Surgery You'll likely need surgery to treat diverticulitis An inflammation or infection of the pouches formed in the colon (diverticula).Diverticulitis
When do you need surgery for diverticulitis?
Surgery for Diverticular Disease. Your NYU Langone gastroenterologist may recommend surgery if symptoms of diverticulitis haven’t improved after nonsurgical treatment; if a perforation or fistula, a connection that forms between the intestines and another organ, develops in the colon wall; or if a diverticular pouch ruptures.
What is the recovery time for Diverticulitis surgery?
The diverticulitis surgery recovery time depends upon the procedure, type of the surgery, and the overall health of the patient. In most cases, people recover within 1½ - 2 months of the procedure.
How is uncomplicated diverticulitis treated?
Uncomplicated diverticulitis. If your symptoms are mild, you may be treated at home. Your doctor is likely to recommend: Antibiotics to treat infection, although new guidelines state that in very mild cases, they may not be needed.
What is a two stage operation for diverticulitis?
Diverticulitis Surgery Recovery. A two-stage operation is usually required in case of emergencies. In a two-stage operation, first the diseased part of the colon is removed, after which the upper section of the colon is attached to an opening on the abdominal wall. This procedure is known as colostomy.

When is surgery needed for diverticulosis?
Surgery usually isn't necessary in people who have acute diverticulitis. But there are exceptions: If abscesses (collections of pus) have formed, and treatment with antibiotics isn't successful, surgery is unavoidable.
How do you know when you need surgery for diverticulitis?
Your doctor may recommend surgery if you have:multiple severe episodes of diverticulitis uncontrolled by medications and lifestyle changes.bleeding from your rectum.intense pain in your abdomen for a few days or more.constipation, diarrhea, or vomiting that lasts longer than a few days.More items...
Is there surgery for diverticulosis?
Surgery for diverticular disease can be performed by laparoscopic or minimally invasive techniques. Surgery involves removing part of the colon, usually the sigmoid colon, and reattaching it to the rectum.
How do I know if my diverticulitis is getting worse?
Symptoms of Diverticulitis This pain may get worse over several days and may vary in severity. In addition, nausea, vomiting, diarrhea and constipation are symptoms that may occur. In moderate to severe symptoms a person has more severe pain, can't keep any liquids down and may have a fever.
What is the standard treatment for diverticulitis?
Diverticulitis is treated using diet modifications, antibiotics, and possibly surgery. Mild diverticulitis infection may be treated with bed rest, stool softeners, a liquid diet, antibiotics to fight the infection, and possibly antispasmodic drugs.
What is the main cause of diverticulosis?
Doctors believe the main cause is a low-fiber diet. Most people with diverticulosis don't have symptoms. Sometimes it causes mild cramps, bloating or constipation. Diverticulosis is often found through tests ordered for something else.
How successful is surgery for diverticulitis?
About 15%-25% of patients who present with a first episode of acute diverticulitis have disease severe enough to require surgery. Up to 22% of those who have surgery will have a future attack.
Can diverticula be removed during colonoscopy?
A polyp found during colonoscopy in patients with colonic diverticular disease may be removed by endoscopic polypectomy with electrosurgical snare, a procedure associated with an incidence of perforation of less than 0.05%.
What is the procedure to remove a diverticulitis colon?
If you’ve had two or three episodes of diverticulitis, your doctor may recommend an elective procedure called sigmoidectomy, in which the affected part of the colon—called the sigmoid colon—is removed to help prevent a recurrence.
What is the procedure called when you have a colon removed?
If you need emergency surgery, your doctor may perform a surgery called Hartmann’s procedure, in which he or she removes the diseased portion of the colon and cleans out any infected areas in the abdominal cavity. This procedure requires general anesthesia. It can be done using laparoscopy or an open technique.
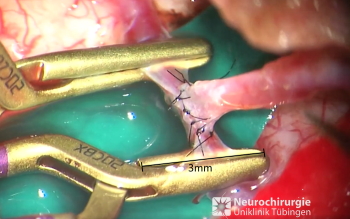
What is laparoscopic surgery?
During a laparoscopic procedure, the surgeon makes several very small incisions in the abdomen, through which the laparoscopic instruments are inserted. He or she performs the surgery with the help of a two-dimensional image on a video monitor.
How are surgical instruments and cameras inserted?
The surgical tools and camera are inserted through tiny incisions in the abdomen. The surgeon controls these instruments and the camera from a console. In both approaches, the abdomen is inflated with gas, which expands the abdominal cavity, giving the surgeon a better view and more freedom of movement.
How long does it take to go to the hospital after a sigmoidectomy?
A typical hospital stay after an elective sigmoidectomy is two to four days. After the procedure, you are given liquids and your doctor waits for you to have a bowel movement. After a period of observation, you are allowed to start eating solid foods and go home.
Can colorectal surgery be performed as an elective procedure?
Colorectal surgery can also be performed as an elective procedure to prevent recurrent episodes of diverticulitis. Your doctor can explain the benefits and risks of this option. Elective surgery is usually a minimally invasive procedure, and surgeons use either traditional laparoscopy or robotic-assisted laparoscopy.
Can you have diverticulitis surgery?
Your NYU Langone gastroenterologist may recommend surgery if symptoms of diverticulitis haven’t improved after nonsurgical treatment; if a perforation or fistula, a connection that forms between the intestines and another organ, develops in the colon wall; or if a diverticular pouch ruptures. These problems can cause stool or infected material to leak into the abdominal cavity, increasing the risk that the infection spreads to the abdominal cavity or elsewhere in the body.
Why do you need diverticulitis surgery?
You can usually manage your diverticulitis by doing the following: taking prescribed antibiotics.
How to treat diverticulitis?
taking prescribed antibiotics. using nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil) drinking fluids and avoiding solid food until your symptoms go away. Your doctor may recommend surgery if you have: multiple severe episodes of diverticulitis uncontrolled by medications and lifestyle changes.
What is the procedure called when a colon is removed?
Bowel resection with primary anastomosis: In this procedure, your surgeon removes any infected colon (known as a colectomy) and sews together the cut ends of the two healthy pieces from either side of the previously infected area (anastomosis). Bowel resection with colostomy : For this procedure, your surgeon performs a colectomy ...
What is diverticulitis in the colon?
What is diverticulitis? Diverticulitis happens when small pouches in your digestive tract , known as diverticula, become inflamed. Diverticula often become inflamed when they get infected. Diverticula are usually found in your colon, the largest section of your large intestine.
What are the risks of having diverticulitis surgery?
As with any surgery, your risk of complications may be increased if you: are obese. are over the age of 60. have other significant medical conditions such as diabetes or high blood pressure. have had diverticulitis surgery or other abdominal surgery before. are in overall poor health or not getting enough nutrition.
What are the symptoms of diverticulitis?
multiple severe episodes of diverticulitis uncontrolled by medications and lifestyle changes. bleeding from your rectum. intense pain in your abdomen for a few days or more. constipation, diarrhea, or vomiting that lasts longer than a few days. blockage in your colon keeping you from passing waste (bowel obstruction)
How many small openings do you need for bowel resection?
To perform a bowel resection with primary anastomosis, your surgeon will: Cut three to five small openings in your abdomen (for laparoscopy) or make a six- to eight-inch opening to view your intestine and other organs (for open surgery). Insert a laparoscope and other surgical tools through the cuts (for laparoscopy).
What does a doctor take into consideration when suggesting a type of diverticulitis surgery?
A doctor will take a person’s health, risk factors, and other symptoms into consideration when suggesting a type. In this article, we describe the types of diverticulitis surgery, including the procedures involved, possible complications, and recovery.
What to do before diverticulitis surgery?
Before a person undergoes surgery, a doctor may prescribe antibiotics to reduce the risk of infection. Before undergoing diverticulitis surgery, it is important to discuss the risks and benefits of each procedure with a doctor. It may also be helpful to get a second opinion. Before surgery:
What is the most common type of surgery for diverticulitis?
Colon resection. This is the most common type of surgery for diverticulitis. A surgeon cuts into the colon, removes the damaged pockets or pouches, then reattaches the remaining segments of the colon. The surgeon may reattach the colon to the rectum or create a colostomy.
Can diverticulitis be a symptom of another attack?
Anyone with diverticulitis may have another attack, even after surgery. It is possible to reduce the risk by eating a diet high in fiber, and by taking probiotics and drugs such as mesalamine.
Can diverticulitis be treated with antibiotics?
In many cases, lifestyle changes and antibiotics can treat symptoms and reduce the risk of future attacks. If diverticulitis does not cause symptoms, or if symptoms go away on their own, surgery is not usually recommended.
Can laparoscopic washouts kill colon infection?
However, because laparoscopic washout involves leaving the damaged portion of the colon in the body, the risk of future attacks is increased .
Can diverticulitis surgery be done with a liquid diet?
Infection may lead to a longer recovery or additional surgery. It may also be necessary to have a liquid diet or eat foods rich in fiber . The success of diverticulitis surgery depends on many factors, including the health of the colon, the person’s age and general health, and the skill of the surgeon.
What is the best treatment for diverticulitis?
Simple diverticulitis, a minor infection of the colon, is treated with bowel rest and antibiotics. Your doctor also will recommend changes in your diet that include an increase in fiber-rich foods, such as whole grains, beans, vegetables, and fruit.
How to recover from a diverticular resection?
Recovery. Following resection surgery, you should try to eat a nutritious diet and walk daily for exercise. A positive attitude can also help speed recovery. To prevent further diverticular issues, we recommend NOT eating popcorn, increasing water intake, and following a healthy diet that includes fiber-rich foods.
How many people have diverticulitis?
Diverticulitis affects 10% of people over age 40 and 50% of people over age 60. It can begin with mild symptoms like cramps or bloating, which are easily mistakable for other minor problems and alleviated by mild pain relievers. But it can evolve into a serious condition accompanied by fever, infection, nausea, vomiting, and constipation.
Is colon surgery invasive?
However, Dr. Meslin explains that by using minimally invasive techniques , risks are significantly reduced.
Can a recurrent colon attack cause bowel problems?
Recurrent attacks can lead to an increased risk of perforation and difficulty with bowel function due to chronic scarring and narrowing of the colon. Under these conditions, elective resection is recommended.
Can diverticulitis be drained?
Complicated diverticulitis with an abscess (infected, pus-filled area) or peritonitis (inflammation of the abdominal lining) results when a perforation, or hole, forms in the colon. An abscess often can be drained with the help of a radiologist using imaging technology.
How long does it take to recover from diverticulitis surgery?
In general, it can take about 3 to 4 weeks to return to work or resume the normal activities, after an open diverticulitis surgery. But, in case of laparoscopic surgery, you can expect to resume your normal activities within 1 to 2 weeks.
How to treat diverticulitis?
If diagnosed in the early stages, it can be treated with medications, by following a proper diverticulitis diet, and making lifestyle changes. However, surgery becomes a necessity for patients with chronic ailments and those who are non-responsive to medications and diet. The diverticulitis surgery recovery time varies with respect ...
How is diverticulitis removed?
During a conventional diverticulitis surgery, the affected part of the sigmoid colon is removed after making an incision in the abdomen. This procedure is known as partial colectomy, which may be done in one step, or it may require a two-stage operation. A two-stage operation is usually required in case of emergencies.
How common is diverticulitis surgery?
As the episodes of diverticulitis attacks become more frequent when one grows older, diverticulitis surgery is more common in people above 40 years.
How long does it take to go to the hospital after a partial colectomy?
The hospital stay can be substantially longer, if partial colectomy is done in two stages. The time between the two operation is usually 6 to 12 weeks. On the other hand, in laparoscopic surgery, the hospital stay time is less, usually 4 to 5 days.
What is the procedure called when the colon is attached to the abdominal wall?
This procedure is known as colostomy.
How are stool removed from the body?
Stools are eliminated from the body through this opening into a disposable bag. The next stage of the operation involves reconnecting the two ends of colon. In recent times, a less invasive laparoscopy method is followed, for removing the diseased part of the colon and reconnecting the healthy parts.
