Full Answer
When should I go to the ER for septic shock?
If you develop any of the symptoms, call 911 or get to the emergency room ASAP. While septic shock can be a scary diagnosis, immediate treatment is important and could save your life. If you have experienced septic shock, make sure to see your healthcare provider regularly for follow-up visits.
What is septic shock and how is it treated?
Septic shock is when you experience a significant drop in blood pressure that can lead to respiratory or heart failure, stroke, failure of other organs, and death.
What is the prognosis of septic shock?
Introduction Septic shock, which is characterized by severe hemodynamic failure, remains a major challenge associated with 30% to 40% hospital mortality, even though important therapeutic advances have been made over the past decades (1).
How are antibiotics administered for sepsis/septic shock?
The antibiotics are administered intravenously (IV). After learning the results of blood tests, your doctor may switch to a different antibiotic that's targeted to fight the particular bacteria causing the infection. Intravenous fluids. People who have sepsis often receive intravenous fluids right away, usually within three hours. Vasopressors.

How soon after making the diagnosis of sepsis should treatment start?
Treatment for sepsis You should get antibiotics within 1 hour of arriving at hospital. If sepsis is not treated early, it can turn into septic shock and cause your organs to fail. This is life threatening.
Which treatment should begin immediately in the diagnosis of septic shock?
Fluid resuscitation is the initial treatment for hypotension in patients with septic shock. Vasopressor therapy should be initiated in patients with sepsis when fluid resuscitation fails to restore mean arterial pressure (greater than 65 mm Hg) or continued organ hypoperfusion.
How soon should fluid resuscitation begin with septic shock?
Rapid initiation of resuscitation – Resuscitation should be initiated within 15 minutes of confirming severe sepsis or septic shock.
What is the priority in treating septic shock?
The first priority is early recognition. The earliest recognizable clinical presentation is fever and hyperventilation. The second priority is augmenting normal compensatory mechanisms by intravenous infusion of crystalloid, with measurement of the response so that vasoactive drugs can be instituted as needed.
What should be done after identifying a patient with possible severe sepsis or septic shock?
Antimicrobial therapy IV antibiotic therapy should be initiated within the first hour after the recognition of septic shock or sepsis; delays in administration are associated with increased mortality.
What is the gold standard for sepsis?
There is no 'gold standard' against which the diagnostic criteria can be calibrated.” In 2004 the Surviving Sepsis Campaign released its initial guidelines for sepsis management in the journals of Critical Care Medicine and Intensive Care Medicine.
What is the sepsis protocol?
What are Sepsis Protocols? A protocol in a medical context refers to a set of rules or a specific plan that doctors and nurses must follow during treatment. Sepsis protocols describe the treatment guidelines that clinicians must follow when assessing and treating patients with sepsis.
What amount of fluid resuscitation would a patient require for severe sepsis?
30 mL/kg of intravenous crystalloid fluid within the first three hours. Fluids should be administered for hypotension, lactate ≥ 4 mmol/L or septic shock. The recommendation is to provide initial fluid resuscitation rapidly; do not infuse using an IV pump.
What is the appropriate first line treatment for shock?
In general, fluid resuscitation (giving a large amount of fluid to raise blood pressure quickly) with an IV in the ambulance or emergency room is the first-line treatment for all types of shock.
When septic shock is suspected Which of the following is the highest priority in the first 1 hour?
Consensus guidelines recommend antibiotic therapy within one hour of suspected sepsis. In septic shock, the initiation of antibiotic therapy within one hour increases survival; with each hour antibiotic therapy is delayed, survival decreases by about 8%.
When does the time zero clock begin for sepsis and septic shock?
NOTE: SEP-1 has two “time zeros.” All cases have a severe sepsis time zero requiring completion of the bundle within three hours. If criteria for shock is met within six hours of severe sepsis presentation, a second septic shock time zero is started requiring the shock bundle elements be completed within six hours.
When should vasopressors be administered during the management of septic shock?
The guidelines recommend a mean arterial pressure (MAP) of at least 65 mmHg should be used as an initial target value [8] and that vasopressors should be started immediately if patients remain hypotensive during or after fluid resuscitation (strong recommendation, moderate quality of evidence) [9].
How to treat septic shock?
A number of medications are used in treating sepsis and septic shock. They include: 1 Antibiotics. Treatment with antibiotics begins as soon as possible. Broad-spectrum antibiotics, which are effective against a variety of bacteria, are usually used first. After learning the results of blood tests, your doctor may switch to a different antibiotic that's targeted to fight the particular bacteria causing the infection. 2 Intravenous fluids. The use of intravenous fluids begins as soon as possible. 3 Vasopressors. If your blood pressure remains too low even after receiving intravenous fluids, you may be given a vasopressor medication. This drug constricts blood vessels and helps increase blood pressure.
What is the best treatment for sepsis?
Supportive care. People who have sepsis often receive supportive care that includes oxygen. Depending on your condition, you may need to have a machine help you breathe. If your kidneys have been affected, you may need to have dialysis.
What tests can be done to determine if you have an infection in your lungs?
If the site of infection is not readily found, your doctor may order one or more of the following imaging tests: X-ray. X-rays can identify infections in your lungs. Ultrasound. This technology uses sound waves to produce real-time images on a video monitor.
When Sepsis Becomes Septic Shock
Sepsis treatment usually requires intravenous (IV) fluids and antibiotics. It is essential that the treatment begin as early as possible. The chance of sepsis progressing to severe sepsis and septic shock, causing death, rises by 4% to 9% for every hour treatment is delayed.
Why Septic Shock Is Dangerous
As your heart pumps blood throughout your body, it produces a certain amount of pressure to help push the blood through the blood vessels. The blood then delivers oxygen and nutrients to the organs and other body tissues. It also removes toxins. The average blood pressure for a healthy adult is less than or around 120/80 mmHg.
Septic Shock Complications
One of the most serious septic shock complications is organ damage. In some cases, the damage may only be temporary. For example, a person in septic shock may develop acute kidney injury. The kidneys are not able to filter out the toxins from the blood.
Septic Shock Treatment
Treating septic shock focuses on increasing the blood pressure, eliminating the infection that triggered the sepsis, and providing support for the organs that are failing. Some treatments could include:
After Septic Shock
Most often, you can be discharged from the ICU once your blood pressure is stable and supportive treatment, like a ventilator or dialysis, are no longer required. You will still be monitored and cared for, but in a lower-acuity ward or unit.
How long does it take for a doctor to treat septic shock?
Doctors use the following medications to treat sepsis and septic shock: Antibiotics: Treatment should begin within the first 6 hours after diagnosis. The doctor will administer these drugs directly into a vein.
How to reduce the risk of septic shock?
There are a few steps that people can take to reduce their risk of developing sepsis and septic shock: Get regular vaccinations against viral infections, such as flu, pneumonia, chickenpox, HIV, and other infections that could potentially lead to sepsis.
What is septic shock?
Takeaway. Septic shock is a severe and potentially fatal condition that occurs when sepsis leads to life-threatening low blood pressure. Sepsis develops when the body has an overwhelming response to infection. Knowing how to recognize and prevent septic shock is vital. The body usually responds to an infection by releasing inflammatory substances ...
What is the best medication for septic shock?
Vasopressors: These medications are necessary to maintain adequate blood pressure in people with septic shock. A doctor will use these if blood pressure remains too low after a person receives fluids. Vasopressors work by tightening the blood vessels to increase blood pressure.
How does the body respond to septic shock?
Knowing how to recognize and prevent septic shock is vital. The body usually responds to an infection by releasing inflammatory substances into the bloodstream. These regulate the immune system to fight the infection. When the body loses control of this response, it triggers damaging changes to the organs.
What tests can be done to confirm sepsis?
Tests that may help a doctor confirm sepsis and septic shock include: Blood cultures: A doctor will draw samples of blood from two different sites in the body and test them for signs of infection. Urine tests: If the doctor suspects a UTI, they may ask for a urine sample to check for bacteria and infection.
How to keep infection at bay?
Washing the hands frequently, especially after handling food, touching pets, and using bathroom facilities, is another way to keep infection at bay. Care for and clean any open or gaping wounds. Wear disposable gloves, and rinse wounds with clean, soap-free water to clear out debris or dirt.
What is the best solution for septic shock?
Crystalloid solutions (isotonic saline or balanced crystalloids) are recommended for volume resuscitation in sepsis and septic shock. The best one to use is still debated, but over the last decade, balanced solutions have come to be favored for critically ill patients. Growing evidence indicates that balanced crystalloids (lactated Ringer solution, Plasma-Lyte) are associated with a lower incidence of renal injury, less need for renal replacement therapy, and lower mortality in critically ill patients. Moreover, isotonic saline is associated with hyperchloremia and metabolic acidosis, and it can reduce renal cortical blood flow. 40 – 42
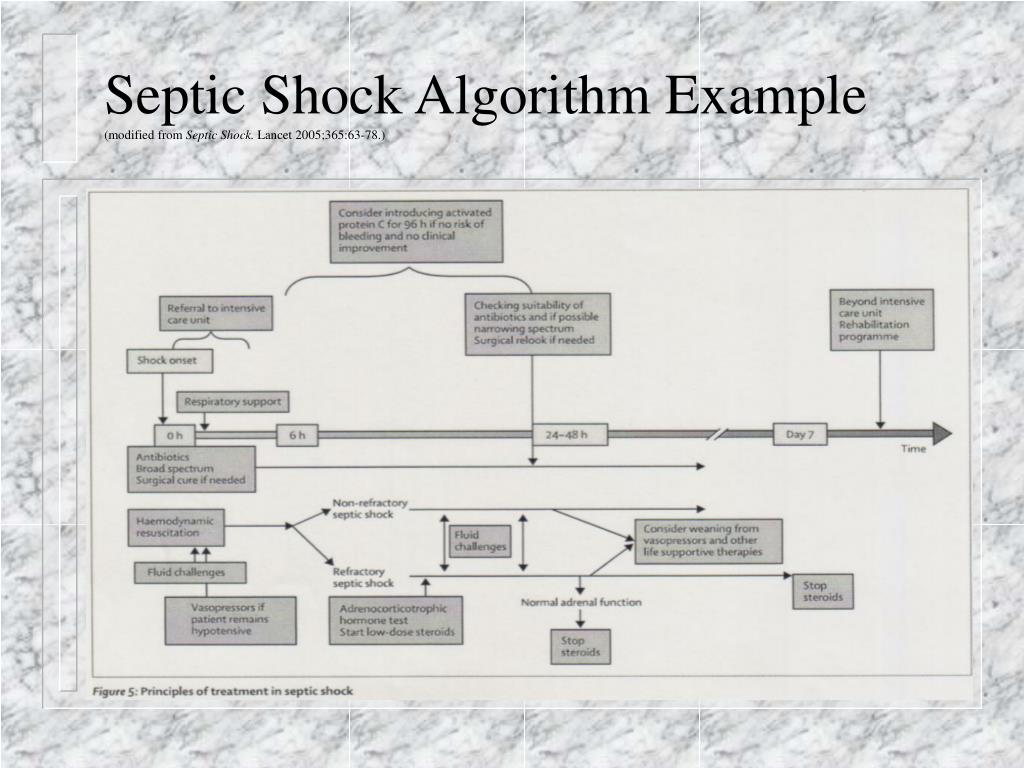
How long does it take for a septic system to stabilize?
Stabilization: During the third phase, usually 24 to 48 hours after the onset of septic shock, an attempt should be made to achieve a net-neutral or a slightly negative fluid balance. De-escalation: The fourth phase, marked by shock resolution and organ recovery, should trigger aggressive fluid removal strategies. 27.
What is the role of antibiotics in sepsis?
Sepsis is a life-threatening organ dysfunction that results from the body’s response to infection. It requires prompt recognition, appropriate antibiotics, careful hemodynamic support, and control of the source of infection. With the trend in management moving away from protocolized care in favor of appropriate usual care, an understanding of sepsis physiology and best practice guidelines is critical.
What are the effects of sepsis on the body?
Sepsis is associated with vasodilation, capillary leak, and decreased effective circulating blood volume, reducing venous return. These hemodynamic effects lead to impaired tissue perfusion and organ dysfunction. The goals of resuscitation in sepsis and septic shock are to restore intravascular volume, increase oxygen delivery to tissues, and reverse organ dysfunction.
How many people die from sepsis in the US?
Sepsis affects 750,000 patients each year in the United States and is the leading cause of death in critically ill patients, killing more than 210,000 people every year. 1 About 15% of patients with sepsis go into septic shock, which accounts for about 10% of admissions to intensive care units (ICUs) and has a death rate of more than 50%.
What is severe sepsis?
Severe sepsis was defined as the progression of sepsis to organ dysfunction, tissue hypoperfusion, or hypotension. Septic shock was described as hypotension and organ dysfunction that persisted despite volume resuscitation, necessitating vasoactive medication, and with 2 or more of the SIRS criteria listed above.
When was sepsis first defined?
In 1991, sepsis was first defined as a systemic inflammatory response syndrome (SIRS) due to a suspected or confirmed infection with 2 or more of the following criteria 4 :