Medication
Treatment
- Prevent the clot from getting bigger.
- Prevent the clot from breaking loose and traveling to the lungs.
- Reduce your chances of another DVT.
Self-care
Treatment of DVT aims to prevent pulmonary embolism, reduce morbidity, and prevent or minimize the risk of developing post-thrombotic syndrome. The cornerstone of treatment is anticoagulation. NICE guidelines only recommend treating proximal DVT (not distal) and those with pulmonary emboli.
Nutrition
A Turkish health care firm has developed a treatment for acute deep vein thrombosis (DVT). The MANTIS Thrombectomy ... and 10% of these deaths occur before the diagnosis is made within the first hour of the onset of symptoms, it added.
What is the optimal duration of treatment for DVT?
Your doctor will decide the duration of your treatment. After at least 6 months of treatment for DVT/PE, your doctor may ask you to continue on a lower dose of ELIQUIS to help reduce the risk of them happening again. How long one takes ELIQUIS generally varies from patient to patient.
What is DVT and how can you treat it?
What is the initial treatment of DVT?
How long do you take Eliquis for DVT?
Explore

What is high risk DVT?
You're at greater risk of developing a deep-vein blood clot if you're overweight or obese or if you have a family history of DVT, pulmonary embolisms, or clotting disorders. Your risk also goes up if you're a smoker.
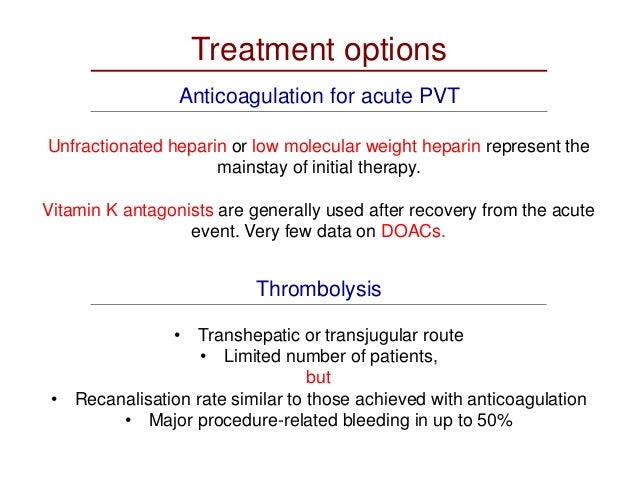
How is acute DVT treated?
For acute DVT, initial anticoagulation should be one of the following regimens: 1) apixaban 10 mg twice a day for 7 days, then 5 mg twice a day; 2) dabigatran 150 mg twice a day after a 5- to 10-day lead-in course of LMWH; 3) edoxaban 60 mg daily (30 mg if creatinine clearance 30-50 ml/min or potent proton pump ...
What medications increase risk of DVT?
Certain medications (eg, birth control pills, hormone replacement therapy, tamoxifen, thalidomide, erythropoietin, cancer chemotherapy medications). The risk of a blood clot is further increased in people who use one of these medications and also have other risk factors.
Which surgery has highest risk of DVT?
Orthopedic surgery procedures, hip or knee replacement, femur fractures and the like, are the ones that are most frequently accompanied by DVT ( VTE – your choice, again), comprising 30% of the cases followed by cancer (15%), digestive (13%), genitourinary (10%), and brain surgery (less than 10%).
What is the first line treatment for DVT?
Use of direct oral anticoagulants (DOACs) are recommended as first-line treatment of acute DVT or PE. DOAC therapy is preferred over vitamin K antagonists (VKAs) for most patients without severe renal insufficiency (creatinine clearance <30 ml/min), moderate-severe liver disease, or antiphospholipid antibody syndrome.
What is acute DVT?
Acute deep vein thrombosis or DVT, is a common condition that occurs in the legs of men and women of all ages. It causes leg swelling, pain and can limit walking. The larger the blood clot, the greater the number of veins that are damaged and the more severe are the symptoms.
Why do NSAIDs increase risk of blood clots?
NSAIDs work by blocking a specific group of enzymes called cyclo-oxygenase enzymes (COX enzymes). These enzymes are involved in the production of prostaglandins which control many different processes such as inflammation, blood flow, and the formation of blood clots.
Which type of DVT is at lesser risk of embolisation?
Deep veins of the legs Calf vein DVT is less likely to be a source of large emboli but can propagate to the proximal thigh veins and from there cause PE. About 50% of patients with DVT have occult PE, and at least 30% of patients with PE have demonstrable DVT.
What is the drug of choice for DVT?
Two older anticoagulants used to help prevent and treat DVT are heparin and warfarin. Heparin comes as a solution that you inject with a syringe. Warfarin comes as a pill you take by mouth. Both of these drugs work well to prevent and treat DVT.
Does general anesthesia increase risk of DVT?
General anesthesia has been associated with higher risk of DVT than spinal or epidural anesthesia. A study of orthopedic surgery patients found that duration of anesthesia >3.5 hours was a strong risk factor for postoperative VTE regardless of the route of anesthesia.
What increases risk of thrombosis?
Who is at risk for a blood clot? Blood clots can affect anyone at any age, but certain risk factors, such as surgery, hospitalization, pregnancy, cancer and some types of cancer treatments can increase risks. In addition, a family history of blood clots can increase a person's risk.
What is the first line of treatment for acute DVT?
Patients with submassive (intermediate-high risk) or massive PE as well as patients at high risk for bleeding may benefit from hospitalization. Use of direct oral anticoagulants (DOACs) are recommended as first-line treatment of acute DVT or PE.
How long does it take to treat DVT?
The ASH guidelines define the treatment period of acute DVT/PE as “initial management” (first 5-21 days), “primary treatment” (first 3-6 months), and “secondary prevention” (beyond the first 3-6 months).
What is the ASH recommendation for DVT?
The ASH guidelines suggest against the routine use of prognostic scores, D-dimer testing, or venous ultrasound to guide the duration of anticoagulation. For patients with breakthrough DVT and/or PE while on therapeutic VKA treatment, the ASH guidelines suggest using low molecular weight heparin over DOAC therapy.
How often do DVT and PE occur?
The ASH assembled a multidisciplinary writing committee to provide evidence-based guidelines for management of DVT and PE, which occur 300,000-600,000 times annually in the United States. The ASH guidelines suggest home treatment over hospitalization for patients with uncomplicated acute DVT.
Can you use compression stockings for DVT?
For patients with acute DVT who are not at high risk for post-thrombotic syndrome, the ASH guidelines recommend against the routine use of compression stockings. However, select patients may benefit from compression stockings to help with edema and pain associated with acute DVT. Share via:
Is thrombolysis considered a high risk procedure?
Thrombolysis is reasonable to consider for patients at low bleeding risk who are at high risk for decompensation. For patients with extensive DVT in whom thrombolysis is considered appropriate, the ASH guidelines suggest using catheter-directed thrombolysis over systemic thrombolysis.
Why is anticoagulant treatment important?
Initial anticoagulant treatment is crucial for reducing mortality, preventing early recurrences, and improving long-term outcome. Treatment and patient disposition should be tailored to the severity of clinical presentation, to comorbidities, and to the potential to receive appropriate care in the outpatient setting.
How common is venous thromboembolism?
Venous thromboembolism (VTE) is a common disease with an average annual age- and sex-adjusted incidence of 123 per 100 000 person-years in the United States. 1 According to recent estimates, the incidence of VTE is 131 per 100 000 person-years in Europe. 2 The clinical manifestation of VTE is deep vein thrombosis (DVT) in the majority of the patients; pulmonary embolism (PE) with or without concomitant DVT accounts for 30% to 40% of the cases. 3 The incidence of PE seems to have increased in recent years, 4 probably because of a heightened awareness of the disease, around-the-clock availability of computed tomography (CT) angiography, and greater sensitivity of imaging techniques. 5
Can a vena cava filter be used for VTE?
Insertion of a vena cava filter is not a treatment for VTE; instead, it is an attempt to block emboli from migrating from the lower limbs to the lung. Having inserted a vena cava filter does not eliminate the need for anticoagulant treatment. 67 In fact, insertion of a vena cava filter is associated with increased risk for proximal extension of DVT, and there is the potential for increased mortality if therapeutic anticoagulation is not started in patients with either initial DVT or PE. 68,69 In patients with absolute contraindications to anticoagulant treatment, a vena cava filter may reasonably reduce the risk of PE until anticoagulation can be started. Careful reassessment of bleeding risk should be scheduled in patients who had a vena cava filter inserted so that anticoagulation can be started as soon as possible. 8,11 Whether the insertion of a vena cava filter is beneficial in hemodynamically unstable PE patients and before catheter-directed thrombolysis in patients with DVT requires additional study.
Is anticoagulation used for VTE?
In conclusion, acute treatment of VTE has an essential role in reducing the risk for adverse outcome events. Therapeutic anticoagulation should be used in all VTE patients in the absence of absolute contraindications.
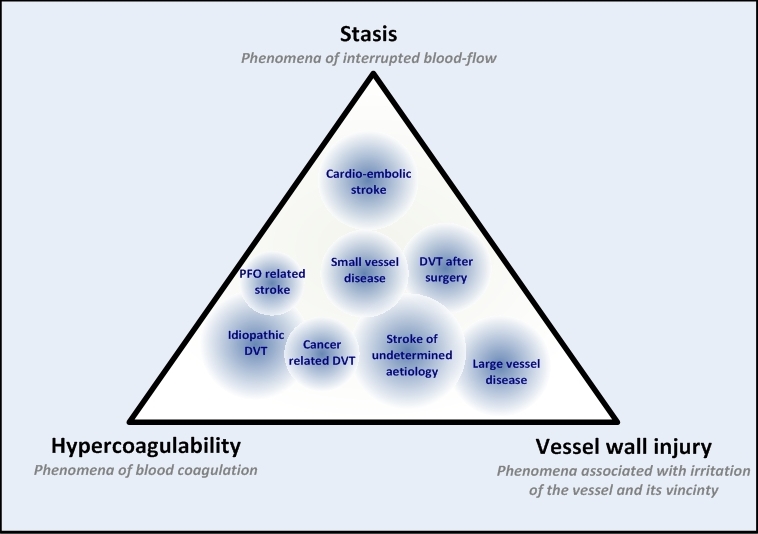
What is the pathophysiology of venous thrombosis?
The pathophysiology of venous thrombosis has been famously described by Rudolf Virchow, known as the Virchow's triad, which includes stasis, endothelial injury, and hypercoagulability. [1] Venous thrombosis can be superficial venous thrombosis, or deep venous thrombosis (DVT), the latter will be the focus of this article.
What are the risk factors for a woman's thrombophilia?
The risk is greatest in the post-partum period, and in women with multiple pregnancies. The presence of other risk factors such as antiphospholipid antibodies, inherited thrombophilias, obesity, increased maternal age, hypertension, diabetes mellitus, smoking, and obesity further increases the risk.
What is the most concerning complication with high mortality?
The most concerning complication with high mortality is associated with pulmonary embolism (PE) secondary to venous thromboembolism (VTE). The pathophysiology of venous thrombosis has been famously described by Rudolf Virchow, known as the Virchow's triad, which includes stasis, endothelial injury, and hypercoagulability. [1] .
What are preventive strategies?
Preventive strategies such as the use of pneumatic devices and prophylactic anticoagulation are a standard of care in hospital medicine, and such strategies are based on the identification of the underlying risk factors in an individual patient. Issues of Concern. Deep Venous Thrombosis Risk Factors.
What is the probability of a high risk D-dimer?
Medium risk carries a 17% likelihood, and either a high-sensitivity D-dimer can be used or forgone in place of a Doppler study, with a single negative test being sufficient. High risk has a prevalence of 17% to 53%, and US doppler is recommended, although it may not be sufficient.
What is the clotting risk for breast cancer?
Advanced breast or breast cancer treated with chemotherapy has a 10% rate of clinically significant VTE. Clotting risk in cancers treated with chemotherapy is highest during the induction phase, especially when treated with fluorouracil, tamoxifen, or L-asparaginase.
Does smoking cause DVT?
Smoking and obesity both have been associated with a higher risk for DVTs . [6][7] Acquired. Several risk factors can contribute to the development of DVTs, and more than 50% of patients who suffer a DVT have more than one acquired risk factor.
Diagnosis
Clinical Trials
Lifestyle and Home Remedies
Preparing For Your Appointment