIV testing, treatment, and/or prophylaxis, including pre-exposure prophylaxis (PrEP), or. Laws that allow a minor to give informed consent to general health care, services, or procedures. As of 2020, all jurisdictions have laws that explicitly allow a minor of a particular age ...
Can a minor give consent to HIV treatment?
Jurisdictions have different types of laws, and the age at which the minor has the legal right to provide informed consent to receive STD or HIV services varies by jurisdiction: Laws that explicitly allow a minor to give informed consent to receive STD diagnosis and treatment, and/or prevention. Laws that explicitly allow a minor ...
Who can consent to treatment for children?
The issue of who can consent for treatment in children can, in certain situations, be a difficult one to judge and MDDUS advisers have dealt with a number of calls from members seeking advice on this topic. It is important to remember the basic principle that, generally, only a person with what is known as "parental responsibility" can consent ...
Who can consent to treatment in children who lack capacity?
ACTION: Only someone with parental responsibility – or authorisation from a parent – can consent to treatment in children who lack capacity, except in an emergency.
What are exceptions to the rule of parental responsibility?
Exceptions to the rule of parental responsibility include carers authorised by a parent and emergency situations where essential treatment can be provided to preserve life or prevent serious deterioration. The GMC offers more detail in its guidance 0-18 years, which states:
Who can do what is reasonable in all the circumstances of the case to safeguard or promote the child's welfare?
The GMC offers more detail in its guidance 0-18 years, which states: “People without parental responsibility, but who have care of a child, may do what is reasonable in all the circumstances of the case to safeguard or promote the child’s welfare. This may include step-parents, grandparents and childminders.
Can a parent consent to dental treatment?
It is important to remember the basic principle that, generally, only a person with what is known as "parental responsibility" can consent to a child’s medical or dental treatment (assuming the child does not have the capacity to give consent themselves). Once it has been established that the child is not legally competent ...
