- Collaborative Goal Setting. ...
- Accountability. ...
- Nutrition Consultation and Meal Planning. ...
- Self-monitoring Food Intake, Weight, and Activity. ...
- Stimulus Control. ...
- Problem Solving. ...
- Problem Solving: Troubleshooting Specific Eating Situations. ...
- Relapse Prevention.
What are the behavioral goals in treating obesity?
Behavioral treatment usually includes multiple components, such as keeping food and activity records (ie, self-monitoring), controlling cues associated with eating (ie, stimulus control), nutrition education, slowing eating, physical activity, problem solving, and cognitive restructuring (ie, cognitive therapy) (5,6).
Which is an example of a behavior modification technique for weight loss?
Of the following, which is an example of a behavior modification technique for weight loss? Download an app to keep a record of your eating and exercise habits. A persons is considered underweight until his BMI reaches _____.
What are the behavior modification techniques?
TechniquesPositive reinforcement.Negative reinforcement.Punishment.Flooding.Systematic desensitization.Aversion therapy.Extinction.
What are behavioral factors of obesity?
A number of behavioural risk factors has been postulated, including diets with a high energy density, high consumption of sugar-sweetened beverages, large portion sizes, eating patterns, high levels of sedentary behaviour and low levels of physical activity.
What are the behavior modification techniques to reduce obesity?
Behavioral Modification for Obesity ManagementCollaborative Goal Setting. ... Accountability. ... Nutrition Consultation and Meal Planning. ... Self-monitoring Food Intake, Weight, and Activity. ... Stimulus Control. ... Problem Solving. ... Problem Solving: Troubleshooting Specific Eating Situations. ... Relapse Prevention.
What are behavioral weight loss programs?
To help patients meet their dietary and physical activity goals, behavioral weight loss interventions teach a range of behavioral skills that facilitate behavior change (24, 38). One core skill is self-monitoring (e.g., tracking or logging) weight, food intake, and physical activity steps or minutes.
What are some examples of behavior modification?
Examples of behavior modification which can be used to increase behavior are: praise and approval, modeling, positive programming, shaping, token economy, self-monitoring, and shaping.
What is Behaviour modification?
Behavior modification is defined as "the alteration of behavioral patterns through the use of such learning techniques as biofeedback and positive or negative reinforcement." More simply, you can modify your child's behavior with positive consequences and negative consequences.
What is behavioral modification therapy?
Behavior modification therapy is a behavior-focused therapy, helping you add or extinguish behaviors to have the outcomes you desire. Ultimately, Choices wants to help you live a happy, healthy life. This could be your best solution to doing just that.
What are behavioral risk factors?
any specific behavior or pattern of behaviors (e.g., overeating or smoking) that increases an individual's likelihood of developing a disorder, disease, or syndrome.
How is obesity associated with behavioral stress?
It has long been theorized that an association exists between long-term stress and obesity. Chronic stress can lead to “comfort eating,” which often involves the overeating of foods that are high in fat, sugar, and calories, which, in turn, can lead to weight gain.
What are 3 main causes of obesity?
Calories. The energy value of food is measured in units called calories. ... Poor diet. Obesity does not happen overnight. ... Lack of physical activity. Lack of physical activity is another important factor related to obesity. ... Genetics. ... Medical reasons.
Understanding Health and Nutrition
Most people do not spend time thinking about the complex systems that make up our bodies. We may not take the time to think about how the food we eat and the physical activity we do can either help or harm our body depending on our choices. Learning more about your body and how to properly nourish it are essential for improved health and weight.
Self-monitoring
Losing weight is not necessarily as simple as eating less and moving more. There is also no one-size-fits-all approach to weight-loss. Self-monitoring is an easy and effective way to keep track of what food and beverages you consume, how much you exercise and more.
Physical Activity
Before you begin any new physical activity plan, be sure to check with your healthcare provider. Physical activity is a key part of any health and wellness plan. Combining physical activity with healthier eating is an important step in beginning to reach and/or maintain your goals.
Support Groups
The journey of improving your health and weight can sometimes feel like a difficult and lonely one. Finding the right weight-loss plan can take time and be mixed with setbacks.
Conclusion
Your everyday choices are your behaviors. They include everything from how much sleep you get each night to what you have for lunch and if you take the stairs or the elevator. Your behaviors join together to form your lifestyle. Making lifestyle modifications is key for managing your health.
What is health behavior change?
Health behavior change is central in obesity management. Due to its complexity, there has been a growing body of research on: i) the factors that predict the adoption and maintenance of health behaviors, ii) the development and testing of theories that conceptualize relationships among these factors and with health behaviors, ...
How do theories help with behavior change?
Theories (‘systematic way of understanding events or situations, (…) a set of concepts, definitions, and propositions that explain or predict these events or situations by illustrating the relationships between variables’ [8], p. 4) are useful to understand, explain, and predict behavior and behavior change, as they conceptualize a set of interrelated constructs operating as predictors or mechanisms of action underlying behavior change. There are various levels of constructs that influence health behavior; they are therefore conceptualized in health behavior change theories. These can be done at the environmental level whether it is physical, cultural, or social (e.g., advice from a healthcare practitioner, low accessibility, peer support) or at the individual level including biological factors (e.g., food reward mechanisms) but also emotions, motivation, and self-regulation skills. Individual factors are considered fundamental for health behavior change as they are mostly responsible for the process of self-regulation of health behaviors. For instance, a systematic review looking at psychological mediators of sustained beneficial effects in lifestyle obesity interventions [9] found that higher levels of autonomous motivation, self-efficacy/barriers, self-regulation skills, flexible eating restraint, and positive body image were mediators of medium-/long-term weight control. High autonomous motivation, self-efficacy, and use of self-regulation skills were significant mediators of physical activity while for dietary intake no consistent mediators were identified.
Why are techniques useful in HBCIs?
Techniques are useful in HBCIs to the extent that they impact on the putative mechanisms of action (e.g. goal setting) to change a given behavior (e.g. physical activity). Currently, there are efforts begin made in linking clusters of BCTs to specific mechanisms of action and overarching behavioral theories [42].
How many theories are there for HBCI?
Recently, a panel of experts has identified and compiled 83 formal theories of behavior and behavior change (including more than 1,700 theoretical constructs) in a comprehensive compendium [16]. Faced with so many theories from which to select from, researchers and practitioners need the skills to make decisions regarding the best candidate theory for a given behavior and context. This can be particularly difficult when targeting multiple behaviors (e.g., physical activity and diet), which is the case when considering weight management interventions. To guide this process, efforts have been made to make frameworks for the development of HBCIs informed by theory. This includes the Intervention Mapping Protocol [17] or the Theoretical Domains Framework [18]. In addition, tools such as the Theory Coding Scheme allow for an evaluation of the extension of use of theory in a HBCI [19]. The overarching COM-B model [6], which contains three broad theory-related dimensions of behavior change determinants – competence, motivation, and opportunity -, can also be used to make decisions on the design of HBCIs, especially when this is conducted without input by health psychologists or behavior change specialists.
How long does it take to maintain weight loss?
While behavioral interventions seem to be effective in promoting weight loss, weight loss maintenance is a key challenge as most adults that successfully lose weight tend to regain part of it within 1 year [20]. Currently, there are very few comprehensive treatments available, and indeed most of the research has focused on the behavioral aspects associated with weight loss [21,22]. A recent systematic review on theoretical explanations for behavior change maintenance [22] identified five interconnected theoretical explanations about how individuals maintain initial behavior changes over time: i) maintenance motives – tendency to maintain behavior when there are sustained motives (e.g. enjoyment) and congruence between behavior and identity/values (e.g. self-determination theory [23]); ii) self-regulation – includes self-monitoring and coping strategies (self-regulation theory [24]); iii) physical and psychological resources (e.g. self-control theory [25]), iv) habit – habitual behaviors supported by automatic responses to cues (e.g. habit theory [26]); and v) environmental and social cues – supportive environment, social support, behavior in line with social changes (e.g. normalization process theory [27]). At present, in long-term weight management there is some support for the effectiveness of HBCIs which are based on self-determination theory (e.g. [9,28,29]) and self-regulation theories (e.g. [9,30,31]).
How can HBCIs be optimized?
Recently, a broad consensus emerged indicating that HBCIs can be optimized if they are informed by theory [10], as it facilitates the understanding of what works to change a certain behavior and how it works [11]. Theories of behavior change propose the mechanisms of action (under the broad categories of capacity, opportunity, and motivation) and the moderators of change through causal predictions. While there is an agreement in health behavior change that the use of theory is useful to promote long-lasting behavior change, there is still limited research on the effectiveness of theory-based (vs. non-theory-based) interventions. For instance, a recent meta-analysis by Gourlan and colleagues [12] investigated the effects of 82 theory-based randomized controlled trials targeting physical activity and showed beneficial but small effects of theory-based interventions in changing physical activity (d = 0.31). Similar results were found in a meta-analysis of digital-based interventions targeting various health behaviors (85 studies), in which the extensive use of theory (e.g., use theoretical constructs to develop intervention techniques) was associated with larger intervention effects [13]. Another meta-analysis examining the influence of theory use in physical activity and dietary interventions, did not find significant associations (e.g. [14]). There are several reasons that may explain these results: i) limited number of theories commonly tested (e.g., Social Cognitive Theory, Theory of Planned Behavior), ii) the fact that some theories may not provide a clear explanation on the process of behavior change maintenance, and iii) when interventions are explicitly based on theory, they often do not apply it extensively [12,14]. Furthermore, research findings suggest that single-theory approaches may be more effective in influencing behaviors such as physical activity, comparing with those interventions applying multiple theories [12,13]. This finding may be related to the fact that some interventions consist of a combination of two or more theories (or key constructs from these theories) lacking internal coherence and parsimony [15].
What are the active ingredients of interventions?
The Active Ingredients of Interventions: Behavior Change Techniques. A key aspect in the development, implementation and evaluation of HBCIs is the adequate characterization of its content – the ‘active ingredients’, i.e., the techniques used in interventions to help change another's or one's own behavior.
How does behavior modification affect weight loss?
The introduction of behavior modification in the treatment of obesity a decade ago resulted in a substantial increase in weight loss of persons treated for mild to moderate obesity. It has been hoped that this increased effectiveness of treatment would extend also to maintenance of weight loss, and the first controlled clinical trial suggested that it did. This article reports the results of (1) a five-year follow-up of this first trial and (2) all follow-up studies of behavior modification for obesity yet conducted, six published and four previously unpublished. A new method of data analysis shows that weight losses are only modestly maintained, although the question of how their maintenance compares with that of other treatments cannot be answered because comparable data on other treatments are not available. In contrast to the vast amount of work on the initiation and generalization of behavior change, study of its maintenance has been a neglected area of behavior modification. We suggest that this area constitutes a new frontier for research in behavior modification.
Is weight loss maintained?
A new method of data analysis shows that weight losses are only modestly maintained, although the question of how their maintenance compares with that of other treatments cannot be answered because comparable data on other treatments are not available.
How does behavioral change affect obesity?
If the total energy consumed exceeds the energy received, the negative energy balances weight loss. The main goal of behavioral treatment in obesity is to reduce eating and increase activity. According to behavior theory, eating behavior strengthens due to the tastes of foods. In summary, the person ignores the negative consequences of overeating in long term over the taste and smell of the short-term pleasure.
How does cognitive behavioral therapy help with obesity?
In the treatment of obesity, combining the changes in lifestyle such as diet and increasing physical activity with cognitive-behavioral interventions increases the efficacy of the treatment and ensures the sustained weight gain.
What is cognitive behavioral therapy?
Cognitive behavioral therapy of obesity includes: self-monitoring, stimulus control, eating control, reinforcement and empowerment, cognitive restructuring, proper nutrition education, increasing physical activity and behavioral contract. In the treatment of obesity, combining the changes in lifestyle such as diet and increasing physical activity ...
What is the relationship between the biological basis of obesity and behaviors?
If the total energy consumed exceeds the energy received, the negative energy balances weight loss.The main goal of behavioral treatment in obesity is to reduce eating and increase activity.
How long does it take to treat obesity?
Behavioral treatment for obesity is usually administered for 12-20 weeks in 1-2 hours sessions per week with groups of 10-12 people under the direction of a therapist. The steps of behavioral treatment are; Self-monitorization. Stimulus control. Control of eating behavior.
What are the principles of behavior change?
This. principles are ; human expectations about the consequences of their behavior, and behavior change in response to environmental requirements. They are based on a large number of studies. The aim is to replace the unwanted behavior with the healthy ones.
Is obesity a public health problem?
Obesity is a public health problem that concerns all segments of the society today, has serious negative effects on mortality and morbidity rates and is one of the most important health problems of developed and developing countries.
How does behavioral change affect weight loss?
Changing behavior is critical to weight loss success. Com-prehensive behavioral interventions that help patients change their eating and exercise behaviors produce weight losses of 5–10% of body weight and clinically significant improvements in health. Such behavioral approaches are important as a stand-alone approach to weight loss as well as a key component of pharmacologic therapy or surgical approaches to weight control.
What is behavioral intervention?
Behavioral (or lifestyle) interventions are considered the cor-nerstone of obesity treatment. These programs are designed to produce long-term weight losses through changes in diet and physical activity. Behavioral approaches form the basis for the prevention and treatment of obesity in both chil-dren and adults. In addition, they are critical components of pharmacological and surgical approaches to obesity.
How long are behavioral programs?
Behavioral programs are typically offered in a closed group format, with approximately 15–20 patients treated together in weekly sessions ranging from 16–24 weeks. Following the chronic disease model, continuation of contact is important but is gradually reduced to bi-weekly and monthly check-ins. Although longer programs have been shown to increase weight loss and delay weight regain, these time-intensive programs have been criticized as too costly and burdensome to translate and deliver outside of research settings. Recent studies have shown that phone contact can be used success-fully in lieu of face-to-face contact. Likewise, providing the intervention via Internet or mobile devices can allow for more cost-effective dissemination of these programs.3
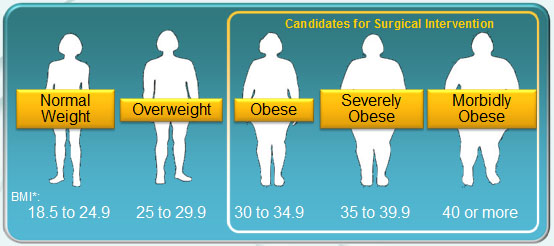
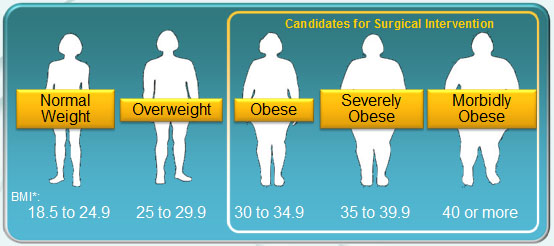
Is bariatric surgery a cure for obesity?
Bariatric surgery is described in detail in another article in this issue (Diabetes, obesity, and other medical diseases – is surgery the answer? – Dieter Pohl, MD, FACS, FASMBS; Aaron Bloomenthal, MD, FACS). While bariatric surgical procedures generally produce weight losses that are far supe-rior and more durable than behavioral or pharmacological weight loss treatments, most patients begin to experience weight regain as early as after the initial postoperative year. Importantly, bariatric surgery is not an obesity cure, but another tool patients may use in combination with behav-ioral changes to achieve weight loss and related health improvements. To be most successful after bariatric sur-gery, patients must make multiple behavior changes such as consuming small meals/snacks (≤ 8 oz), ≥ 5 meals/snacks each day, eating slowly, stopping at satiation, and avoiding alcohol and concentrated sweets/snacks.18 Although surgi-cal outcomes are enhanced when combined with changes in diet, activity, and other weight-related (e.g., self-weigh-ing) behaviors, development and testing of behavioral interventions for bariatric surgery patients has received limited attention. Our group recently tested a behavioral intervention to increase moderate-intensity walking before bariatric surgery, as prior studies have shown that higher physical activity levels before surgery are related to greater physical activity levels and weight loss after surgery. Our intervention employed standard behavioral strategies (e.g., self-monitoring, goal-setting) to help patients increase theirphysical activity in bouts ≥ 10 minutes. Patients in the intervention group increased objectively-monitored moder-ate to vigorous physical activity in bouts ≥ 10 minutes by nearly 5-fold (from 4.4 to 21.0 min/d) where patients ran-domly assigned to standard care did not change (from 7.9 to 7.6 min/d). Additionally, in those patients who went on to have bariatric surgery, those who had received the inter-vention maintained higher physical activity levels through
Understanding Health and Nutrition
- Most people do not spend time thinking about the complex systems that make up our bodies. We may not take the time to think about how the food we eat and the physical activity we do can either help or harm our body depending on our choices. Learning more about your body and how to properly nourish it are essential for improved health and weight. There are a variety of ways t…
Self-Monitoring
- Losing weight is not necessarily as simple as eating less and moving more. There is also no one-size-fits-all approach to weight-loss. Self-monitoring is an easy and effective way to keep track of what food and beverages you consume, how much you exercise and more. Your goal in monitoring your lifestyle should be to increase self-awareness of your choices and make modifi…
Physical Activity
- Before you begin any new physical activity plan, be sure to check with your healthcare provider. Physical activity is a key part of any health and wellness plan. Combining physical activity with healthier eating is an important step in beginning to reach and/or maintain your goals. Increasing your physical activity will help you feel better and give you more energy. Physical activity can no…
Support Groups
- The journey of improving your health and weight can sometimes feel like a difficult and lonely one. Finding the right weight-loss plan can take time and be mixed with setbacks. However, you are not alone. Support groups are a wonderful resource for you and others to share and learn with each other. Support groups can be women-only, men-only, faith-based, offered by your local communi…
Conclusion
- Your everyday choices are your behaviors. They include everything from how much sleep you get each night to what you have for lunch and if you take the stairs or the elevator. Your behaviors join together to form your lifestyle. Making lifestyle modifications is key for managing your health. Finding modifications that work and are ones you can keep...