What is a CHD?
CHDs can vary from mild (such as a small hole in the heart) to severe (such as missing or poorly formed parts of the heart). About 1 in 4 babies born with a heart defect has a critical CHD (also known as critical congenital heart disease). 1 Babies with a critical CHD need surgery or other procedures in the first year of life.
Which critical heart disease screening targets are most likely to detect CHDS?
Pulse oximetry screening is most likely to detect seven of the critical CHDs. These seven main screening targets are hypoplastic left heart syndrome, pulmonary atresia, tetralogy of Fallot, total anomalous pulmonary venous return, transposition of the great arteries, tricuspid atresia, and truncus arteriosus.
Is there a cure for CHD?
Even with improved treatments, many people with a CHD are not cured, even if their heart defect has been repaired. People with a CHD can develop other health problems over time, depending on their specific heart defect, the number of heart defects they have, and the severity of their heart defect.
How are congenital heart defects (CHDs) diagnosed and treated?
If a healthcare provider suspects a CHD may be present, the baby can get several tests (such as an echocardiogram) to confirm the diagnosis. Treatment for CHDs depends on the type and severity of the defect present. Some affected infants and children might need one or more surgeries to repair the heart or blood vessels.
What Are Critical Congenital Heart Defects (Critical Chds)?
In the United States, about 7,200 babies born every year have critical CHDs.2 Typically, these types of heart defects lead to low levels of oxygen...
Importance of Newborn Screening For Critical Chds
Some CHDs may be diagnosed during pregnancy using a special type of ultrasound called a fetal echocardiogram, which creates pictures of the heart o...
How Newborn Screening For Critical Chds Is Done
Newborn screening for critical CHDs involves a simple bedside test called pulse oximetry. This test estimates the amount of oxygen in a baby’s bloo...
Timing of Critical Chd Screening
Screening is done when a baby is at least 24 hours of age, or as late as possible if the baby is to be discharged from the hospital before he or sh...
Pulse Oximetry Screening Results
Pulse oximetry screening is most likely to detect seven of the critical CHDs. These seven main screening targets are hypoplastic left heart syndrom...
What are the conditions that children with congenital heart defects need to be treated for?
Children and adults with congenital heart defects may need medical treatment for a number of common conditions, including: Congestive heart failure.
What are the special needs of children with CHD?
Special needs for children with CHD. Physical activity for those with congenital heart defects. Heart-health recommendations for those with CHD. If you are a parent caring for a child with a congenital heart defect, the American Heart Association wants to be there for you.
Why is cardiac catheterization needed?
In other cases, surgery or a cardiac catheterization may be needed to reduce the effects of the heart defect, or to repair the defect. Even when a defect is treated in childhood, further conditions may develop later, making additional medical treatment beneficial.
What are the most common CHDs detected by pulse oximetry?
Pulse oximetry screening is most likely to detect seven of the critical CHDs. These seven defects are hypoplastic left heart syndrome, pulmonary atresia, tetralogy of Fallot, total anomalous pulmonary venous return, transposition of the great arteries, tricuspid atresia, and truncus arteriosus. Other heart defects can be just as severe as these ...
How many babies have a critical congenital heart defect?
Critical Congenital Heart Defects. About 1 in every 4 babies born with a heart defect has a critical congenital heart defect (critical CHD, also known as critical congenital heart disease). 1 Babies with a critical CHD need surgery or other procedures in the first year of life. Learn more about critical CHDs below.
What does it mean when a baby passes a CHD?
If the baby passes the screen (also called “negative” or “in-range” result), it means that the baby’s test results did not show signs of a low level of oxygen in the blood. A baby that passes the screen is unlikely to have a critical CHD. However, not all babies with a critical CHD will have a low level of oxygen in the blood that is detected during newborn screening. Thus, it is possible for a baby who passes the screen to still have a critical CHD or other CHD.
When do babies need surgery for CHD?
Babies with a critical CHD need surgery or other procedures in the first year of life. Other heart defects can be just as severe as critical CHDs and may also require treatment soon after birth.
What is a newborn screening?
Newborn screening is a tool that can identify some of these babies so they can receive prompt care and treatment. Timely care may prevent disability or death early in life.
Why does my baby have low oxygen levels?
There may be other causes, such as breathing problems, for low levels of oxygen in the blood. The baby’s doctor might recommend that the baby get screened again or have more specific tests, like an echocardiogram (an ultrasound picture of the heart), to diagnose a critical CHD.
How to tell if a baby has a CHD?
Low levels of oxygen in the blood can be a sign of a critical CHD. The test is done using a machine called a pulse oximeter, with sensors placed on the baby’s skin. The test is painless and takes only a few minutes.
Why is physical activity important?
Physical activity helps you achieve and maintain a healthy weight and control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. If you have a heart arrhythmia or heart defect, there may be some restrictions on the activities you can do, so talk to your doctor.
What should your LDL be if you have diabetes?
If you're at very high risk of heart disease — if you've already had a heart attack or have diabetes, for example — aim for an LDL level below 70 mg/dL (1.8 mmol/L). Keep diabetes under control. If you have diabetes, tight blood sugar control can help reduce the risk of heart disease. Exercise.
What is the recommended LDL level?
Most people should aim for a low-density lipoprotein (LDL) level below 130 milligrams per deciliter (mg/dL), or 3.4 millimoles per liter (mmol/L). If you have other risk factors for heart disease, you should aim for an LDL level below 100 mg/dL (2.6 mmol/L).
What tests are needed to diagnose heart disease?
The tests you'll need to diagnose your heart disease depend on what condition your doctor thinks you might have. Besides blood tests and a chest X-ray, tests to diagnose heart disease can include: Electrocardiogram (ECG or EKG). An ECG is a quick and painless test that records the electrical signals in your heart.
What is the noninvasive exam that shows how your heart beats and pumps blood?
Echocardiogram. This noninvasive exam uses sound waves to produce detailed images of your heart's structure. It shows how your heart beats and pumps blood. Stress test. This type of test involves raising your heart rate with exercise or medicine while performing heart tests and imaging to check how your heart responds.
How to help a heart attack?
Here are some ways to help cope with heart disease or improve your condition: Cardiac rehabilitation. For people who have cardiovascular disease that's caused a heart attack or has required surgery to correct, cardiac rehabilitation is often recommended as a way to improve treatment and speed recovery.
How much weight can I lose to prevent heart disease?
Being overweight increases your risk of heart disease. A body mass index (BMI) of less than 25 and a waist circumference of 35 inches (88.9 centimeters) or less is the goal for preventing and treating heart disease. Manage stress. Reduce stress as much as possible.
What Are Congenital Heart Defects (Chds)?
Types
- Listed below are examples of different types of CHDs. The types marked with a star (*) are considered critical CHDs. 1. Atrial Septal Defect 2. Atrioventricular Septal Defect 3. Coarctation of the Aorta* 4. Double-outlet Right Ventricle* 5. d-Transposition of the Great Arteries* 6. Ebstein Anomaly* 7. Hypoplastic Left Heart Syndrome* 8. Interrupted Aortic Arch* 9. Pulmonary Atresia…
Signs and Symptoms
- Signs and symptoms for CHDs depend on the type and severity of the particular defect. Some defects might have few or no signs or symptoms. Others might cause a baby to have the following symptoms: 1. Blue-tinted nails or lips 2. Fast or troubled breathing 3. Tiredness when feeding 4. Sleepiness
Diagnosis
- Some CHDs may be diagnosed during pregnancy using a special type of ultrasound called a fetal echocardiogram, which creates ultrasound pictures of the heart of the developing baby. However, some CHDs are not detected until after birth or later in life, during childhood or adulthood. If a healthcare provider suspects a CHD may be present, the baby can get several tests (such as an …
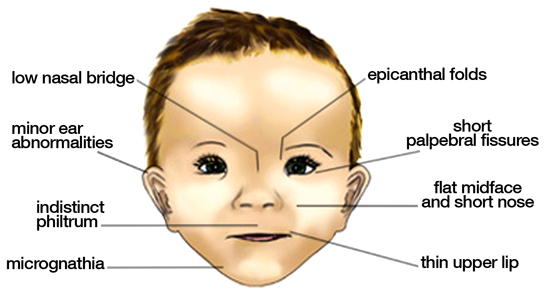
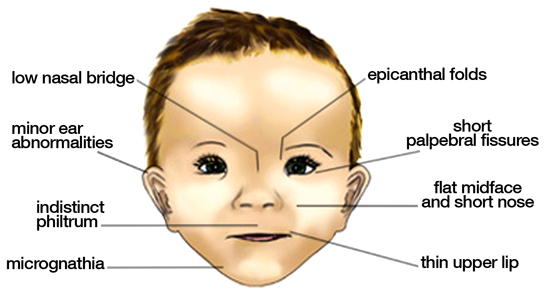
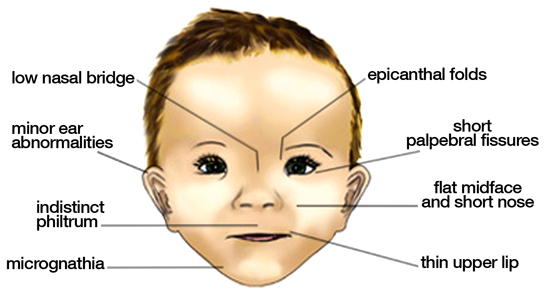
Causes
- The causes of CHDs among most babies are unknown. Some babies have heart defects because of changes in their individual genes or chromosomes. CHDs also are thought to be caused by a combination of genes and other factors, such as things in the environment, the mother’s diet, the mother’s health conditions, or the mother’s medication use during pregnancy. For example, certa…
Living with A Chd
- As medical care and treatment have advanced, infants with CHDs are living longer and healthier lives. Many children with CHDs are now living into adulthood. It is estimated that more than two million individuals in the United States are living with a CHD. Many people with a CHD lead independent lives with little or no difficulty. Others might develop disability over time. Some peo…
References
- Oster M, Lee K, Honein M, Colarusso T, Shin M, Correa A. Temporal trends in survival for infants with critical congenital heart defects. Pediatrics. 2013;131(5):e1502-8.
- Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, Elixson M, Warnes CA, Webb CL. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific st...
- Oster M, Lee K, Honein M, Colarusso T, Shin M, Correa A. Temporal trends in survival for infants with critical congenital heart defects. Pediatrics. 2013;131(5):e1502-8.
- Jenkins KJ, Correa A, Feinstein JA, Botto L, Britt AE, Daniels SR, Elixson M, Warnes CA, Webb CL. Noninherited risk factors and congenital cardiovascular defects: current knowledge: a scientific st...
- Patel SS, Burns TL. Nongenetic risk factors and congenital heart defects. Pediatr Cardiol.2013;34(7):1535-55.