How is obesity defined in Ans 4 4?
4.Within appropriate range of ideal weight ANS: 1 Obesity is defined as greater than 120% of ideal body weight. For this patient, 120% of her ideal body weight, 120 pounds, is 144 pounds. Her current weight of 146 pounds is greater than 120% of ideal body weight.
How much tidal volume is needed to ventilate an obese patient?
They require a tidal volume of 10 mL/kg of body weight. Laying the patient supine often results in hyperventilation syndrome. The weight of adipose tissue on the chest wall makes ventilation of obese patients more difficult.
What are the 4 parameters used for Nutrition Screening?
ANS: 4 Parameters used for nutrition screening typically include weight and weight history, conditions associated with increased nutritional risk, diet information, and routine laboratory data. A patient is asked to indicate on a form how many times he eats a specific food.
What must the nurse remember during a nutritional assessment?
During a nutritional assessment of a 22-year-old male refugee, the nurse must remember to: 1.obtain a 24-hour dietary recall. 2.clarify what is meant by the term "food."
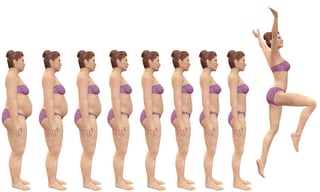
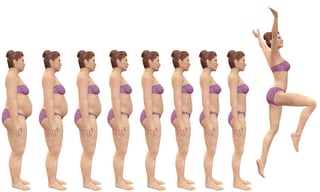
What is the definition of obesity?
The definition of obesity has been evolving over the past few decades. Historically, obesity has been defined simply as an excess of body fat [9]. Today, however, measurement of body weight and height is most often utilized as a measure of obesity. Initially, weight-for-height tables were used to determine the normal weight range ...
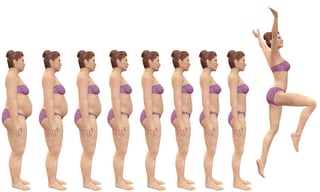
What percentage of the population is obese?
Since 1960, the prevalence of obesity has been on an upward trajectory, with rates increasing dramatically in the past few decades. In 1980, the percentage of obese and extremely obese adults was 15% and 1.4% of the total population, respectively; by 1994, the numbers had increased to 23.2% and 3.0% [1]. In the year 2000, 30.9% of the adult population was obese and 5.0% were extremely obese [1]. Data collected in 2017–2018 show that 42.4% are obese and 9.2% are extremely obese (class III); an additional 31.9% of adults are overweight [1, 75]. That means that more than 83% of Americans 20 years of age or older are above a healthy weight and are at an increased risk for disease and early death.
What is the BMI for bariatric surgery?
In 2013, cosponsored guidelines from the American Association of Clinical Endocrinologists (AACE), the Obesity Society (TOS), and ASMBS were released reaffirming BMI criteria, and adding the consideration of bariatric surgery for individuals with a BMI between 30–34.9 with diabetes or metabolic syndrome [96]. In 2019, the AACE/TOS/ASMBS/Obesity Medicine Association (OMA)/American Society of Anesthesiologists (AASA) guidelines further added a recommendation that the BMI requirement for bariatric surgery should be adjusted for ethnicity (e.g., 18.5 to 22.9 is normal range, 23 to 24.9 is overweight, and ≥25 is obesity for Asian patients) [97].
What are the diseases associated with obesity?
Genetic diseases with associated obesity include Schinzel syndrome, Bardet-Biedel syndrome, Albright hereditary osteodystrophy, and Prader-Willi syndrome. Many of these genetic disorders present with dysmorphic features, developmental delay, and obesity in addition to changes seen specifically with each disorder [22]. For instance, young males with Prader-Willi syndrome present with the features described above as well as with linear growth defects and undescended testicles.
Can leptin be used to treat obesity?
Further investigations revealed that injections of leptin in ob mice could cure obesity and diabetes. After locating the human homologues to the leptin gene and its receptor in 1999, the chromosomal locus containing the leptin gene was determined to be genetically related to human body weight [21].
Does Medicare cover weight loss?
Starting in January 2006, Medicare began to offer prescription drug plans, whereby it would assist in the payment of enrolled individuals' medications. Weight-loss medications such as orlistat may be covered; many variables contribute to the amount of coverage available. Effective in 2006, Medicare/Medicaid covers RYGB, BPD/DS (or gastric reduction duodenal switch), and LGB for patients with BMIs of 35 or greater, who have one or more comorbid conditions, and who have unsuccessfully attempted behavioral or pharmacologic interventions [93]. All other bariatric surgeries for obesity alone are not covered. As of 2013, the procedures are not required to be performed at an approved facility [106]. Medicare/Medicaid provides more information and implementation tools on its website at https://www.cms.gov.
Is obesity a genetic trait?
Overall, the relationship between genetics and obesity cannot be fully determined at this time. Evidence suggests a link between the two, implying that genetics is one of the complex factors involved in the development of this prevalent condition. Although many argue that "obesity genes" cannot be responsible for the epidemic, because the gene pool in the United States had not changed significantly between 1980 and 1994, the etiology of obesity is most likely multifactorial [23]. In 2010, one group of researchers confirmed 14 genetic variations and discovered an additional 18 variations associated with obesity [77]. In 2015, the group published additional research that identified a total of 97 genetic variations [111]. Although the progress with genetic variations related to BMI is promising, further research is needed to clarify the influence of genetics.
Why are patients in need reluctant to be transported?
Patients who are in need may be reluctant to be transported because they cannot afford medical treatment.
How long can a patient breathe on his own?
The patient can breathe adequately on his own for several minutes to several hours if you are not able to transport his ventilator with him.
When is EMS called?
EMS may be called when the chronic condition worsens or a medical device fails.
Should you assume patients have difficulty understanding your explanations?
Even when patients express themselves normally, you should assume they have difficulty understanding your explanations.
Can a patient understand your explanations?
Even though the patient has difficulty expressing himself, you should assume he can understand your explanations.
What are the parameters used for nutrition screening?
Parameters used for nutrition screening typically include weight and weight history, conditions associated with increased nutritional risk, diet information, and routine laboratory data. A patient is asked to indicate on a form how many times he eats a specific food.
Why is total cholesterol measured?
Total cholesterol is measured to evaluate fat metabolism and to assess the risk of cardiovascular disease. Serum triglycerides are used to screen for hyperlipidemia and to determine the risk of coronary artery disease. A 40-year-old man has had a recent weight loss of 20 pounds because of a quick loss diet and stress.
What are the most common health problems of immigrants from developing countries?
ANS: 3. General undernutrition, hypertension, diarrhea, lactose intolerance, osteomalacia (soft bones), scurvy, and dental caries are among the more common nutrition- related problems of new immigrants from developing countries. During a nutritional assessment of a 22-year-old male refugee, the nurse must remember to:
What does the examiner ask about when a change occurs?
With changes in appetite, taste, smell, or chewing or swallowing, the examiner asks about the type of change and when the change occurred. The nurse is performing a nutritional assessment on a 15-year-old girl, who tells the nurse that she is "so fat.".
What are the vulnerable groups?
Vulnerable groups are infants, children, pregnant women, recent immigrants, persons with low incomes, hospitalized people, and aging adults. Click again to see term 👆. Tap again to see term 👆. When assessing a patient's nutritional status, the nurse recalls that the best definition of optimal nutritional status is:
Why is it important to have a low calorie diet?
4.The importance of a low-calorie diet to prevent the accumulation of fat
How to prevent lean muscle catabolism?
1.Decrease the amount of carbohydrates to prevent lean muscle catabolism. 2.Increase the amount of soy and tofu in her diet to promote bone growth and reverse osteoporosis. 3.Decrease the number of calories she is eating because of the decrease in energy requirements from loss of lean body mass.
Which branch of medicine deals with the cause, prevention, and treatment of which of the following diseases?
Acquired disease. Bariatrics is defined as the branch of medicine that deals with the cause, prevention, and treatment of which of the following diseases? obesity. You are transporting a resident of a nursing home to the hospital for a complaint of abdominal pain that has lasted for 3 days.
What is Chloe's condition?
Chloe was born with a cardiac problem that she will have to manage the rest of her life. This disease is considered
What is the least effective way to determine how much the patient understands?
A) Speaking with the patient's family is the least effective way to determine how much the patient understands.
Why is communication important with the patient's caregiver or family members?
D) Communication with the patient's caregiver or family members is important because they are the most familiar with the patient's condition.