Treatment for cardiac arrest includes immediate cardiopulmonary resuscitation (CPR) and, if a shockable rhythm is present, defibrillation. Among those who survive, targeted temperature management may improve outcomes. An implantable cardiac defibrillator may be placed to reduce the chance of death from recurrence.
Full Answer
What are the treatment options for cardiac arrest?
Treatment 1 CPR. Immediate CPR is crucial for treating sudden cardiac arrest. ... 2 Defibrillation. Advanced care for ventricular fibrillation, a type of arrhythmia that can cause sudden cardiac arrest, generally includes delivery of an electrical shock through the chest wall to the heart. 3 At the emergency room. ... 4 Long-term treatment. ...
What type of care is needed for post–cardiac arrest patients?
A comprehensive, structured, multidisciplinary system of care should be implemented in a consistent manner for the treatment of post–cardiac arrest patients (Class I, LOE B).
What do you need to know about cardiac arrest?
Cardiac Arrest 1 Overview. Cardiac arrest is a serious heart condition. 2 A number of factors can cause sudden cardiac arrest. 3 Certain heart conditions and health factors can increase your... 4 Recognizing the Signs and Symptoms of Cardiac Arrest. 5 Diagnosing Cardiac Arrest. During a cardiac event...
What type of cardiac monitoring should be initiated after cardiac arrest?
Continuous cardiac monitoring, pulse oximetry, capnography and NIBP (non-invasive blood pressure) monitoring should be initiated. This provides critical information on tissue oxygenation and perfusion and helps guide further resuscitative care.

What is the best treatment for cardiac arrest?
CPR. Immediate CPR is crucial for treating sudden cardiac arrest. By maintaining a flow of oxygen-rich blood to the body's vital organs, CPR can provide a vital link until more-advanced emergency care is available. If you don't know CPR and someone collapses unconscious near you, call 911 or emergency medical help.
What is the single most important therapy for survival of cardiac arrest?
CPR is key to survival of sudden cardiac arrest.
What do you give a patient with cardiac arrest?
How is a cardiac arrest treated? Starting immediate CPR is vital as it keeps blood and oxygen circulating to the brain and around the body. A defibrillator will then deliver a controlled electric shock to try and get the heart beating normally again.
Does defibrillation prevent cardiac arrest?
Defibrillation is the only therapy to treat someone in cardiac arrest. Every minute that a person in Sudden Cardiac Arrest does not receive defibrillation, their chances of survival drop by 7-10%, making rapid defibrillation imperative for survival and one of the key steps in saving a life from Sudden Cardiac Arrest.
Does CPR help cardiac arrest?
CPR Saves Lives. Currently, about 9 in 10 people who have cardiac arrest outside the hospital die. But CPR can help improve those odds. If it is performed in the first few minutes of cardiac arrest, CPR can double or triple a person's chance of survival.
What is the first treatment for cardiac arrest?
The sequence of CPR begins with 30 chest compressions, followed by 2 rescue breaths, and continues in a ratio of 30:2 until the rescuer is relieved by emergency personnel. Chest compressions can quickly tire a person, resulting in compressions that are too weak to circulate blood effectively.
What are the two first line drugs and doses used in cardiac arrest?
Epinephrine (adrenaline) has been the preferred vasopressor used for resuscitating cardiac arrest patients for several decades; however, vasopressin, an antidiuretic hormone, has been evaluated and recommended as an alternative in recent years.
How do you do CPR for cardiac arrest?
Start hands-only chest compressions:Put one hand over the other, and place both on the person's breastbone, in the middle of his or her chest.Press hard enough to make the chest move inward about an inch.Relax, and repeat. Do this about 100 times a minute.
What is the treatment for cardiac arrest?
Treatments might include: Drugs. Doctors use various anti-arrhythmic drugs for emergency or long-term treatment of arrhythmias or potential arrhythmia complications.
What is the best medication for sudden cardiac arrest?
A class of medications called beta blockers is commonly used in people at risk of sudden cardiac arrest. Other possible drugs that can be used to treat the condition that led to the arrhythmia include angiotensin-converting enzyme (ACE) inhibitors and calcium channel blockers. Implantable cardioverter-defibrillator (ICD).
What is the best way to help someone who is at risk of cardiac arrest?
The American Red Cross and other organizations offer courses in CPR and defibrillator use. Being trained will help not only your loved one, but your training might help others.
What is the importance of CPR?
Immediate CPR is crucial for treating sudden cardiac arrest. By maintaining a flow of oxygen-rich blood to the body's vital organs, CPR can provide a vital link until more-advanced emergency care is available. If you don't know CPR and someone collapses unconscious near you, call 911 or emergency medical help.
What is the procedure called when you have ventricular fibrillation?
The procedure, called defibrillation, momentarily stops the heart and the chaotic rhythm.
What to do if you survive sudden cardiac arrest?
If you survive sudden cardiac arrest, your doctor will try to learn what caused it to help prevent future episodes. Tests your doctor may recommend include:
What is the ejection fraction of a heart?
Ejection fraction refers to the percentage of blood that's pumped out of a filled ventricle with each heartbeat. A normal ejection fraction is 50% to 70%. An ejection fraction of less than 40% increases your risk of sudden cardiac arrest. Nuclear scan.
What is the best treatment for cardiac arrest?
Cardiopulmonary resuscitation (CPR) is one form of emergency treatment for cardiac arrest. Defibrillation is another. These treatments get your heart beating again once it has stopped. If you survive a cardiac arrest, your doctor may start you on one or more treatments to reduce the risk of another attack.
What is cardiac arrest?
Overview. Cardiac arrest is a serious heart condition. The word arrest means to stop or bring to a halt. In cardiac arrest, the heart ceases to beat. It’s also known as sudden cardiac death. Your heartbeat is controlled by electrical impulses. When these impulses change pattern, the heartbeat becomes irregular. This is also known as an arrhythmia.
What are the causes of sudden cardiac arrest?
A number of factors can cause sudden cardiac arrest. Two of the most common are ventricular and atrial fibrillation.
What happens when the heart stops pumping blood?
In some cases, the circulation of blood stops completely. This may lead to sudden cardiac death.
What are the risk factors for cardiac arrest?
Other risk factors for cardiac arrest include: smoking. sedentary lifestyle. high blood pressure. obesity. family history of heart disease. history of a previous heart attack. age over 45 for men, or over 55 for women.
What is the name of the chambers of the heart that stop beating?
The heart can also stop beating efficiently after an arrhythmia in the upper chambers. These chambers are known as the atria.
What happens if your heart is too big?
Having an abnormally large heart places you at increased risk for cardiac arrest. A large heart may not beat correctly. The muscle may also be more prone to damage.
What is cardiac arrest?
Cardiac arrest (CA) is often the terminal event following progression of and decompensation from a wide range of pathophysiological events. With medical advances and improvements in the delivery of prehospital care, we are witnessing increasing rates of return of spontaneous circulation (ROSC) following CA. Once resuscitated, the next challenge is to manage these patients appropriately so as to not only prevent mortality but preserve neurological and cognitive function. Proper post-resuscitation care (PRC) has been shown to reduce mortality and morbidity.1–3To achieve this, a closely coordinated multidisciplinary team effort is required. The key steps involved in caring for these patients include:
What is the most common cause of cardiac arrest?
Coronary artery occlusion remains a leading cause of out-of-hospital cardiac arrest (OHCA).24,25An initial 12-lead ECG should be obtained in all patients post-arrest.8If STEMI is noted, reperfusion therapy should be strongly considered: either via primary percutaneous coronary intervention (PCI) or intravenous fibrinolytic therapy as both have been shown to be efficacious.26Traumatic or prolonged CPR (>10 min) is a relative contraindication to fibrinolytic use27and the risk and benefits of fibrinolysis should be considered in this sub-group. PCI can be safely performed in patients undergoing TH28but the safety of fibrinolytic therapy for STEMI in conjunction with TH is less well established. Preliminary studies suggest that the risk of stent thrombosis is no different in patients treated with or without TH.29Consideration may be given to performing angiography (and possible PCI) in all patients following ROSC who do not have an alternate explanation of arrest irrespective of the ECG findings30,31but the benefit of routinely implementing this approach remains controversial and it has been challenging to identify patients who would benefit most from invasive assessment and treatment. Future research should be directed towards developing modalities identifying these patients appropriately. Body surface potential mapping as mentioned previously is one such modality.15
What is the cause of death after resuscitation?
Neurological injury is a major cause of death following successful resuscitation.32Post-resuscitation TH has been demonstrated to improve neurological outcomes in comatose patients whose initial recorded rhythm was VF.10,11Harmful pathways that accompany reperfusion injury seem to be inhibited by hypothermia and exacerbated by hyperthermia. According to the 2010 AHA guidelines,8all comatose patients with ROSC after out of hospital VF arrest should be cooled to 32 °C–34 °C for 12–24 h. TH should be considered for comatose patients with ROSC after in-hospital CA from any rhythm or OHCA from PEA or Asystole. Active rewarming is contraindicated in patients who develop spontaneous hypothermia (temperature >32 °C) after ROSC post-CA within the first 48 h.
What is a 12 lead ECG?
A 12-lead ECGshould be analyzed in all patients with CA for presence of ST-segment deviation, T-wave abnormalities, dysrhythmias, conduction defects, QT-interval and presence of low voltage (which may indicate tamponade).8An initial as well as repeat 12-lead ECG's are critical for early recognition of ongoing myocardial ischemia and presence of arrhythmias that require treatment. A 64-lead continuous ST mapping obtained using a chest vest may enhance sensitivity and specificity compared to a standard 12-lead ECG for detecting underlying coronary artery occlusion,15however, additional studies are warranted prior to recommending routine implementation of this strategy.
How much should PaCO2 be maintained?
This impedes preload and decreases cardiac output which can be deleterious in hypotensive patients. Generally, PaCO2should be maintained around 40–45 mm of Hg and, if monitored, end-tidal CO2(capnometry) level should be kept between 35–40 mm of Hg.8
Which treatment should be considered when considering fibrinolysis and thrombectomy?
Anticoagulation, consideration should be given to fibrinolysis and thrombectomy.
Can you monitor a patient without intubation?
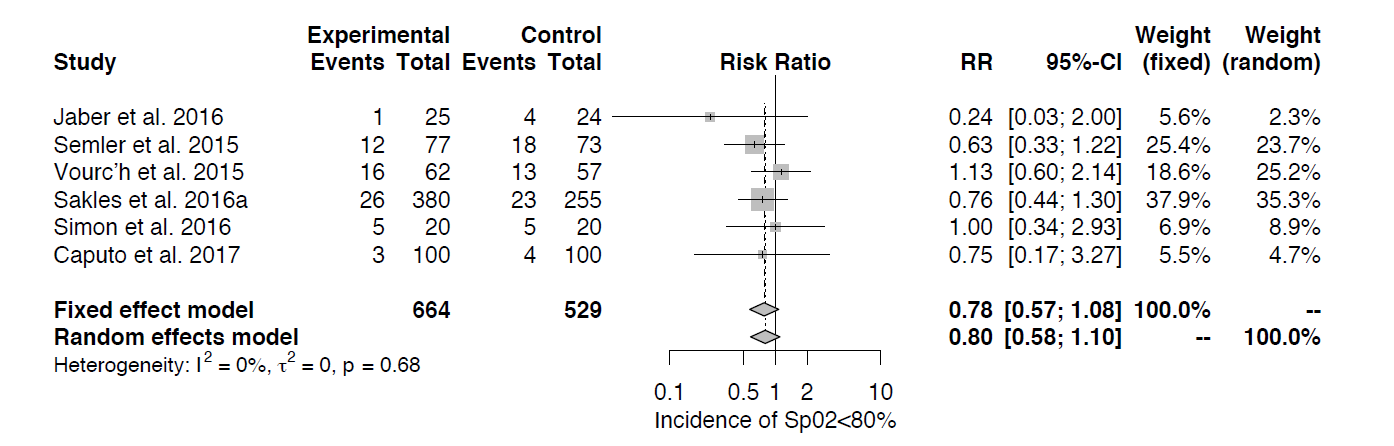
Awake patients with appropriate respiratory effort and able to maintain their airway can be monitored without intubation. Controlled use of supplemental oxygen to achieve SpO2≥94% is recommended in the non-intubated patients post-resuscitation. Similarly, in patients who are intubated FIO2should be quickly titrated to maintain SpO2≥94%. Higher PaO2levels may lead to adverse neurological outcomes secondary to generation of free radicals and brain lipid peroxidation in the context of global ischemia followed by reperfusion.8,19
What percentage of cardiac arrest patients survive?
Overall outcomes from out-of-hospital cardiac arrest (OHCA), both in terms of survival and neurologic and functional ability, are poor: only 11 percent of patients treated by emergency medical services (EMS) personnel survive to discharge (Daya et al., 2015; Vellano et al., 2015). Although a few EMS systems have demonstrated the ability to significantly increase survival rates (Nichol et al., 2008; Sasson et al., 2010b), a fivefold difference in survival-to-discharge rates exists among communities in the United States (Nichol et al., 2008). This presents important challenges and opportunities to improve EMS system performance across the country.
What is the response interval for cardiac arrest?
Response intervals include the time required to receive and process the initial 911 call, notify closest EMS responders, and for responders to arrive on scene with a defibrillator. These intervals vary considerably among EMS systems because of differences in geography, traffic, population density, and distribution of EMS units. Survival decreases by approximately 7 to 10 percent for every minute after witnessed cardiac arrest that passes without administration of CPR (Larsen et al., 1993). In the majority of OHCA cases where bystander CPR is not provided, cardiac arrest survival is extremely low. As discussed in Chapter 3, bystander CPR is especially important in areas where response times are often delayed.
How does EMS affect cardiac arrest?
EMS response intervals are strongly associated with cardiac arrest survival rates, with longer response intervals linked to worse outcomes (Stiell et al., 1999). Studies indicate that the likelihood of survival with favorable neurologic outcome following a cardiac arrest increases the sooner that treatment begins, and the effect of any BLS treatment is minimal if a patient has not achieved ROSC within 10 minutes of collapse (Weisfeldt and Becker, 2002). See Chapter 6for research into novel therapies that may extend the window of effective treatment. Given the numerous variables and actors between recognition of an emergency and defibrillation or provision of CPR, there are many points at which delays might occur. For example, delays could occur if a call center was not able to track the location of a cell phone and could not immediately dispatch EMS personnel to the scene. Delays may also occur in collecting information from bystanders, routing calls between PSAPs and dispatchers, assessing a patient's medical condition, locating available nearby EMS responders, or in transitions between individuals performing BLS or ACLS and the transfer of care to hospital staff.
What are the five main chains of survival?
As described in Chapter 1, the chain of survival includes five interconnected links: (1) immediate recognition of cardiac arrest and activation of the emergency response system , (2) early cardiopulmonary resuscitation (CPR), (3) rapid defibrillation, (4) effective advanced cardiac life support (ACLS), and (5) integrated post-resuscitative care (M. D. Berg et al., 2010; R. A. Berg et al., 2010). This conceptual model illustrates the sequence of events that can optimize care and outcomes for the approximately 395,000 individuals who experience an OHCA in the United States each year (Daya et al., 2015). Together, the first three steps comprise the fundamental actions within basic life support (BLS) strategies for cardiac arrest (R. A. Berg et al., 2010), including early recognition of a cardiac arrest by bystanders1and 911 call takers, as well as the delivery of initial treatments (i.e., CPR and defibrillation) by bystanders or trained first responders prior to the arrive of EMS providers (i.e., emergency medical technicians [EMTs] and paramedics).
What is an EMS system?
For purposes of this report, the committee defines an EMS system as a system that provides emergency medical care in response to serious illness or injury , such as a cardiac arrest, in the prehospital setting. An EMS system comprises a wide range of responders who provide critical services, such as response to 911 emergency calls, dispatch of medical personnel, triage, treatment, and rapid transport of patients by ground or air ambulances to appropriate care facilities (IOM, 2007). Emergency medical response and care involves different types of people and agencies, including those in the public health, public safety, and health care sectors (see Table 4-1). As such, multiple regulatory and administrative bodies at local, state, and federal levels regulate different aspects of emergency medical care, leading to different resource and funding streams available for implementation and evaluation activities.
How does transport distance affect EMS response times?
The negative effects of transport distance and population density on EMS response times and patient outcomes can be mitigated by the use of computer-aided dispatching and coordination among ambulance crews. For example, a study of the Singapore EMS system found that by moving ambulances to locations where, and staffing them at times when, OHCAs were more likely to occur, response times decreased significantly from a monthly median of 10.1 minutes to 7.1 minutes (Ong et al., 2010). Importantly, this improvement was achieved without the addition of new ambulances, personnel, or total working hours (Ong et al., 2010). Similar efforts to decrease response times by predicting cardiac events and efficiently deploying ambulances have been successful in the United States and elsewhere (Gonzalez et al., 2009; Jermyn, 2000; Peleg and Pliskin, 2004). Response times may also be reduced by expanding access to the emergency response system. The Next Generation 911 (NG911) program seeks to enable 911 callers anywhere in the United States to connect to PSAPs via wireless and Voice over Internet Protocol (VoIP) communication devices, to locate these callers, and to allow 911 dispatchers to freely exchange call data among PSAPs (DOT, 2015). Given the increasing prevalence of smartphones in the United States, the ability to text 911 in an emergency holds promise for expanding access to 911. In 2014, the FCC adopted an order requiring all wireless carriers to develop the capability to send text messages to 911 and to deliver emergency texts to PSAPs upon request (FCC, 2015c). As a result, PSAPs began to prepare to receive emergency text messages from wireless providers; as of March 2015, more than 200 PSAPs were capable of doing so (FCC, 2015a). However, much progress remains to be made, because only 21 percent of NG911 systems are fully operational, and more than half have zero functionality (NHTSA, 2015b, p. 3).
What is the role of EMS in cardiac arrest?
This chapter focuses on the EMS system's response to cardiac arrest and covers the EMS role across all of the links in the chain-of-survival model. Because the overall structure, organization of services, and capabilities of EMS systems affect cardiac arrest care, the chapter begins with an overview of the EMS system, including discussion of the relevant personnel and oversight at the federal, state, and local levels. The second section covers elements of the EMS response itself, including the facilitation of bystander CPR and early defibrillation strategies. The final section of the chapter focuses on opportunities to improve the timeliness and quality of cardiac arrest care, which can lead to improved patient outcomes in communities across the United States.
What antiarrhythmics are used for cardiac arrest?
Patients with cardiac arrest may receive antiarrhythmic drugs such as lidocaine or amiodarone during initial resuscitation. There is no evidence to support or refute continued or prophylactic administration of these medications. 7, 148 – 152
What is the most common cause of cardiac arrest?
ACS is a common cause of cardiac arrest. 14, 16, 34, 35, 134 – 147 The clinician should evaluate the patient's 12-lead ECG and cardiac markers after ROSC. A 12-lead ECG should be obtained as soon as possible after ROSC to determine whether acute ST elevation is present (Class I, LOE B). Because it is impossible to determine the final neurological status of comatose patients in the first hours after ROSC, aggressive treatment of ST-elevation myocardial infarction (STEMI) should begin as in non–cardiac arrest patients, regardless of coma or induced hypothermia. Because of the high incidence of acute coronary ischemia, consideration of emergent coronary angiography may be reasonable even in the absence of STEMI. 14, 16 Notably, PCI, alone or as part of a bundle of care, is associated with improved myocardial function 14 and neurological outcomes. 11, 16 Therapeutic hypothermia can be safely combined with primary PCI after cardiac arrest caused by AMI. 11, 31, 33 – 35 Other details of ACS treatment are discussed in Part 10.
How long after a comatose cardiac arrest can you have a physical examination?
A thorough neurological evaluation is needed to obtain accurate prognostic findings. No postarrest physical examination finding or diagnostic study has as yet predicted poor outcome of comatose cardiac arrest survivors during the first 24 hours after ROSC. After 24 hours somatosensory evoked potentials (SSEPs) and select physical examination findings at specific time points after ROSC in the absence of confounders (such as hypotension, seizures, sedatives, or neuromuscular blockers) are the most reliable early predictors of poor outcome in patients not undergoing therapeutic hypothermia. However, the decision to limit care should never be made on the basis of a single prognostic parameter, and expert consultation may be needed.
What is ROSC in cardiac arrest?
Correction. There is increasing recognition that systematic post–cardiac arrest care after return of spontaneous circulation (ROSC) can improve the likelihood of patient survival with good quality of life.
What should be monitored during resuscitation?
The clinician should assess vital signs and monitor for recurrent cardiac arrhythmias. Continuous electrocardiographic (ECG) monitoring should continue after ROSC, during transport, and throughout ICU care until stability has been achieved. Intravenous (IV) access should be obtained if not already established and the position and function of any intravenous catheter verified. IV lines should be promptly established to replace emergent intraosseous access achieved during resuscitation. If the patient is hypotensive (systolic blood pressure <90 mm Hg), fluid boluses can be considered. Cold fluid may be used if therapeutic hypothermia is elected. Vasoactive drug infusions such as dopamine, norepinephrine, or epinephrine may be initiated if necessary and titrated to achieve a minimum systolic blood pressure of ≥90 mm Hg or a mean arterial pressure of ≥65 mm Hg.
What oxygen level should be used for resuscitation?
Although 100% oxygen may have been used during initial resuscitation, providers should titrate inspired oxygen to the lowest level required to achieve an arterial oxygen saturation of ≥94%, so as to avoid potential oxygen toxicity. It is recognized that titration of inspired oxygen may not be possible immediately after out-of-hospital cardiac arrest until the patient is transported to the emergency department or, in the case of in-hospital arrest, the intensive care unit (ICU). Hyperventilation or “overbagging” the patient is common after cardiac arrest and should be avoided because of potential adverse hemodynamic effects. Hyperventilation increases intrathoracic pressure and inversely lowers cardiac output. The decrease in Pa co2 seen with hyperventilation can also potentially decrease cerebral blood flow directly. Ventilation may be started at 10 to 12 breaths per minute and titrated to achieve a P etco2 of 35 to 40 mm Hg or a Pa co2 of 40 to 45 mm Hg.
Do corticosteroids help with stress?
Corticosteroids have an essential role in the physiological response to severe stress, including maintenance of vascular tone and capillary permeability. In the post–cardiac arrest phase, several authors report a relative adrenal insufficiency compared with the metabolic demands of the body. 188, 189 Relative adrenal insufficiency in the post–cardiac arrest phase was associated with higher rates of mortality. 188 – 190
