If a patient with bradycardia
Bradycardia
Heart rate slower than 60 beats per minute.
How to cure bradycardia naturally?
Apr 17, 2022 · Which situation does bradycardia require treatment? Patients with imminent heart failure or unstable patients with bradycardia need immediate treatment. The drug of choice is usually atropine 0.5–1.0 mg given intravenously at intervals of …
How serious is bradycardia?
Dec 26, 2018 · In which situation does bradycardia require treatment? (a) 12-lead ECG showing a normal sinus rhythm (b) Hypotension (c) Diastolic blood pressure > 90 (d) Systolic blood pressure > 100 (b) Hypotension. A 67 yr old woman has palpitations, chest discomfort, and tachycardia. The monitor shows a regular wide-complex QRS at a rate of 180/min.
When does bradycardia require treatment ACLS?
Sep 20, 2021 · Patients with impending heart failure or unstable patients with bradycardia require immediate treatment. The preferred drug is usually 0.5 to 1.0 mg atropine administered intravenously at 3-5 minute intervals up to a dose of 0.04 mg / kg. Other auxiliary drugs that can be given are adrenaline (adrenaline) and dopamine. What drugs are used in ACLS?
What is the most common bradycardia treatment?
Sometimes bradycardia is a good thing and is the goal of treatment. If you need treatment, it will be based on the cause of the condition. If you have an electrical problem in your heart, you will need a pacemaker to keep your heart beating as it should. A pacemakers is a small device that is placed under your skin to monitor your heart’s rate and rhythm.

In what situation does bradycardia require treatment ACLS?
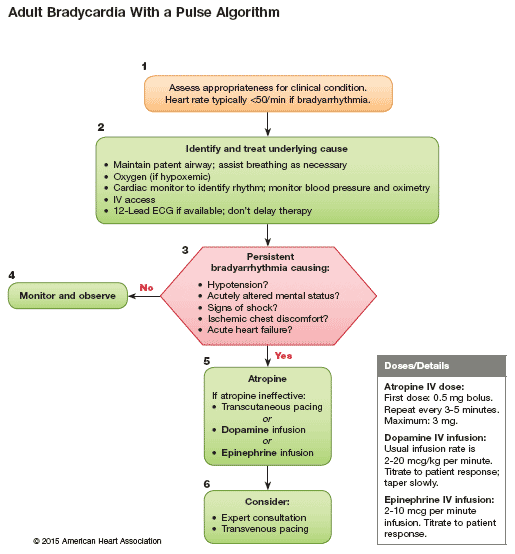
Regardless of the patient's rhythm, if their heart rate is too slow and the patient has symptoms from that slow heart rate, the bradycardia should be treated to increase the heart rate and improve perfusion, following the steps of the bradycardia algorithm below.
Does bradycardia require treatment?
Treatment for bradycardia depends on the severity of symptoms and the cause of the slow heart rate. If you don't have symptoms, treatment might not be necessary. Bradycardia treatment may include lifestyle changes, medication changes or an implanted device called a pacemaker.Oct 20, 2021
When does sinus bradycardia require treatment?
A patient with sinus bradycardia should be evaluated for hemodynamic instability. If found to be hemodynamically unstable, the patient can be treated with intravenous (IV) atropine 0.5 mg push every 3 to 5 minutes up to 3 mg total.Aug 9, 2021
Does bradycardia require treatment with hypotension?
Provide immediate therapy for patients with hypotension, acute altered mental status, chest pain, congestive heart failure, seizures, syncope, or other signs of shock related to the bradycardia (Box 4). AV blocks are classified as first, second, and third degree.Nov 28, 2005
What is the best treatment for irregular heartbeat?
Therapies to treat heart arrhythmias include vagal maneuvers and cardioversion to stop the irregular heartbeat.Vagal maneuvers. If you have a very fast heartbeat due to supraventricular tachycardia, your doctor may recommend this therapy. ... Cardioversion.Oct 1, 2021
When does bradycardia require a pacemaker?
Your doctor may recommend a temporary pacemaker when you have a slow heartbeat (bradycardia) after a heart attack, surgery or medication overdose but your heartbeat is otherwise expected to recover. A pacemaker may be implanted permanently to correct a chronic slow or irregular heartbeat or to help treat heart failure.Dec 2, 2021
What happens if bradycardia is left untreated?
When bradycardia is more severe, you may experience shortness of breath, chest pain, and fainting. If severe bradycardia goes untreated, it could lead to cardiac arrest, meaning the heart stops beating, and that can lead to death. Not everyone with bradycardia has symptoms.Aug 15, 2011
Is a pacemaker the only treatment for bradycardia?
If bradycardia doesn't cause symptoms, it may not be treated. You and your doctor can decide what treatment is right for you. If damage to the heart's electrical system causes your heart to beat too slowly, you will probably need to have a pacemaker.
What is a dangerously low heart rate?
When the heart does not operate as it is supposed to and develops an abnormally slow heart rate that is less than 60 beats per minute, the condition is known as bradycardia. Bradycardia can be life threatening if the heart is unable to maintain a rate that pumps enough oxygen-rich blood throughout the body.
What is the first line treatment for unstable bradycardia?
The American Heart Association recommends atropine sulfate as the first line of treatment for symptomatic bradycardia, regardless of whether it is due to AVB or not.Nov 23, 2019
How does atropine treat bradycardia?
Abstract. The use of atropine in cardiovascular disorders is mainly in the management of patients with bradycardia. Atropine increases the heart rate and improves the atrioventricular conduction by blocking the parasympathetic influences on the heart.
How to diagnose bradycardia?
To diagnose your condition, your doctor will review your symptoms and your medical and family medical history and do a physical examination. Your doctor will also order tests to measure your heart rate, establish a link between a slow heart rate and your symptoms, and identify conditions that might be causing bradycardia.
What causes bradycardia?
Change in medications. A number of medications, including some to treat other heart conditions, can cause bradycardia. Your doctor will check what medications you're taking and possibly recommend alternatives. Changing drugs or lowering dosages might correct problems with a slow heart rate.
What is an EKG?
Electrocardiogram (ECG or EKG) An electrocardiogram, also called an ECG or EKG, is a primary tool for evaluating bradycardia. Using small sensors (electrodes) attached to your chest and arms, it records electrical signals as they travel through your heart. Because an ECG can't record bradycardia unless it happens during the test, ...
Can bradycardia cause slow heart rate?
Treatment for bradycardia depends on the type of electrical conduction problem, the severity of symptoms and the cause of your slow heart rate. If you have no symptoms, treatment might not be necessary.
What is a wireless pacemaker?
The pacemaker monitors your heart rate and generates electrical impulses as necessary to maintain an appropriate rate. A wireless pacemaker has been approved by the FDA. The leadless system holds promise for people who need pacing in only one ventricle, but more study is needed.
How long does a Holter monitor record heart rate?
Holter monitor. Carried in your pocket or worn on a belt or shoulder strap, this device records your heart's activity for 24 to 48 hours. Your doctor will likely ask you to keep a diary during the same 24 hours. You'll describe any symptoms you experience and record the time they occur. Event recorder.
Where is the pacemaker implanted?
Pacemaker. This battery-operated device about the size of a cellphone is implanted under your collarbone. Wires from the device are threaded through veins and into your heart. Electrodes at the end of the wires are attached to heart tissues.
How to tell if you have bradycardia?
You may not have any symptoms of bradycardia. But if you do have a slow heart rate and any of these symptoms, call your doctor: 1 Syncope/passing out 2 Dizziness 3 Weakness 4 Confusion 5 Heart palpitations/fluttering 6 Feeling short of breath 7 Chest pain 8 Lack of energy
Why do you need a heart monitor?
You will keep track of any symptoms you have. Your doctor will match up the symptoms with the activity on the monitor to see if a heart rhythm problem is the cause and if your heart rate is related to your symptoms.
What does it mean when your heart beats slow?
Bradycardia means your heart rate is slow. This can be completely normal and desirable, but sometimes it can be an abnormal heart rhythm (arrhythmia). If you have bradycardia and you have certain symptoms along with the slow heart rate, then it means your heartbeat is too slow.
What is the normal heart rate for a person?
A normal resting heart rate for most people is between 60 and 100 beats per minute (bpm). A resting heart rate slower than 60 bpm is considered bradycardia. Athletic and elderly people often have a heart rate slower than 60 bpm when they are sitting or lying down, and a heart rate less than 60 bpm is common for many people during sleep.
What is the heart's electrical system?
To understand bradycardia, it helps to understand the heart’s electrical system, which is what makes the heart beat. Your heart has a natural pacemaker called the sinus node (SA node), which is made of a small bunch of special cells.
What is the purpose of a pacemaker?
A pacemakers is a small device that is placed under your skin to monitor your heart’s rate and rhythm.
Where is the AV node?
Next, the impulse travels down an electrical pathway to the AV node. The AV node is in the center of your heart, in between the atria and ventricles. The AV node acts like a gate that slows the electrical signal before it moves into the ventricles.
Answer
Bradycardia is a slower than normal heart rate. The average heartbeat of an adult at rest is usually between 60 and 100 times a minute. If one has their heart beats fewer than 60 times a minute. bradycardia is not considered a health problem but in cases of Hypotension bradycardia requires treatment
New questions in Social Studies
3 Type the correct answer in the box. Spell all words correctly. What are the three ways through which a company tries to sell its products? Businesse …
What are the symptoms of bradycardia?
5. Common bradycardia symptoms include: syncope. presyncope. transient dizziness or lightheadedness. fatigue. dyspnea on exertion. heart failure symptoms.
What is bradycardia heart rate?
What is bradycardia? The National Institutes of Health defines bradycardia* as a heart rate <60 bpm in adults other than well-trained athletes. 9 The determination on whether or not treatment is necessary for bradycardic events is generally based on the presence of bradycardia symptoms. The clinical manifestations of bradycardia can vary widely from insidious symptoms to episodes of frank syncope. 5
When a patient is evaluated for symptomatic bradycardia, an in-depth history and physical is
When a patient is evaluated for symptomatic bradycardia, an in-depth history and physical is important, along with the identification of possible reversible causes. The following is a list of conditions associated with bradycardia and conduction disorders: 11
What percentage of patients with sleep apnea have sinus bradycardia?
The prevalence of sinus bradycardia in patients with sleep apnea can be as high as 40%, with episodes of second- or third-degree AV block in up to 13% of patients. 8
How much atropine is given?
Atropine 0.5 mg intravenous (IV) is given up to a total of 3 mg. 1 Atropine sulfate acts by reversing the cholinergic-mediated decreases in the heart rate and AV node conduction. 1. If atropine is ineffective, two treatment pathways are available.
Can exercise be used for ischemia?
Although not routinely recommended for assessment of ischemia, exercise testing can be considered in patients with symptoms temporally related to exercise, asymptomatic second-degree AV block, or for suspected chronotropic incompetence. 11
