- You have a complication, such as a bowel abscess, fistula or obstruction, or a puncture (perforation) in the bowel wall.
- You have had multiple episodes of uncomplicated diverticulitis.
- You have a weakened immune system.
When should I go to the hospital for a diverticulitis flare up?
That's why you should go to an emergency room immediately if you have any of the following symptoms: Excessive vomiting and severe nausea. Fever of more than 100 degrees — with or without chills. Loss or sudden change in appetite.20 Feb 2020
How do you know if diverticulitis is serious?
Symptoms of diverticulitis tend to be more serious and include:more severe abdominal pain, especially on the left side.high temperature (fever) of 38C (100.4F) or above.diarrhoea or frequent bowel movements.14 Feb 2020
Do I need to go to the doctor for a diverticulitis flare up?
Symptoms of a diverticulitis flare-up. If you think that you may have diverticulitis, or if you've been diagnosed before and you think that you're having a flare-up, call or see your doctor.21 Jul 2021
How long does diverticulitis flare up lasts?
“We usually see improvement within the first 24 hours, then considerable improvement within three to five days, and then the disease resolves in about 10 days.”6 Mar 2018
What does diverticulitis poop look like?
Diverticulitis stool characteristics Color: The stool may be bright red, maroon, or black and tarry, which indicates the presence of blood. Stools may contain more mucus than normal.
What can be mistaken for diverticulitis?
Common alternative conditions that can clinically mimic diverticulitis include small bowel obstruction, primary epiploic appendagitis, acute cholecystitis, appendicitis, ileitis, ovarian cystic disease, and ureteral stone disease.
What happens if diverticulitis goes untreated?
If left untreated, diverticulitis may lead to a collection of pus (called an abscess) outside the colon wall or a generalized infection in the lining of the abdominal cavity, a condition referred to as peritonitis.
Why do you need bed rest with diverticulitis?
An attack of diverticulitis without complications may respond to antibiotics within a few days if treated early. To help the colon rest, the doctor may recommend bed rest and a liquid diet, along with a pain reliever. An acute attack with severe pain or severe infection may require a hospital stay.
Can you have diverticulitis without a fever?
The patients with “atypical diverticulitis” present primarily with pain and may report alterations in bowel habits, though without fever, leukocytosis, or radiological signs of diverticulitis.18 Aug 2016
Will diverticulitis heal on its own?
In about 95 out of 100 people, uncomplicated diverticulitis goes away on its own within a week. In about 5 out of 100 people, the symptoms stay and treatment is needed. Surgery is only rarely necessary.17 May 2018
How to treat diverticulitis?
In most cases, diverticulitis can be treated at home with oral antibiotics, but if your condition is severe, a hospital stay may be required. Your doctor will recommend getting plenty of rest, taking medication to control pain, and drinking mainly fluids for the first couple of days of your recovery. After the first few days, you should introduce a high-fiber diet into your daily routine to ensure your bowels move regularly. You should incorporate foods such as: 1 Cooked vegetables 2 Cooked fruits 3 Apples 4 Foods rich with probiotics
How long does it take to recover from diverticulitis?
If your condition is being treated with antibiotics, you must take them fully and as directed by your doctor. This can take as long as two weeks. But, you’ll begin to feel better in as short as 24-hours.
Is diverticulitis dangerous?
Diverticulitis can also be dangerous because it shares common symptoms with other conditions — including: Appendicitis. Irritable Bowel Syndrome (IBS) Colon cancer. Urinary Tract Infection (UTI) Pelvic inflammatory disease (PID)
Can diverticulitis be treated with antibiotics?
They may also conduct other tests to help diagnose diverticulitis — including CT scans, ultrasounds of the abdomen, and x-rays of the abdomen. In most cases, diverticulitis can be treated at home with oral antibiotics, but if your condition is severe, a hospital stay may be required.
Can diverticulitis be ignored?
But, if you’re experiencing symptoms of diverticulitis, your answers may come sooner than you expect. That’s because some signs of the condition shouldn’t be ignored — and require an immediate emergency room visit.
What to do if your large intestine is blocked?
If your large intestine is completely blocked, you will need emergency surgery, with possible colon resection. Partial blockage is not an emergency, so you can schedule the surgery or other corrective procedures.
What to do if you have a perforation in your colon?
If you have a perforation, you will likely need surgery to repair the tear or hole. Additional surgery may be needed to remove a small part of your colon if the surgeon cannot repair the perforation.
What is the procedure for a colon resection?
Colon resection. If your bleeding does not stop, a surgeon may perform abdominal surgery with a colon resection. In a colon resection, the surgeon removes the affected part of your colon and joins the remaining ends of your colon together. You will receive general anesthesia.
Can probiotics help with diverticulosis?
Some studies show that probiotics#N#NIH external link#N#may help with diverticulosis symptoms and may help prevent diverticulitis. 5 However, researchers are still studying this subject. Probiotics are live bacteria like those that occur normally in your stomach and intestines. You can find probiotics in dietary supplements—in capsule, tablet, and powder form—and in some foods, such as yogurt.
Does fiber help with diverticulosis?
Although a high- fiber diet may not prevent diverticulosis, it may help prevent symptoms or problems in people who already have diverticulosis. A doctor may suggest that you increase fiber in your diet slowly to reduce your chances of having gas and pain in your abdomen. Learn more about foods that are high in fiber.
How to tell if you have diverticulitis?
Generally speaking, diverticula isn’t harmful. These pouches can exist within your intestines without you ever knowing about it. That’s not the case with diverticulitis. Here are a few symptoms: 1 Severe abdominal pain on your left side 2 Fever and chills 3 Bloating 4 Nausea and vomiting 5 Constipation 6 Blood in your stools
What are the symptoms of diverticulitis?
Severe abdominal pain on your left side. Fever and chills. Bloating. Nausea and vomiting. Constipation. Blood in your stools. Although the presence of diverticulitis isn’t necessarily a dangerous condition on its own, if you experience any of the symptoms listed above, it’s time to see a doctor.
Is diverticulitis dangerous?
When to see a doctor. Generally speaking, diverticula isn’t harmful. These pouches can exist within your intestines without you ever knowing about it. That’s not the case with diverticulitis. Here are a few symptoms: Severe abdominal pain on your left side. Fever and chills.
Can diverticulitis cause death?
Left untreated, diverticulitis can lead to severe consequences, including death. Abscesses are just one complication of diverticulitis that require urgent care. If abscesses form, they can break through the intestinal wall. If this happens you can develop peritonitis, an infection that could be fatal.
Is diverticulitis a rare disease?
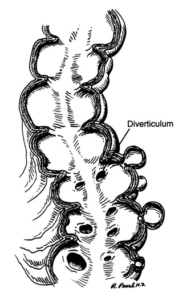
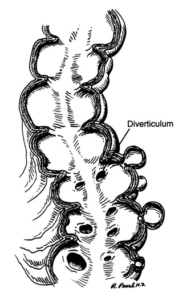
Diverticulitis isn’t a rare condition. It’s a condition that affects your digestive tract and is more likely to happen as you age, most commonly affecting people 40 and older. Diverticulitis is the result of inflammation of small pouches that have the ability to form inside your intestines. Diverticulitis occurs not from the formation ...
How to diagnose diverticulitis?
If you think you have either diverticulosis or diverticulitis, talk to your doctor. Your doctor can perform tests to diagnose the conditions including: 1 A series of contrast images from a CT scan or from X-rays that then are processed and viewed on a computer to see the intestines and surrounding tissue and bones 2 Colonoscopy, a test in which a flexible lighted tube is used to examine the inside of the intestines
What are the factors that contribute to diverticulosis?
Aging and heredity are primary factors in the development of diverticulosis and diverticulitis, but diet also plays a role. Eating a diet low in fiber and high in refined foods may increase the risk. Indeed, in Western societies, an estimated 10% of people over 40 eventually develop diverticulosis; the figure reaches at least 50% in people over 60.
Can you be hospitalized for a perforation?
However, if you have had a perforation or develop a more severe infection, you will probably be hospitalized so you can receive intravenous (through a vein) antibiotics. You may also be fed intravenously to give the colon time to recuperate.
Can diverticulitis be reversed?
Depending on the success of recovery, this procedure may be reversed during a second operation. If you have several attacks of acute diverticulitis, your doctor may want to remove the affected section of the intestine when you are free of symptoms.
What is an IV used for?
Ask your healthcare provider how to prevent or treat constipation. An IV may be used to give you liquids and nutrition. You may not be able to eat or drink anything until your healthcare provider says it is okay. Drainage may be done to reduce inflammation or treat infection.
What causes small pockets in the intestine?
Diverticulitis is a condition that causes small pockets along your intestine called diverticula to become inflamed or infected. This is caused by hard bowel movement, food, or bacteria that get stuck in the pockets.
Why do you need contrast liquid?
You may be given contrast liquid to help your intestines show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. A colonoscopy is used to look at your intestines with a scope. A scope (long bendable tube with a light on the end) is used to take pictures.
What is a scope used for?
A scope (long bendable tube with a light on the end) is used to take pictures. This test may show swollen diverticula or bleeding. Samples may be taken from your digestive tract and sent to a lab for tests. Bleeding may be controlled with tools that are inserted through the scope.
Can you refuse treatment?
You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
What is clear liquid diet?
A clear liquid diet will allow your intestines to heal. A clear liquid diet includes any liquids that you can see through. Examples include water, ginger-ale, cranberry or apple juice, frozen fruit ice, or broth. Ask your healthcare provider for more information on a clear liquid diet.
Can you stop vomiting?
You are not able to have a bowel movement. You cannot stop vomiting. You have severe abdominal pain, a fever, and your abdomen is larger than usual. You have new or increased blood in your bowel movements.
Symptoms that mimic Diverticulitis
There are multiple other conditions that show the same symptoms as diverticulitis. Some of these conditions can be deadly if not treated right away; these conditions include:
When to go to the ER For Diverticulitis
There are a few symptoms of Diverticulitis that should never be ignored. These symptoms point to a more serious complication of the condition and typically require a 2-day stay in the hospital for IV antibiotics and in more serious cases, surgery.
How long does it take for diverticulitis to heal?
Most people who have diverticulitis will recover with about a seven to 10-day course of antibiotics and rest. Severe complication of diverticulitis occur in about the following percent of people: perforation of the colon (1% to 2% of patients), obstruction (rare), fistula (14%) or abscess (30%).
What are the symptoms of diverticulosis?
Keep in mind that having one or more of these symptoms doesn’t mean you have diverticulosis. These symptoms are common symptoms of other gastrointestinal disorders such as irritable bowel syndrome, celiac disease, inflammatory bowel disease, appendicitis, gallstones and stomach ulcers.
What is the difference between diverticulosis and diverticulitis?
Diverticulosis is “the presence of” and diverticulitis is “inflammation and infection of” one or more diverticula (bulges in your colon wall). Diverticulosis is common , doesn’t cause symptoms or need treatment . Mild diverticulitis is treated with antibiotics. Surgery is needed if problems develop. A high fiber diet, exercise and drinking lots of water can help prevent.
How common is diverticulosis?
This condition is very common and increases with age. It is present in about 50% of people over age 60 and in almost everyone over age 80. You likely won’t even have symptoms if you have diverticulosis. If you have a mild case of diverticulosis, it may go away on its own without treatment.
Where are diverticula found?
Although they can form anywhere in the inner lining of your colon, they are most commonly found in your lower left-side, in the S-shaped segment of your colon called the sigmoid colon. Cleveland Clinic is a non-profit academic medical center.
What is a diverticula?
Overview. Diverticula are tiny pockets that form in the wall of your colon. They can become inflamed and infected, causing symptoms and sometimes serious problems including bleeding, blockages and abscesses.
Where is diverticulitis most common?
If the affected area of your colon is removed, another surgery is usually not needed. The most common location for diverticulitis is the sigmoid colon, which is the S-shaped near end portion of your colon. Although this is the most common location, it’s possible for diverticula to form in other areas of your colon.
What is the best treatment for diverticulitis?
Outpatient management with rest and fluids is effective for patients with mild diverticulitis. Inpatient management is recommended in patients with moderate to severe diverticulitis. Broad-spectrum antibiotics covering gram-negative rods and anaerobic bacteria should be used in patients with complicated diverticulitis.
How long after diverticulitis can you have a colonoscopy?
COLONOSCOPY. Colonoscopy is contraindicated in acute diverticulitis, but historically was recommended to be performed four to six weeks after resolution of acute diverticulitis to confirm the diagnosis and to exclude other causes (e.g., colorectal cancer).
Where is diverticulitis found?
In Western societies, most diverticula (85 percent) are found in the sigmoid and descending colons; diverticula in the ascending colon are more common in Asian populations.
What are the factors that contribute to diverticulosis?
Factors associated with diverticulosis include alterations in colonic wall resistance, colonic motility, and dietary issues, such as lack of fiber, that contribute to increased intraluminal pressure and weakness of the bowel wall. 1 Genetic susceptibility is an important component for the development of diverticular disease because monozygotic twins are twice as likely as dizygotic twins to develop diverticulosis. 7 Aspirin and nonsteroidal anti-inflammatory drugs increase the risk of diverticulitis (hazard ratio = 1.2 to 1.7). 8 Other risk factors for diverticulitis include increasing age, obesity, and lack of exercise. 1
Is laparoscopic surgery better than colectomy?
Laparoscopic surgery results in a shorter length of stay, fewer complications, and lower in-hospital mortality compared with open colectomy. The decision to proceed to surgery in patients with recurrent diverticulitis should be individualized and based on patient preference, comorbidities, and lifestyle.
What are the symptoms of diverticulitis?
1, 9 Other possible symptoms include anorexia, constipation, nausea, diarrhea, and dysuria. 1 Patients may have a history of diverticulosis or diverticulitis. Although patients with diverticulitis typically have a fever (usually below 102°F [39°C]), in one study, nine of 62 patients with acute diverticulitis were afebrile. 10 Tachycardia and hypotension may occur and should raise suspicion for complicated diverticulitis. On examination, tenderness only in the left lower quadrant significantly increases the likelihood of acute diverticulitis (positive likelihood ratio = 10.4), as do a palpable mass and abdominal distention. 9
Why is computed tomography important?
Computed tomography, the most commonly performed imaging test, is useful to establish the diagnosis and the extent and severity of disease, and to exclude complications in selected patients.