
What is the best and safest treatment for osteoporosis?
Aug 17, 2020 · Detect low bone density before osteoporosis develops. Help predict your risk of future fractures. Monitor the effectiveness of ongoing treatment for osteoporosis. The most common test for measuring bone mineral density is dual-energy x-ray absorptiometry (DXA). It is a quick, painless, and noninvasive test.
How to naturally treat osteoporosis?
For women with osteoporosis who are at least 65 years of age and have a high risk for fracture, treatment decisions should be individualized; risk versus benefit, patient preferences, fracture-risk profile, and costs should be assessed to determine if osteoporotic treatment is warranted.
What is the first line treatment for osteoporosis?
Dec 31, 2013 · The aim of osteoporosis treatment is to prevent fragility fractures. Pharmacological treatment for osteoporosis is only indicated when the fracture risk is considered unacceptably high , such that treatment benefits overwhelmingly exceed the risks. Pharmacological treatment should be continued while the fracture risk is high.
What are the early signs of osteoporosis?
Jun 26, 2017 · Treating osteoporosis means stopping the bone loss and rebuilding bone to prevent breaks. Healthy lifestyle choices such as proper diet, exercise, and medications can help prevent further bone loss and reduce the risk of fractures. But, lifestyle changes may not be enough if you have lost a lot of bone density.

What is the first line treatment of osteoporosis?
Bisphosphonates should be used as first-line pharmacologic treatment for osteoporosis. In patients who cannot tolerate or whose symptoms do not improve with bisphosphonate therapy, teriparatide (Forteo) and denosumab (Prolia) are effective alternative medications to prevent osteoporotic fractures.Aug 15, 2015
Does osteoporosis need to be treated?
There's no cure for osteoporosis, but proper treatment can help protect and strengthen your bones. These treatments can help slow the breakdown of bone in your body, and some treatments can spur the growth of new bone.
What is the fastest way to increase bone density?
10 Natural Ways to Build Healthy BonesEat Lots of Vegetables. ... Perform Strength Training and Weight-Bearing Exercises. ... Consume Enough Protein. ... Eat High-Calcium Foods Throughout the Day. ... Get Plenty of Vitamin D and Vitamin K. ... Avoid Very Low-Calorie Diets. ... Consider Taking a Collagen Supplement. ... Maintain a Stable, Healthy Weight.More items...•Jan 18, 2017
What not to do if you have osteoporosis?
With low bone density or osteoporosis, you should avoid:Rounding poses or rounded spine movements.Spine twist or any deep twists.Corkscrew or bicycle.Deep hip stretches (like the pigeon pose)Warrior pose.Overpressure from teachers.Nov 26, 2019
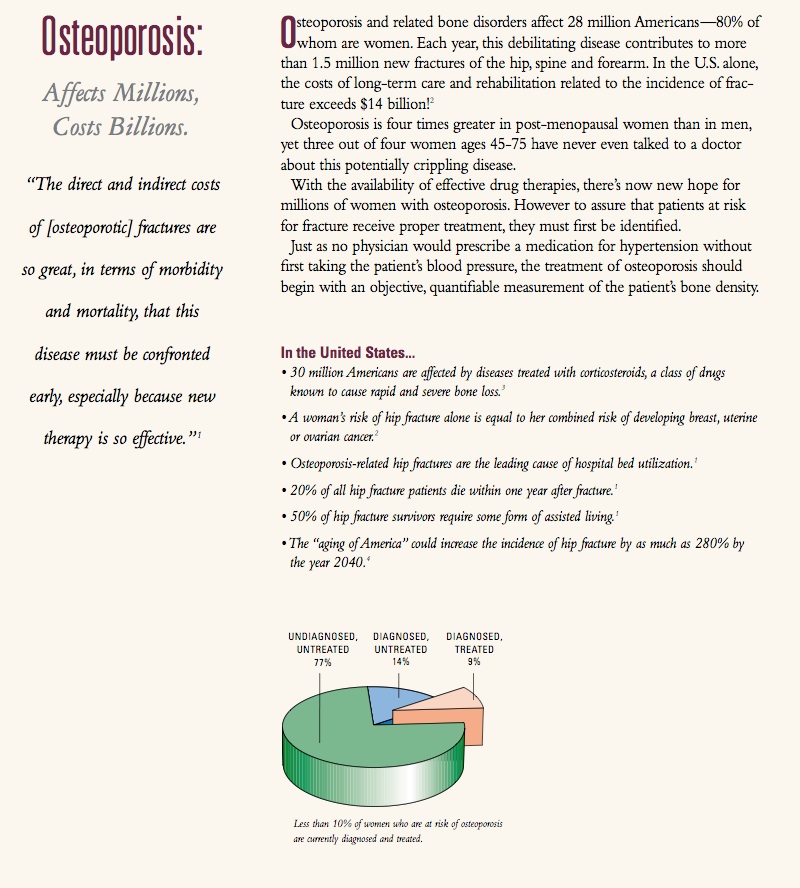
Abstract
Approximately 10 million men and women in the U.S. have osteoporosis, 1 a metabolic bone disease characterized by low bone density and deterioration of bone architecture that increase the risk of fractures. 2 Osteoporosis-related fractures can increase pain, disability, nursing home placement, total health care costs, and mortality.
INTRODUCTION
Osteoporosis is a bone disorder that increases a person’s risk of fracture due to low bone mineral density (BMD), impaired bone microarchitecture/mineralization, and/or decreased bone strength.
PATHOPHYSIOLOGY
Bones provide structure for the body, protection for the organs, and storage for minerals, such as calcium and phosphorus, that are essential for bone development and stability. Individuals continue to build bone and will reach peak bone mass at about 30 years of age, after which they begin to lose bone mass steadily.
ETIOLOGY
Primary osteoporosis is often associated with age and sex hormone deficiency. Age-related osteoporosis results from the continuous deterioration of the trabeculae in bone. In addition, the reduction of estrogen production in post menopausal women causes a significant increase in bone loss.
SCREENING AND DIAGNOSIS
Published osteoporosis screening guidelines vary greatly. In general, most organizations recommend that all adults older than 50 years of age with a history of fracture receive BMD screening.
SELECT GUIDELINES AND RECOMMENDATIONS
In a systematic review, Solomon et al. looked at 18 osteoporosis guidelines, among them those of the NOF, the ACR, and the American Association of Clinical Endocrinologists and American College of Endocrinology (AACE/ACE).
NONPHARMACOLOGICAL MANAGEMENT
Nonpharmacological management of osteoporosis includes adequate calcium and vitamin D intake, weight-bearing exercise, smoking cessation, limitation of alcohol/caffeine consumption, and fall-prevention techniques. 2 – 6, 9, 18, 34
How to prevent osteoporosis?
17 The USPSTF recommends exercise or physical therapy and vitamin D supplementation to prevent falls in community-dwelling adults 65 years or older who are at increased risk of falls. 18 A multicomponent exercise program that consists of weight-bearing resistance and balance training should be recommended. Aerobic exercise programs that do not incorporate strength and balance training should be avoided because of the association with increased fracture risk. 19 A thorough assessment of a patient's risks of falling and mitigation of those risk factors have strong evidence of effectiveness in fall prevention. 20 A Cochrane review suggested that hip protectors decrease fracture risk. 21
What is osteoporosis based on?
Osteoporosis is diagnosed radiographically based on bone mineral density (BMD) determinations from dual energy x-ray absorptiometry (DEXA) assessment. 4 Although quantitative calcaneal ultrasonography and peripheral DEXA can also predict fracture risk, these modalities do not correlate well enough with central DEXA to be used diagnostically. 1, 5, 6 The World Health Organization (WHO) established commonly accepted definitions of osteoporosis and osteopenia 4 ( Table 3 6).
What is secondary osteoporosis?
Primary osteoporosis is related to aging and loss of gonadal function. Secondary osteoporosis is caused by other health conditions ( Table 4). 2 Up to 30% of osteoporosis cases in postmenopausal women are estimated to be from a secondary cause. 10 The estimate climbs to greater than 50% in men, premenopausal women, and perimenopausal women if vitamin D deficiency is included as a secondary cause. 11 – 13 In addition to performing a history and physical examination, expert consensus suggests a basic laboratory evaluation for all newly diagnosed patients to determine if there are contraindications for certain osteoporosis medications and to identify the more common secondary causes. The most commonly recommended laboratory tests include serum 25-hydroxyvitamin D, calcium, creatinine, and thyroid-stimulating hormone levels. 1, 14
How long does it take to stop bisphosphonate therapy?
Clinicians should consider discontinuing bisphosphonate therapy after five years in women without a personal history of vertebral fractures.
How many white women have osteoporosis?
Osteoporosis-related fractures affect approximately one in two white women and one in five white men in their lifetime. The impact of fractures includes loss of function, significant costs, and increased mortality.
How many Americans have osteoporosis of the hip?
Statistics. Disability (pain, disability, complications) 10 million Americans 50 years and older have osteoporosis of the hip. 1.5 million Americans have osteoporotic fracture (40% of women and 10% of men will have a fracture of the hip, spine, or wrist) 40% regain prefracture independence.
How to contact the National Osteoporosis Foundation?
301-565-2966 (TTY ) [email protected]. www.niams.nih.gov. National Osteoporosis Foundation. 800-231-4222 (toll-free) [email protected]. www.nof.org. This content is provided by the NIH National Institute on Aging (NIA). NIA scientists and other experts review this content to ensure it is accurate and up to date.
What are some exercises to help with osteoporosis?
So is regular weight-bearing exercise, such as weight training, walking, hiking, jogging, climbing stairs, tennis, and dancing . If you have osteoporosis, avoid activities that involve twisting your spine or bending forward from the waist, such as conventional sit-ups, toe touches, or swinging a golf club.
What is a bone mineral density test?
A bone mineral density test compares your bone density to the bones of an average healthy young adult. The test result, known as a T-score, tells you how strong your bones are, whether you have osteoporosis or osteopenia, and your risk for having a fracture.
Why is osteoporosis considered a silent disease?
Osteoporosis is called a “silent disease” because you may not notice any changes until a bone breaks. All the while, though, your bones had been losing strength for many years. Bone is living tissue. To keep bones strong, your body breaks down old bone and replaces it with new bone tissue.
What happens to the bones in your 40s?
As people enter their 40s and 50s, more bone may be broken down than is replaced. A close look at the inside of bone shows something like a honeycomb. When you have osteoporosis, the spaces in this honeycomb grow larger, and the bone that forms the honeycomb gets smaller. The outer shell of your bones also gets thinner.
How do you know if you have osteoporosis?
For some people, the first sign of osteoporosis is to realize they are getting shorter or to break a bone easily. Don’t wait until that happens to see if you have osteoporosis. You can have a bone density test to find out how strong your bones are.
How to keep bones strong?
To keep bones strong, your body breaks down old bone and replaces it with new bone tissue. Sometime around age 30, bone mass stops increasing, and the goal for bone health is to keep as much bone as possible for as long as you can. As people enter their 40s and 50s, more bone may be broken down than is replaced.
Treatment of Low Bone Density or Osteoporosis
The guideline, Treatment of Low Bone Density or Osteoporosis to Prevent Fractures in Men and Women, was developed by the American College of Physicians and was endorsed by the American Academy of Family Physicians.
Key Recommendations
Pharmacologic treatment with alendronate, risedronate, zoledronic acid, or denosumab should be prescribed for women with osteoporosis to reduce the risk of hip and vertebral fractures.
How common is osteoporosis in older people?
Osteoporosis is most common in older people, especially (but not only) in women. In many cases, it is first revealed by a sudden fracture — and by the time that happens, it is too late to go back and prevent this dreadful event, which can lead to many complications. According to an article published in the Journal of the American Medical Association, each year Americans suffer from 1.5 million osteoporotic fractures, resulting in more than 432,000 hospital admissions, almost 2.5 million medical office visits, and about 180,000 nursing home admissions. Medicare currently pays for approximately 80% of these fractures, with hip fractures accounting for 72% of the total cost. And because people are living longer (and are therefore more likely to get osteoporosis), the cost of osteoporosis care is expected to rise to $25.3 billion by 2025.
How long after a fracture can you get a bone mineral density test?
Despite the availability of cost-effective and well-tolerated treatments that can reduce fracture risk, only 23% of women ages 67 or older who have an osteoporosis-related fracture receive either a bone mineral density test or a prescription for an osteoporosis drug in the six months after the fracture.
Why do women question the need for treatment?
Because osteoporosis is a silent disease until a fracture occurs, women often question the need for treatment at all. There are guidelines and tools designed to help you and your doctor decide whether to start treatment, and as a patient, you have the right to know every detail of the treatment options being offered.
What happens when osteoblasts die?
Since the osteoclasts are dead, the osteoblasts just keep laying down bone. Bisphosphonates increases the bone density to a point where capillaries get smaller and smaller, eventually closing them off and then blood can’t get to the periosteum and whatever class of tissue is on top of the periosteum.
How much does Medicare pay for hip fractures?
Medicare currently pays for approximately 80% of these fractures, with hip fractures accounting for 72% of the total cost. And because people are living longer (and are therefore more likely to get osteoporosis), the cost of osteoporosis care is expected to rise to $25.3 billion by 2025.
Why is modern medicine important?
Because many people are living longer these days, one of the biggest responsibilities of modern medicine is to provide care and treatment for those diseases that become more common with increasing age. One of those diseases is osteoporosis, a thinning and weakening of the bones, which means they break more easily.
Can you take bisphosphonate by mouth?
Most often, it is associated with bisphosphonates given intravenously, not taken by mouth (as most bisphosphonates are). Certain population groups are also at higher risk for necrosis than others. Talk to your doctor about your personal risk for serious bisphosphonate side effects.
Prevention
- Your bone density can be measured by a machine that uses low levels of X-rays to determine the proportion of mineral in your bones. During this painless test, you lie on a padded table as a scanner passes over your body. In most cases, only certain bones are checked — usually in the h…
Diagnosis
Cause
Treatment
Prognosis
Medical uses
- Osteoporosis is diagnosed radiographically based on bone mineral density (BMD) determinations from dual energy x-ray absorptiometry (DEXA) assessment.4 Although quantitative calcaneal ultrasonography and peripheral DEXA can also predict fracture risk, these modalities do not correlate well enough with central DEXA to be used diagnostically.1,5,6 The World Health Organi…
Pharmacology
- Primary osteoporosis is related to aging and loss of gonadal function. Secondary osteoporosis is caused by other health conditions (Table 4).2 Up to 30% of osteoporosis cases in postmenopausal women are estimated to be from a secondary cause.10 The estimate climbs to greater than 50% in men, premenopausal women, and perimenopausal women if vitamin D defici…
Research
- The National Osteoporosis Foundation recommends treatment of postmenopausal women and men with a personal history of hip or vertebral fracture, a T-score of 2.5 or less, or a combination of low bone mass (T-score between 1 and 2.5) and a 10-year probability of hip fracture of at least 3% or any major fracture of at least 20% as calculated by the FR...
Resources
- The optimal length of oral bisphosphonate therapy is unknown. One study found that women who take alendronate for five years followed by five years of placebo have no increased incidence of nonvertebral or hip fractures compared with women who take alendronate for 10 years. There is, however, an increase in vertebral fractures.38 Osteonecrosis of the jaw and atypical femoral fra…