While vaccines provide the best protection from COVID-19, treatment options such as monoclonal antibodies are available if you have had symptoms of COVID-19 for 10 days or less or have been exposed to COVID-19. If taken early, they can reduce the risk of severe disease, hospitalization, and death.
When to get a booster after monoclonal?
Jan 06, 2022 · Monoclonal antibody treatment is most effective when given early—and the sooner it is given, the better. Treatment is not effective for people who are already hospitalized or severely ill with COVID-19. Monoclonal antibodies should not be considered a replacement for vaccination. “While we have this treatment and it does help keep high-risk people out of the …
How often can you get monoclonal antibodies?
Dec 21, 2021 · When do I need to get the treatment in order for it to work? The monoclonal antibody treatments are meant for mild to moderate COVID cases in adults and children over 12 to prevent the progression...
How effective is the monoclonal treatment?
Feb 01, 2022 · Treatment with anti-SARS-CoV-2 mAbs should be started as soon as possible after SARS-CoV-2 infection is confirmed by an antigen test or a nucleic acid amplification test (NAAT) and within 10 days of symptom onset.
Who is eligible for monoclonal?
Dec 30, 2021 · For starters, a monoclonal antibody cocktail can be given for the treatment of mild-to-moderate Covid-19 in adults and children above 12 years who are at high risk of developing severe COVID-19 infection and/or hospitalisation. It is approved at a combined dose of 1200 mg (600 mg of each drug) administered by intravenous infusion or subcutaneous route.
How do monoclonal antibodies work against COVID-19?
Monoclonal antibodies for COVID-19 may block the virus that causes COVID-19 from attaching to human cells, making it more difficult for the virus to reproduce and cause harm. Monoclonal antibodies may also neutralize a virus.Mar 31, 2022
Can I get the COVID-19 vaccine if I was treated with monoclonal antibodies or convalescent plasma?
If you were treated for COVID-19 symptoms with monoclonal antibodies or convalescent plasma, you should wait 90 days before getting a COVID-19 vaccine.
What is a monoclonal antibody?
Monoclonal antibodies are laboratory-produced molecules that act as substitute antibodies that can restore, enhance or mimic the immune system's attack on cells.Mar 31, 2022
How long does it take for antibodies to develop after exposure to COVID-19?
It can take days to weeks after an infection for your body to make antibodies.Feb 24, 2022
Should you still get the COVID-19 vaccine if you were treated with monoclonal antibodies?
If you were treated for COVID-19 with monoclonal antibodies or convalescent plasma, there is no need to delay getting a COVID-19 vaccine.Feb 17, 2022
Do I need the COVID-19 vaccine if I still have antibodies?
Yes, the COVID-19 vaccines are recommended, even if you had COVID-19.Nov 23, 2021
What is the difference between monoclonal antibodies and the COVID-19 vaccine?
COVID-19 vaccines help stimulate and prepare a person's immune system to respond if they are exposed to the virus. However, monoclonal antibodies boost the immune system only after a person is already sick, speeding up their immune response to prevent COVID-19 from getting worse.Nov 8, 2021
How many types of monoclonal antibody COVID-19 treatments are there in the US?
In the United States, there are three anti-SARS-CoV-2 monoclonal antibody treatments with FDA Emergency Use Authorization (EUA) for the treatment of COVID-19: bamlanivimab plus etesevimab, casirivimab plus imdevimab,, and sotrovimab.
Is there an antibody cocktail for COVID-19?
The treatment, bamlanivimab and etesevimab administered together, was granted FDA emergency use authorization in February. Eli Lilly and the FDA stipulated that the antibody cocktail is authorized as a COVID-19 prophylaxis only for individuals who have been exposed to the virus.Sep 16, 2021
Is it possible to develop immunity to COVID-19 after being exposed?
In addition, the hope is that people who've been exposed to COVID-19 also develop an immunity to it. When you have immunity, your body can recognize and fight off the virus. It's possible that people who've had COVID-19 can get sick again -- and maybe infect other people.Jan 21, 2022
What does a positive antibody test result mean for COVID-19?
A: A positive antibody test result could mean you previously had a SARS-CoV-2 infection or COVID-19. A positive antibody test could also mean the test is detecting antibodies in your blood in response to your COVID-19 vaccine.Feb 24, 2022
What is the COVID-19 antibody test?
COVID-19 antibody tests can help identify people who may have been infected with the SARS-CoV-2 virus or have recovered from a COVID-19 infection.Feb 24, 2022
What is the purpose of monoclonal antibodies?
Monoclonal antibodies targeting the S protein have the potential to prevent SARS-CoV-2 infection and to alleviate symptoms and limit progression to severe disease in patients with mild to moderate COVID-19, particularly in those who have not yet developed an endogenous antibody response. 3.
What are the adverse events of bamlanivimab?
In the Phase 2 Blocking Viral Attachment and Cell Entry with SARS-CoV-2 Neutralizing Antibodies (BLAZE-1) trial, the most common adverse events associated with bamlanivimab were nausea, diarrhea, dizziness, headache, pruritis, and vomiting. The safety profile of bamlanivimab at all three doses was reportedly like that of the placebo.
What antibody targets the RBD of the S protein?
Bamlanivimab (also known as LY-CoV555 and LY3819253) is a neutralizing monoclonal antibody that targets the RBD of the S protein of SARS-CoV-2. Etesevimab (also known as LY-CoV016 and LY3832479) is another neutralizing monoclonal antibody that binds to a different but overlapping epitope in the RBD of the SARS-CoV-2 S protein. Casirivimab (previously REGN10933) and imdevimab (previously REGN10987) are recombinant human monoclonal antibodies that bind to nonoverlapping epitopes of the S protein RBD of SARS-CoV-2.
What is Casirivimab plus imdevimab?
Casirivimab plus imdevimab: These are recombinant human monoclonal antibodies that bind to nonoverlapping epitopes of the spike protein RBD of SARS-CoV-2. Sotrovimab: This monoclonal antibody was originally identified in 2003 from a SARS-CoV survivor.
What are the side effects of monoclonal antibody therapy?
One possible side effect of monoclonal antibody therapy is an allergic reaction. These reactions typically only occur during infusion or soon after, and your care team will closely monitor for any signs of an allergic reaction. However, because an infusion reaction can also be delayed, contact your doctor immediately if you notice any of the following signs of an allergic reaction: 1 Fever and/or chills 2 Nausea 3 Headache 4 Shortness of breath 5 Low blood pressure 6 Wheezing 7 Swelling of lips, face or throat 8 Muscle aches 9 Hives or itchiness
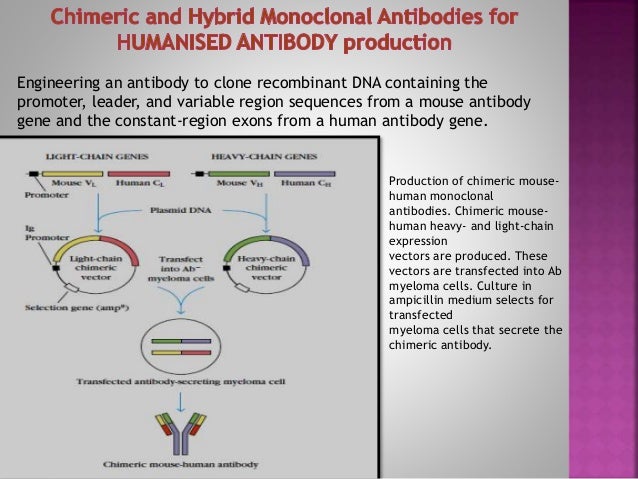
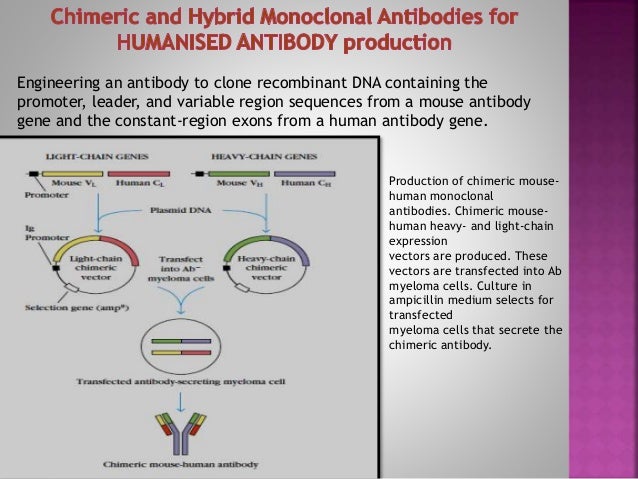
What are monoclonal antibodies?
However, monoclonal antibodies are mass-produced in a laboratory and are designed to recognize a specific component of this virus — the spike protein on its outer shell .
How long should you wait to get a second shot?
If you already received the first dose of vaccine before monoclonal antibody therapy, current CDC guidelines recommend you wait 90 days before receiving the second dose. Categories: Tips to Live By. Tags: Coronavirus, Infectious Disease.
What are the high risk people?
Those who are at high risk include people who: Are 65 years of age or older. Are at least 55 years of age and have heart disease, hypertension or a chronic respiratory disease such as COPD. Have a BMI above 35. Have chronic kidney disease.