
Should doctors set individual health and treatment priorities with patients with multimorbidity?
Patients with multimorbidity often receive diverse treatments; they are subjected to polypharmacy and to a high treatment burden. Hence it is advocated that doctors set individual health and treatment priorities with their patients.
How do older patients evaluate the importance of their multiple health problems?
34 older patients evaluated the importance of their multiple health problems disclosed by a geriatric assessment. When deciding upon the importance of specific health issues, the patients considered the broader impact on their lives rather than disease specific aspects.
What are the main categories for older patients in priority setting?
It is suggested that symptom burden, physical function and survival are the main categories for older patients that determine the decision making in the priority setting process [ 18 ].
Why do patients evaluate their problems as rather unimportant?
Little or no suffering was a reason why patients evaluated their problems as rather unimportant. These problems were either well treated or not severe. Non-severe problems, in the eyes of the patients, were those that of short duration, intermittently present, not (always) intense, improving, or were not linked to medical complications.
When multiple patients are evaluated and prioritized for treatment it is called?
In medicine, triage (/ˈtriːɑːʒ, triˈɑːʒ/) is a practice invoked when acute care cannot be provided for lack of resources. The process rations care towards those who are most in need of immediate care, and who benefit most from it. More generally it refers to prioritisation of medical care as a whole.
What are the 3 categories of triage?
TriageImmediate category. These casualties require immediate life-saving treatment.Urgent category. These casualties require significant intervention as soon as possible.Delayed category. These patients will require medical intervention, but not with any urgency.Expectant category.
What is the difference between primary and secondary triage?
Primary triage is carried out at the scene of an accident and secondary triage at the casualty clearing station at the site of a major incident. Triage is repeated prior to transport away from the scene and again at the receiving hospital.
What are the 4 categories of triage in a mass casualty situation?
In both SALT and START , responders classify each victim involved in a mass casualty incident into the following categories for treatment needs:Green (minimal)Yellow (delayed)Red (immediate)Black (dead)
What is a priority 4 patient?
Priority 4 (Blue) Those victims with critical and potentially fatal injuries or illness are coded priority 4 or "Blue" indicating no treatment or transportation.
What are the 5 levels of triage?
In general, triage categories can be expressed as a Description (immediate; Urgent; Delayed; Expectant), Priority (1 to 4), or Color (Red, Yellow, Green, Blue), respectively, where Immediate category equals Priority 1 and Red color [1,2]. ...
What is triage priority?
[tre-ahzh´] (Fr.) the sorting out and classification of casualties of war or other disaster, to determine priority of need and proper place of treatment.
When should secondary triage occur?
Triage. PERFORMING: Triage will be performed in two phases, PRIMARY TRIAGE: the initial classification of patients and. SECONDARY TRIAGE: when patients enter treatment areas.
What makes a patient high priority?
Medical screening of patients to determine their relative priority for treatment; the separation of a large number of casualties, in military or civilian disaster medical care, into three groups: 1) those who cannot be expected to survive even with treatment; 2) those who will recover without treatment; 3) the highest ...
In which order would the nurse care for clients according to priority of care based on triage tag color?
Red-tagged clients have major injuries, black-tagged clients are expected and allowed to die, and yellow-tagged clients have major injuries.
How is priority of care determined during mass casualty triage?
In this method, immediate and rapid classification of the injured people is based on the type and severity of the injury, the probability of survival, as well as the priority of treatment in order to provide the best health care services for the largest number of people [1], [9], [10].
What criteria does the START triage system used to determine patient priority?
The START triage system classifies patients as red/immediate if the patient fits one of the following three criteria: 1) A respiratory rate that's > 30 per minute; 2) Radial pulse is absent, or capillary refill is > 2 seconds; and 3) Patient is unable to follow simple commands.
What is the order of triage?
Triage is the sorting of children into priority groups according to their medical need and the resources available. After these steps are completed, proceed with a general assessment and further treatment according to the child's priority.
What is basic triage?
Simple triage and rapid treatment (START) is a triage method used by first responders to quickly classify victims during a mass casualty incident (MCI) based on the severity of their injury.
What are the principles of triage?
Results: The classification and prioritization of the injured people, the speed, and the accuracy of the performance were considered as the main principles of triage.
Why is it important for doctors to set individual health and treatment priorities with their patients?
Patients with multimorbidity often receive diverse treatments; they are subjected to polypharmacy and to a high treatment burden. Hence it is advocated that doctors set individual health and treatment priorities with their patients. In order to apply such a concept, doctors will need a good understanding of what causes patients to prioritise some of their problems over others. This qualitative study explores what underlying reasons patients have when they appraise their health problems as more or less important.
What is care planning in multimorbidity?
Care planning in the face of multiple morbidities requires decisions on what and what not to treat. An “expert panel on the care of older adults with multimorbidity” recommends eliciting individual health goals as a guiding principle for these challenging decisions [ 5 ]. “Health goals” are defined here as broad health and life outcomes that people hope to gain or maintain (e.g. everyday function) [ 6 ]. The term “health priorities”, in contrast, refers to the result of individual treatment decisions on the basis of conflicting treatment choices that occur with multimorbidity. Health priorities, ideally, emerge as a result of person-centered care planning processes, in which patients reflect and reveal what matters to them. However, in practice all too often the medical perspectives of physicians guide the decision on what to treat [ 7 ]; and it has become evident that physicians tend to focus on clinical aspects whereas patients primarily consider everyday life effects [ 8, 9 ]. The different perspectives result in substantial disagreements on health and treatment priorities [ 10, 11 ], which makes it even more important to include patients’ views when setting priorities in a care planning process.
Why are chronic conditions important?
The patients find their chronic conditions important, if they are associated with substantial physical, emotional or functional strains. A high symptom burden or prospect of medical complications contribute to physical strain. Impaired functions impact on daily lives, in particular on mobility, independence, self-sufficiency and social relations. Negative feelings accentuate the importance of a problem.
How many health problems did patients explain?
Altogether, patients gave explanations for 245 important health problems. Four main themes emerged, in which explanations were assigned to further subcategories (see Fig. 1 ).
What are the health problems associated with suffering?
Different types of health problems were associated with suffering such as pain, difficulty sleeping, dysaesthesia, incontinence, chest pain, falls and hearing impairment. Underlying functional impairments were also rated important. In the first instance, patients felt compromised managing their daily tasks.
Why is it important to ask patients about their health problems?
Asking patients with multimorbidity, which health problems are important, may guide physicians to treatment priorities and health problems in need of empowerment .
How did Schreier use qualitative content analysis?
First, we selected text material that dealt with the importance of a health problem. A coding frame was developed with the themes “important”, “unimportant” and “both, important and unimportant” as well as “type of health problem” as main categories. Subcategories were generated as data driven codes and arranged under the main categories. Subcategories could be only coded once under one main category to assure reflective demarcation between subthemes. Each subcategory received an explanation, indicators and a coding example to guide the coding procedure. In this way, two investigators (UJW and UV) developed the coding frame using two interviews. TS and UV then independently piloted four further interviews with an overall 87% agreement of coding. Differences in codings were discussed and the coding frame altered. Using the final coding frame, UV then coded all 34 interviews. Mindmaps were created for each main category to explore cross-thematic findings in the subcategories.
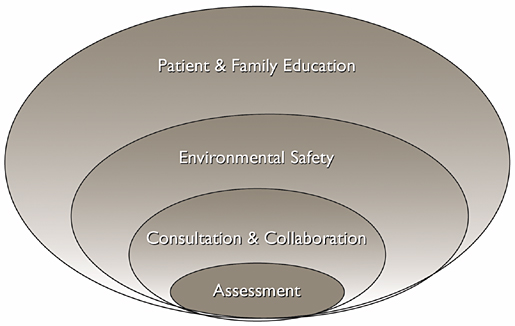
The list of all the things
As you go through shift report, assess your patient and look through the chart, you are going to start zeroing in on all the abnormal findings. Start a list of all these things, but don’t worry about prioritizing them just yet…just get them down on paper.
Prioritizing like a pro
Looking at your list of real and potential problems, you’re going to assign each item a rating.
Some questions to ask yourself
Is this an acute problem or a chronic problem? (acute problems usually take precedence over chronic ones)
What are the priorities of focus groups?
Focus groups identified different priorities, including “increase their connection to community and recovery services”.
What are the priority outcomes for men and women?
The priority outcomes selected most frequently by men and women were identical in four of five cases: 1) “Have improved quality of life”; 2) “stay alive”; 3) “stop alcohol and drug use”; and 4) “address issues that come up in daily life.” The women’s list included “improve mental health.”
What is the benchmark for substance use recovery?
For the first several decades of treatment and recovery support service provision, abstinence has been the primary benchmark used by providers, researchers, and government agencies to evaluate successful recovery from a substance use disorder. This narrow focus on substance use versus non-use has come under increasing criticism from several perspectives. The growing field of recovery research has introduced the concept of multiple paths of recovery, including moderation and Harm Reduction-based paths. A nationally representative survey of people in recovery shows that many people resolve their problem despite continuing to use substances, return to moderate use in recovery, or combine abstinence from one substance with using others. Clinically, too, individuals may be using substances and still achieve substance use disorder remission (sustained remission is defined by meeting diagnostic criteria for at least 1 year and then reporting no symptoms for 1 year). For example, among individuals in remission from alcohol use disorder, 1/3 are abstinent, 1/3 are drinking but within NIAAA’s low-risk guidelines, and 1/3 are drinking beyond the low-risk drinking thresholds. This data has prompted calls to move away from use/non-use as the only metric to mark and measure recovery.
What are the outcomes of the National Peer Council?
Based on the findings from the focus groups and surveys, the National Peer Council and staff from the sponsoring organizations created a revised priority outcomes list: 1) “staying alive”; 2) “improving quality of life”; 3) “reducing harmful substance use”; 4) improving mental health; 5) “meeting their basic needs”; 6) “increasing self-confidence/self-efficacy”; 7) “increasing connections to services and supports.” This list is described as capturing the outcomes of service that are “the most important to individuals with lived experiences”.
What is recovery in psychology?
A new generation of research defines recovery as a dynamic, goal-directed process of change that may be best measured using multiple dimensions, such as, personal growth, quality of life, and fulfilling relationships, and other aspects of wellbeing. These arguments build on studies showing great diversity in how people who identify as being in recovery describe the core elements of their experience. Nevertheless, there is little consensus regarding what aspects of recovery to measure, how to measure them, and on what time scale. This confusion has made it difficult, if not impossible, for treatment providers and government agencies to adopt standardized metrics of success for individuals involved with treatment and recovery support services. Such metrics are key for judging the effectiveness of such services and supporting decision making for providers, policy makers, scientists, and individual stakeholders alike.
What is patient centered care?
Forms of patient centered care include a non-judgmental approach (“meeting people where they are at”), individualized treatment, including patients in crafting treatment plans or shared decision making, and holistic or integrated services. The successful integration of patient centered care in other domains has led to calls for developing a similar comprehensive and evidence-based framework for the treatment of substance use disorders.
What is Faces and Voices of Recovery?
This project was a novel collaboration between Faces and Voices of Recovery, a leading recovery advocacy organization, and the American Society for Addiction Medicine. It represents an important step toward placing the voices of people directly impacted by substance use, including family members, at the center of discussions about what outcomes should be prioritized in treatment and recovery support services. Through the central role played by the National Peer Council, the project also validated the leadership and placed great value in the expertise of people with lived experiences of addiction. Critically, the project attempted to represent, primarily through the National Peer Council and focus groups, the perspectives of racially and ethnically diverse groups that are often marginalized or excluded. Their contributions underscore the need to promote the leadership of African American, Indigenous, and People of Color in the addiction and recovery fields.
