Symptoms
What medical care will I receive if I may have been exposed to rabies? Postexposure prophylaxis (PEP) consists of a dose of human rabies immune globulin (HRIG) and rabies vaccine given on the day of the rabies exposure, and then a dose of vaccine given again on days 3, 7, and 14.
Causes
Once a person is infected, there is not much a doctor can do to treat it. If a dog, cat, bat, or other mammal you might suspect has rabies has bitten you, get to the doctor. The first dose of the vaccine should be administered within the first 24 hours after exposure.
Prevention
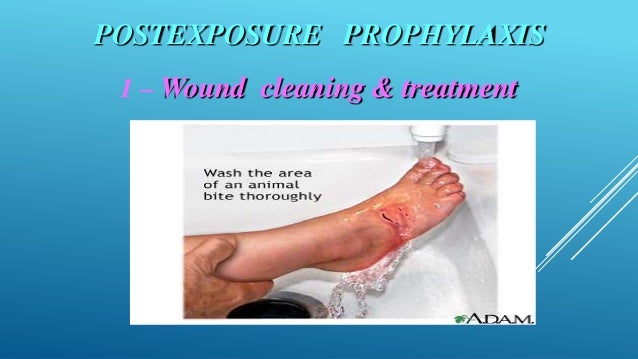
Anyone who has been bitten by an animal suspected to have rabies, or who otherwise may have been exposed to rabies, should clean the wound and see a health care provider immediately regardless of vaccination status. The health care provider can help determine if the person should receive post-exposure rabies vaccination.
Complications
Postexposure prophylaxis (PEP) consists of a dose of human rabies immune globulin (HRIG) and rabies vaccine given on the day of the rabies exposure, and then a dose of vaccine given again on days 3, 7, and 14. For people who have never been vaccinated against rabies previously, postexposure prophylaxis ...
What medical care will I receive if I have been exposed to rabies?
When should I go to the doctor for rabies?
What should I do if I’m bitten by a rabies animal?
What is postexposure prophylaxis for rabies?
What should you do if you are potentially exposed to rabies?
WASH: Immediately wash wounds/exposed areas with soap and clean running water for 15 minutes. The patient should visit a physician or emergency department for wound care and assessment of the need for antibiotics, tetanus post-exposure prophylaxis (PEP) and for Rabies Risk Assessment for rabies PEP (Step 3).
How quickly must rabies be treated?
If a dog, cat, bat, or other mammal you might suspect has rabies has bitten you, get to the doctor. The first dose of the vaccine should be administered within the first 24 hours after exposure. Emergency room physician Dr.
Where do you get injected for rabies?
The vaccine is injected into the upper arm muscle (deltoid). Very young or small children may have the vaccine injected into the upper leg (thigh) muscle.
Can I take rabies vaccine after 3 days?
The first dose should be given as soon as possible after the exposure. Additional doses should be given on days three, seven, and 14 after the first shot. These shots should be given in the deltoid muscle of the arm.
Is it too late to get rabies vaccine?
Once a person develops rabies symptoms it is too late to vaccinate against rabies!
Can I take rabies vaccine after 24 hours?
Rabies immunoglobulin for passive immunization is administered only once, preferably within 24 hours after the exposure (on day 0 along with the first dose of anti-rabies vaccine).
Can I take rabies vaccine after 4 days?
The first dose of the 5-dose course should be administered as soon as possible after exposure. This date is then considered day 0 of the post exposure prophylaxis series. Additional doses should then be administered on days 3, 7, 14, and 28 after the first vaccination.
Can I take rabies injection after 2 weeks?
Once it enters the nerves, it is the end of the person. Therefore to neutralise, kill or inactivate the virus, immunoglobulins or rabies monoclonal antibodies must be injected into the wound. Then the vaccine must be given over a period of a month, multiple times; the antibodies from which form after 2 weeks," said Dr.
Can a normal person take rabies vaccine?
Rabies vaccine is given to persons who have been exposed (eg, by a bite, scratch, or lick) to an animal that is known, or thought, to have rabies. This is called post-exposure prophylaxis. Rabies vaccine may also be given ahead of time to persons who have a high risk of getting infected with rabies virus.
Can rabies occur after 20 years?
We report an unusual case of rabies, with very prolonged incubation period suspected to be more than 20 years, from the South Western state of India, Goa.
How long does it take to show signs of rabies in humans?
In people, the incubation period (the time between initial contact with the virus and onset of the disease) generally ranges from two to eight weeks. In rare cases, it can vary from 10 days to 2 years. The incubation period is shorter in children and in people exposed to a large dose of the rabies virus.
How do you treat rabies without a vaccine?
Once a rabies infection is established, there's no effective treatment. Though a small number of people have survived rabies, the disease usually causes death. For that reason, if you think you've been exposed to rabies, you must get a series of shots to prevent the infection from taking hold.
Can I take rabies vaccine after 4 days?
The first dose of the 5-dose course should be administered as soon as possible after exposure. This date is then considered day 0 of the post exposure prophylaxis series. Additional doses should then be administered on days 3, 7, 14, and 28 after the first vaccination.
How long after a dog bite should I get a rabies shot?
To prevent rabies, four to five doses of anti-rabies vaccine are administered on the 0, 3, 7, 14 and 28 days of a bite.
Can we take rabies vaccine after 10 days?
✓ If the bite is by a dog or cat and the animal is alive & healthy till 10 days after bite or it is humanely killed and its brain is found to be negative for rabies in the lab, vaccination may be stopped after the 3rd dose (dose of day 7).
Can I take rabies injection after 2 weeks?
Once it enters the nerves, it is the end of the person. Therefore to neutralise, kill or inactivate the virus, immunoglobulins or rabies monoclonal antibodies must be injected into the wound. Then the vaccine must be given over a period of a month, multiple times; the antibodies from which form after 2 weeks," said Dr.
What to do if you have been bitten by a rabies?
If you’ve been in contact with any wildlife or unfamiliar animals, particularly if you’ve been bitten or scratched, you should talk with a healthcare or public health professional to determine your risk for rabies or other illnesses. Wash any wounds immediately with soap and water and then plan to see a healthcare provider.
Is rabies an emergency?
Remember that rabies is a medical urgency but not an emergency. Decisions should not be delayed. See your doctor for attention for any trauma due to an animal attack before considering the need for rabies vaccination.
What is PEP in rabies?
Postexposure prophylaxis (PEP) consists of a dose of human rabies immune globulin (HRIG) and rabies vaccine given on the day of the rabies exposure, and then a dose of vaccine given again on days 3, 7, and 14.
What are the side effects of rabies shots?
Mild, local reactions to the rabies vaccine, such as pain, redness, swelling , or itching at the injection site, have been reported.
Does PEP include rabies?
For people who have never been vaccinated against rabies previously , postexposure prophylaxis (PEP) should always include administration of both HRIG and rabies vaccine.
Is rabies prevention a serious matter?
Rabies prevention is a serious matter and changes should not be made in the schedule of doses. Patient assistance programs that provide medications to uninsured or underinsured patients are available for rabies vaccine and immune globulin.
Can you transmit rabies to other people?
People cannot transmit rabies to other people unless they themselves are sick with rabies. PEP will protect you from developing rabies, and therefore you cannot expose other people to rabies. You can continue to participate in your normal activities.
Can rabies cause headaches?
Rarely, symptoms such as headache, nausea, abdominal pain, muscle aches, and dizziness have been reported. Local pain and low-grade fever may follow injection of rabies immune globulin. The vaccine should be given at recommended intervals for best results.
What is the weakened form of rabies?
The Rabies Vaccine. Like all vaccines, rabies vaccines contain a weakened form of the virus that is incapable of causing disease or reproducing. In response to the vaccine, your body produces antibodies that target and kill the rabies virus.
What is PEP in rabies?
Post-exposure prophylaxis (PEP) is the only treatment strategy known to prevent rabies-related deaths. 4 This treatment includes extensive washing and local treatment of the wound followed by a course of a potent and effective rabies vaccine.
What is the first category of exposure to rabies?
The guidelines identify three categories of rabies exposure. The first category is defined as "touching or feeding animals, licks on intact skin," but post-exposure prophylaxis (PEP) is recommended only for category 2 and category 3 exposure. 8.
What animals are most likely to get rabies?
2 The rabies virus may also be spread by such animals as foxes, skunks, and raccoons. Across the globe, over 90 percent of human rabies cases result from virus transmission by domestic dogs. 3 .
What to do after a rabies bite?
In addition to seeking medical attention right after an animal bite (especially from a bat, fox, or skunk), the wound should be cleaned immediately and thoroughly.
What are the side effects of a booster shot?
Symptoms at the injection site such as soreness, redness, swelling, or itching. Systemic side effects including headache, nausea, stomach pain, muscle aches, or dizziness. After booster shots, some people develop hives, joint pain, or fever.
How long does it take to die from rabies?
Once symptoms set in, however, death from respiratory failure usually occurs within seven days —even if treatment is given.
How is rabies transmitted?
Rabies virus is transmitted through direct contact (such as through broken skin or mucous membranes of the eyes, nose, or mouth) with infectious tissue or fluids.
How does rabies get killed?
Rabies virus is fragile and is killed by desiccation (drying out), ultra-violet light, and common disinfectants. Healthcare workers providing care to patients with suspected or confirmed rabies (i.e., encephalitis of unknown origin) should protect themselves by using standard precautions.
How do you get rabies?
The most common way people get rabies is after being exposed to a rabid animal. Human-to-human transmission of rabies virus has only been documented from infected organ/tissue donors to transplant recipients. There have been no other confirmed instances of human-to-human transmission, including in healthcare settings.
What do you wear to help a patient with rabies?
This includes wearing gowns, goggles, masks, and gloves, particularly during intubation and suctioning. Healthcare workers caring for patients with rabies do not pose a risk to their families or community.
Is rabies transmitted through clothing?
The exposure of intact skin to infectious tissue or fluids rarely constitutes a risk for virus transmission. Rabies is not transmitted through contaminated objects or materials such as clothes or bedding. Rabies virus is fragile and is killed by desiccation (drying out), ultra-violet light, and common disinfectants.
How does rabies affect people?
Most rabies deaths in people around the world are caused by bites from unvaccinated dogs. Rabies infects the central nervous system. After infection with rabies, at first there might not be any symptoms. Weeks or even months after a bite, rabies can cause general weakness or discomfort, fever, or headache.
How to contact CDC about rabies?
Call your local or state health department. Contact the Centers for Disease Control and Prevention (CDC): Call 1-800-232-4636 (1-800-CDC-INFO) or. Visit CDC’s rabies website. Many Vaccine Information Statements are available in español and other languages. See http://www.immunize.org/vis.
What is the most common source of rabies?
Humans get rabies when they are bitten or scratched by infected animals. Human rabies is rare in the United States. Wild animals like bats, raccoons, skunks, and foxes are the most common source of human rabies infection in the United States. Rabies is more common in other parts of ...
Can you postpone rabies shots?
Has a weakened immune system. In some cases, your health care provider may decide to postpone a routine (non-exposure) dose of rabies vaccination to a future visit. People with minor illnesses, such as a cold, may be vaccinated.
Do you need rabies immunoglobulin?
A person who has been previously vaccinated should get 2 doses of rabies vaccine and does not need Rabies Immune Globulin. Your health care provider can give you more information.
Who are the Spelunkers?
Spelunkers (people who explore caves), and. Persons who work with live vaccine to produce rabies vaccine and rabies immune globulin. Pre-exposure rabies vaccination should also be considered for: People whose activities bring them into frequent contact with rabies virus or with possibly rabid animals.
Who should get rabies shots?
People at high risk of exposure to rabies should be offered pre-exposure rabies vaccination, including: Veterinarians, animal handlers, and veterinary students. Rabies laboratory workers.
What is the treatment for rabies exposure?
Treatment for rabies exposure is called Post Exposure Prophylaxis. During your first visit, rabies immune globulin (RIG) is administered regardless of the length of time from exposure. Rabies vaccine is also administered on that same day. Additional dosages of rabies vaccine are given on day 3, 7, and 14.
How is rabies spread?
Rabies is spread by saliva or exposure to brain/nervous system tissue from an infected mammal. Rabies is not spread by petting an animal or by exposure to animal blood, urine, or feces. Rabies is spread when there is saliva exposure to an open wound, or if there is a bite. Rabies virus does not survive once it is dry on a surface.
How is rabies transmitted?
For more detailed information please visit http://www.cdc.gov/rabies. Rabies is a viral disease transmitted by saliva, usually from a bite of an infected animal. Any mammals can get or transmit rabies. Rabies is 100 percent preventable either by animal vaccination, or treatment following an exposure. Rabies can be spread by non-domestic animals ...
How long does rabies stay on a surface?
Rabies virus does not survive once it is dry on a surface. If someone is bit or has a possible rabies exposure, you should contain the animal if it is domestic for up to 10 days. If it is a non-domestic animal it should not be contained, but is usually euthanized if captured.
What to do if you get rabies bites?
A rabies exposure is a medical URGENCY. You should seek the guidance of your primary care provider. If they are unavailable, you should go to the emergency room. If there is a bite, wound treatment may consist of a tetanus shot, wound irrigation, closure if appropriate, possible antibiotic treatment, and discussion of rabies exposure.
How long does it take to test for rabies?
Testing for rabies antibodies takes up to 4-6 weeks and is not recommended prior to treatment after an exposure. Individuals handling animals that may be at risk for rabies exposure should have pre-exposure rabies vaccine and have periodic blood work for rabies antibody testing.
When is rig administered?
RIG is only administered if a patient has never had a rabies vaccine series.
