How are pressure ulcers managed and treated?
Strategies to manage pressure ulcers and facilitate healing include proper tissue load management (which includes proper positioning and the use of support surfaces) as well as appropriate ulcer care and management of infection. Initial ulcer care involves debridement, wound cleansing, dressing application and possible adjunctive therapy.
How are pressure ulcers treated with skin grafts?
The slimy layer over the surface of ulcer is sharply debrided to get a healthy vascular bed for skin grafting. Local flaps Variety of local flaps can be used to reconstruct the defect created by excision of pressure ulcers.
What are the most common sites of pressure ulcers?
The most common sites for pressure ulcers to occur are over a bony prominence, such as the buttock (sacrum/ischium), heels, hips (trochanter), elbows, ankles (lateral and medial malleolus), back, shoulders, back of the head (occipit) and ears. Common sites of pressure ulcers 6 Prevalence of pressure ulcers
How much does a pressure ulcer cost?
According to recent literature, hospitalizations related to pressure ulcers cost between $9.1 to $11.6 billion per year. The cost of individual patient care per pressure ulcer may range from $20,900 to $151,700.

What kind of doctor treats pressure ulcers?
A doctor who specializes in conditions of the skin (dermatologist) A neurosurgeon, vascular surgeon, orthopedic surgeon or plastic surgeon.
How is a partial-thickness wound treated?
In general, silver sulfadiazine is a good choice for deep partial-thickness burns because it may allow the wound to heal without the need for a skin graft.
What is the cost of pressure stasis ulcer treatment?
The direct costs for pressure ulcer treatment range between $2,000 and $20,000.
How do you treat a Stage 2 pressure ulcer at home?
Stage II pressure sores should be cleaned with a salt water (saline) rinse to remove loose, dead tissue. Or, your provider may recommend a specific cleanser. Do not use hydrogen peroxide or iodine cleansers. They can damage the skin.
When treating a partial thickness burn you should EMT?
For superficial and partial thickness burns, cool the burns using water or wet sterile dressing and then cover with a dry sterile dressing. Do not use creams or ointments and do not rupture any blisters. Elevate burned area if possible to reduce edema.
When do you treat a partial thickness burn?
Superficial partial-thickness or deep partial-thickness burn Soak the burn in cool water for 15 minutes. If the burned area is small, put cool, clean wet cloths on the burn for a few minutes every day. Then put on an antibiotic cream or other creams or ointments prescribed by your doctor.
Are hospitals reimbursed for pressure ulcers?
Last year, the Centers for Medicare and Medicaid Services announced that it will cease reimbursement for hospital care of eight reasonably preventable conditions – including pressure ulcers, bed sore aka decubitus ulcers – in October 2008.
Does Medicare pay for pressure ulcers?
Widespread screening is good news, Dr. White-Chu noted, because the Medicare payment guidelines state that physicians must document pressure ulcers that are present on admission. Otherwise, Medicare will not pay the treatment costs of any pressure ulcers that progress to stage III or IV during hospitalization.
What is the average treatment cost range for a Stage III pressure injury?
The estimated cost of managing stage III/IV pressure injury per patient is $70–150 thousand, and the total cost for treatment of pressure ulcers in the United States is estimated at $9–11 billion per year [4].
How is Stage 2 bed sores treated?
Treatments for stage 2 bedsores include:Removing all pressure from the area.Keeping the area clean and dry.Maintaining a nutritious diet high in protein, vitamins (especially A and C) and minerals (especially iron and zinc)Staying properly hydrated.Finding and eliminating the cause.More items...•
What's the best cream for bed sores?
Options that are antimicrobial or hydrocolloid, or that contain alginic acid, may be best. Dressings are available for purchase online. Use topical creams: Antibacterial creams can help combat an infection, while barrier creams can protect damaged or vulnerable skin.
What cream is good for leg ulcers?
The most frequently used topical antimicrobials in wound care practice are chlorhexidine, iodine, silver containing products, mupriocin and fucidic acid.
How do pressure ulcers heal?
The healing process varies depending on the stage of the pressure ulcer. Stage I & II pressure ulcers and partial thickness wounds heal by tissue regeneration. Stage III & IV pressure ulcers and full thickness wounds heal by scar formation and contraction.
What is pressure ulcer?
Previously called decubitus or bed sore, a pressure ulcer is the result of damage caused by pressure over time causing an ischemia of underlying structures. Bony prominences are the most common sites and causes. There are many risk factors that contribute to the development of pressure ulcers.
How many stages are there in pressure ulcers?
Pressure ulcers are classified by stages as defined by the National Pressure Ulcer Advisory Panel (NPUAP). Originally there were four stages (I-IV) but in February 2007 these stages were revised and two more categories were added, deep tissue injury and unstageable. Pressure Ulcer Staging.
What is a slough in a wound?
Often include undermining and tunneling. Unstageable - Full thickness tissue loss in which the base of the ulcer is covered by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed.
What does a grade 2 pressure ulcer look like?
Grade 2. In Grade 2 pressure ulcers, some of the outer surface of the skin (the epidermis) or the deeper layer of skin (the dermis) is damaged, leading to skin loss [Figure 1b]. The ulcer looks like an open wound or a blister.
What are the characteristics of a grade 4 pressure ulcer?
The characteristics are: Full thickness skin loss with extensive destruction, tissue necrosis, or damage to muscle, bone, or supporting structures, for example, tendon or joint capsule.
What is split thickness skin grafting?
Split thickness skin grafting . When the ulcer is superficial and vital tissues such as bone, vessels, nerves or tendons are not exposed, and the ulcer is not copiously discharging, skin grafting is the first option for surgical treatment.
Why use a pneumatic ripple bed?
Owing to unique pressure redistributing properties, affordable cost, easy availability and effectiveness; pneumatic ripple beds are now most commonly used for pressure ulcer prevention worldwide.
What age group is most likely to have pressure ulcers?
Age is also a factor that the majority (approximately two-third) of pressure ulcers occur in old age people (60-80 years of age).[7] .
What is grade 3 skin loss?
Partial thickness skin loss involving epidermis, dermis or both, for example, abrasion, blister or shallow crater. Grade 3. In Grade 3 pressure ulcers, skin loss occurs throughout the entire thickness of the skin. The underlying tissue is also damaged, but the underlying muscle and bone are not damaged.
Can friction cause pressure ulcers?
Friction, along with pressure and shear, is also frequently cited as a cause of pressure ulcers.[14] . Friction can cause pressure ulcers both indirectly and directly. In the indirect sense, friction is necessary to generate the shearing forces.
How to treat a swollen ulcer?
The first step to treating an ulcer in this stage is to remove pressure from the area. Any added or excess pressure can cause the ulcer to break through the skin surface. If you are lying down, adjust your position or use pillows and blankets as extra padding.
What are the stages of a pressure ulcer?
hips. ankles. heels. If you develop a pressure ulcer, you may notice that they form in a series of four stages. These stages are based on how deep the sore is. In some severe cases, there are two kinds of pressure ulcers that cannot fit into one of the four stages: suspected deep pressure injury. unstageable sores.
Why is it hard to diagnose an unstageable ulcer?
Unstageable pressure ulcers are also hard to diagnose because the bottom of the sore is covered by slough or eschar. Your doctor can only determine how deep the wound is after clearing it out. The ulcer may be yellow, green, brown, or black from slough or eschar.
How long does it take for a skin ulcer to heal?
These foods help with skin health. If treated early, developing ulcers in stage one can heal in about three days.
How long does it take for a stage 4 pressure ulcer to heal?
Your doctor will likely recommend surgery. Recovery for this ulcer can take anywhere from three months to two years to completely heal.
What is the most serious ulcer?
Stage 4 ulcers are the most serious. These sores extend below the subcutaneous fat into your deep tissues like muscle, tendons, and ligaments. In more severe cases, they can extend as far down as the cartilage or bone. There is a high risk of infection at this stage. These sores can be extremely painful.
What is the second stage of ulcers?
Stage 2. In the second stage, you’ll likely experience some pain from the ulcer. The sore area of your skin has broken through the top layer and some of the layer below. The break typically creates a shallow, open wound and you may or may not notice any drainage from the site.
What is a stage 2 pressure ulcer?
Definition. Partial thickness skin loss involving the dermis. May present as an open blister or shallow crater without slough or bruising. Stage 2 pressure ulcers happen because of pressure: therefore, the term/description stage 2 pressure ulcer should not be used to describe skin tears, tape burns, maceration, excoriation.
What to cover blisters with?
For blisters: cover with protective non adherent dressing. For an open wound: apply thin film of wound gel (examples include saf-gel or Duo derm gel) and a thin hydrocolloid (Duo Derm Extra Thin) or foam dressing (PolyMem or Allevyn) (Also.
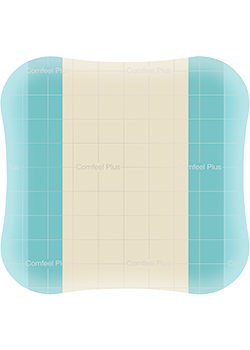
What is the best dressing for pressure ulcers?
An antimicrobial moist wound healing dressing, e.g.a silver foam (Biatain® Ag), or a silver alginate dressing (SeaSorb®Soft Ag) in combination with an adhesive secondary dressing(Biatain Silicone) may help prevent or resolve wound infection.
What is partial thickness loss of dermis?
Partial thickness loss of dermis presenting as a shallow open ulcer with a red-pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled or sero-sanginous filled blister.
What is the color of a slough in a wound?
Full thickness tissue loss in which actual depth of the ulcer is completely obscured by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed.
Can an alginate filler be used on a deep pressure ulcer?
Infected deep pressure ulcers or deep wounds at-risk of infection can be filled with antimicrobial dressing materials, such as an alginate filler, and covered with an adhesive dressing. If the infection spreadsbeyond the wound, antibiotics should be used at the discretion of aphysician.
What is a partial thickness burn?
Tweet. A partial thickness burn (also known as a second degree burn) is a burn that affects the top two layers of skin, called the epidermis and hypodermis. Partial thickness burns can continue to change over time and can evolve to a full thickness burn (or third degree burn), even after initial treatment.
How to treat a burn on the back of the head?
Do not use ice to cool the burn. Soak a clean cloth with cool water, wring out excess water, fold and apply to burn as a compress (to help relieve pain) Bandage the burn with a nonstick bandage or sterile cloth to protect from bacteria and foreign debris.
Is partial thickness burn serious?
Partial thickness burns are serious and have a high risk of developing infection or other complications.
What is a pressure ulcer?
A pressure ulcer is any lesion caused by unrelieved pressure resulting in damage of underlying tissue. Pressure ulcers usually occur over bony prominences ...
What is ulcer care?
Initial ulcer care involves debridement, wound cleansing, dressing application and possible adjunctive therapy. Debridement should be performed to remove moist, devitalized tissue. Small wounds can be debrided at bedside, while extensive wounds should be debrided in the operating room or special procedure room.
What stage of pressure ulcers are colonized?
According to clinical guidelines from the Agency for Healthcare Research and Quality (AHRQ), stage 2, 3 and 4 pressure ulcers should all be considered as colonized with bacteria. Proper wound cleansing and debridement should prevent bacterial colonization from proceeding to the point of clinical infection. Strategies to manage pressure ulcers and ...
Is pressure ulcers a negligence?
When the treatment and prevention of pressure ulcers comes under legal scrutiny, it is often alleged as negligence. According to the authors, the readily apparent nature of pressure ulcers means that, unlike many other medical complications, they never go unnoticed by patients and their families.