
Does a heart block require a pacemaker?
Heart block that occurs within the AV node (so-called "proximal" heart block) is usually pretty benign, and often does not require a permanent pacemaker. When the block is occurring within the AV node, subsidiary pacemaker cells in the AV node just beyond the site of the block often take over the rhythm of the heart.
What is the long-term treatment for an AV block?
Long-term treatment of AV block: permanent artificial pacemaker First-degree AV block and second-degree AV block Mobitz type I: Only necessitates pacemaker if symptomatic. The indication is stronger if the QRS complexes are wide.
When is a pacemaker necessary for a Mobitz type 1 AV block?
First-degree AV block and second-degree AV block Mobitz type I: Only necessitates pacemaker if symptomatic. The indication is stronger if the QRS complexes are wide.
Is pacemaker implantation indicated for first-degree atrioventricular (AV) block?
Permanent pacemaker implantation is not indicated for asymptomatic first-degree AV block (class III recommendation; level of evidence, B). In the absence of a disease process that requires admission, patients with first-degree AV block may be safely discharged and receive follow-up on an outpatient basis.
Which heart block requires a pacemaker?
A third degree heart block can cause a wide range of symptoms, some of which are life-threatening. This type of heart block is usually regarded as a medical emergency and may require immediate treatment with a pacemaker (an artificial electrical device that is used to regulate heartbeats).
Do you need a pacemaker with AV block?
With first-degree heart block, you might not need treatment. With second-degree heart block, you may need a pacemaker if symptoms are present or if Mobitz II heart block is seen. With third-degree heart block, you will most likely need a pacemaker.
What is the treatment for 3rd degree AV block?
Transcutaneous pacing is the treatment of choice for any symptomatic patient. All patients who have third-degree atrioventricular (AV) block (complete heart block) associated with repeated pauses, an inadequate escape rhythm, or a block below the AV node (AVN) should be stabilized with temporary pacing.
Does Mobitz Type 1 require treatment?
Mobitz I block Symptomatic patients should be treated with atropine and transcutaneous pacing. However, atropine should be administered with caution in patients with suspected myocardial ischemia, as ventricular dysrhythmias can occur in this situation.
When is a pacemaker required?
Your doctor may recommend a temporary pacemaker when you have a slow heartbeat (bradycardia) after a heart attack, surgery or medication overdose but your heartbeat is otherwise expected to recover. A pacemaker may be implanted permanently to correct a chronic slow or irregular heartbeat or to help treat heart failure.
What is the difference between Type 1 and Type 2 second-degree heart block?
Both Mobitz type 1 block and type 2 block result in blocked atrial impulses (ECG shows P-waves not followed by QRS complexes). The hallmark of Mobitz type 1 block is the gradual prolongation of PR intervals before a block occurs. Mobitz type 2 block has constant PR intervals before blocks occur.
How do you treat type 2 mobitz?
Treatment for a Mobitz type II involves initiating pacing as soon as this rhythm is identified. Type II blocks imply structural damage to the AV conduction system. This rhythm often deteriorates into complete heart block. These patients require transvenous pacing until a permanent pacemaker is placed.
What is second-degree type 2 heart block?
A second-degree type II AV block indicates significant conduction disease in this His-Purkinje system and is irreversible (not subject to autonomic tone or AV blocking medications). This is a very important distinguishing factor compared to second-degree type I AV block.
What is 1st 2nd and 3rd degree heart block?
8:039:17AV Blocks (1st, 2nd, and 3rd Degree) - YouTubeYouTubeStart of suggested clipEnd of suggested clipThere are no dropped beats in a first-degree AV block. In a second-degree AV block there are twoMoreThere are no dropped beats in a first-degree AV block. In a second-degree AV block there are two types the first type is a mobitz type one.
What is the difference between Mobitz I and Mobitz II?
Mobitz 1 and 2 are the two forms of second-degree heart block. The difference between them is in mobitz 1 there is a gradual increase in the duration of PR interval until an impulse completely wanes off before reaching the ventricles but in mobitz 2 although the PR interval is prolonged it does not change with time.
How can you tell the difference between a Mobitz I and Mobitz II heart block?
Unlike Mobitz I, which is produced by progressive fatigue of the AV nodal cells, Mobitz II is an “all or nothing” phenomenon whereby the His-Purkinje cells suddenly and unexpectedly fail to conduct a supraventricular impulse.
What is the treatment for 1st degree AV block?
In general, no treatment is required for first-degree AV block unless prolongation of the PR interval is extreme (>400 ms) or rapidly evolving, in which case pacing is indicated. Prophylactic antiarrhythmic drug therapy is best avoided in patients with marked first-degree AV block.
Can a transcutaneous pacemaker be withdrawn?
Transcutaneous pacemaker is a painful method which mandates sedation but should not be withdrawn if the situation is life-threatening. Any medications causing or aggravating the block must be withdrawn. AV blocks due to reversible causes does not need permanent pacemaker.
Is Holter ECG necessary?
Holter ECG may be valuable if the diagnosis is uncertain. Otherwise, no further examination is needed beyond the 12-lead ECG. Echocardiography is generally not necessary. Management of AV blocks aims to restore atrioventricular conduction either pharmacologically or by means of artificial pacemakers. Both methods may be used in the acute setting, ...
Does atropine block AV node?
Atropine will have effect if the block is located in the AV node. Note that atropine may aggravate the block if it is located distal to the AV node. Isoprenaline (isoproterenol, 5 micrograms per minute) may also be administered (with caution in case of acute coronary syndromes, as isoprenaline may trigger ventricular tachycardia).
Overview
In heart block, when the heart’s electrical impulses try to travel from the heart’s atrial chambers to the ventricular chambers, they are partially or completely blocked. Because these electrical impulses let the heart know when it should beat, if the heart block is severe enough, it can slow the heart rate to dangerously low levels.
Causes of heart block
A transient heart block is not always dangerous or even abnormal. Transient heart block is common in young, healthy people with a sudden increase in vagal tone.
heart block symptoms
Depending on its severity, heart block can produce a range of symptoms, from no symptoms at all to dizziness, fainting (loss of consciousness), and even death.
degree of heart block
Health care providers classify heart block as one of three “degrees.” Your healthcare provider can use an electrocardiogram (ECG) to determine the extent of your heart block. The higher the degree of blockade, the more dangerous the heart block may be.
location of heart block
During normal heart rhythm, the heart’s electrical impulses must pass through the junction between the atria and ventricles (atrioventricular junction). This AV junction consists of two structures:
What is a Mobitz II block?
Mobitz II, or Type II, second degree AV block, can be confused with a nonconducted premature atrial complex. In Mobitz II block, the electrocardiogram (EKG) shows a constant P–R interval, followed by a sudden failure of a P wave to be conducted to the ventricles.
What is the P–R interval of AV block?
First-degree AV block, with a P–R interval greater than 200 ms , is rarely found in young, healthy adults during activity. However, a longer P–R interval, and even Mobitz I (Wenckebach) block can be seen in young, well-conditioned individuals at rest and during sleep. The P–R interval decreases and the Wenckebach block disappears with increased activity, and is considered normal vagal influence on the AV node.
What is surface EKG?
The surface EKG is our most important tool for the diagnosis of AV block and intraventricular conduction disturbances. First-degree AV block is seen as a P–R interval >200 ms and each P wave is followed by a QRS complex with a constant, prolonged interval (Figure 2).
How long can you keep anticoagulant for atrial fibrillation?
Patients on anticoagulants who need temporary or permanent pacemaker placement are at increased risk of bleeding complications. If the procedure is not emergent, and the patient is on warfarin for atrial fibrillation, the drug can be withheld for 3 to 5 days, and restarted postprocedure when the risk of bleeding is acceptable.
What is a slowed conduction?
Slowed conduction, or blocked conduction, can occur anywhere along the path of conduction fibers, and can generally be identified by EKG analysis. Infra-Hisian block is the most important to identify, since it is the cause of most cases of symptomatic complete heart block.
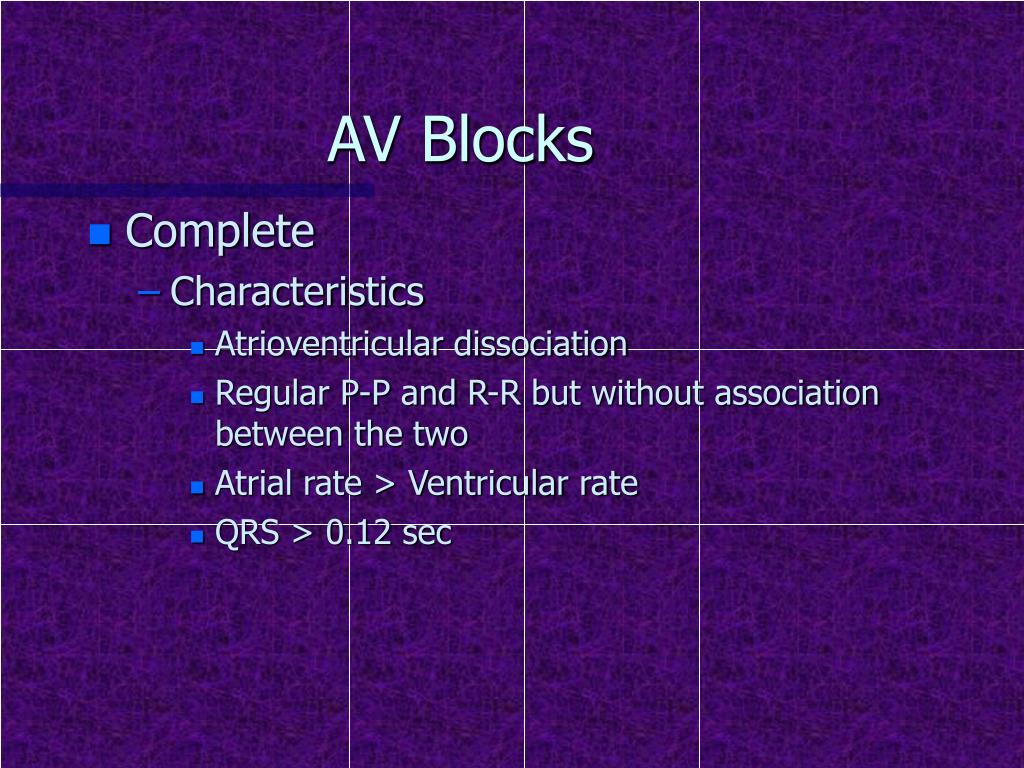
Why is my heart block reversible?
Reversible causes of complete heart block can be due to metabolic abnormalities, drug effects, Lyme disease, or vasovagal episodes. In these cases, the complete heart block resolves once the abnormality has been treated. In true complete heart block, the sinus rate is faster than the ventricular rate.
What causes AV block?
Acquired AV block is most commonly caused by idiopathic fibrosis, acute myocardial infarction, or drug effects. AV block can also be congenital. If AV block is symptomatic, and determined to be permanent, pacing is the only effective long-term therapy. Conduction Terminology.
