The most common definition of treatment-resistant schizophrenia denotes patients with schizophrenia who, despite at least two adequate trials of classical neuroleptic drugs, have persistent moderate to severe positive, or disorganisation, or negative symptoms together with poor social and work function over a prolonged period of time.
Is there a permanent cure for schizophrenia?
Yes there is a permanent cure for Schizophrenia through PyrAmid Energy Healing Techniques and Homeopathy Medicine combination. I have helped many such cases successfully and within 6 months.
What are the different treatments for schizophrenia?
- Omega-3 fatty acids. Omega-3 supplementation has been explored for a variety of mental disorders. ...
- Vitamin supplementation. Early evidence indicates that supplementation with B vitamins may help reduce psychiatric symptoms in some individuals with schizophrenia.
- Diet. ...
What is treatment resistant?
- mood and anxiety disorders;
- substance use disorders;
- post-traumatic stress disorder (PTSD); and
- eating disorders.
How to cure schizophrenia permanently?
- Eating a healthy diet and getting regular exercise
- Maintaining a healthy weight
- Getting enough sleep
- Avoiding drugs and alcohol
- Spending time with family and friends
- Taking time to do enjoyable and relaxing activities
- Avoiding taking on too many responsibilities
- Setting goals
- Using relaxation strategies, like meditation or yoga
What is treatment-resistant schizophrenia definition?
The most common definition of treatment-resistant schizophrenia denotes patients with schizophrenia who, despite at least two adequate trials of classical neuroleptic drugs, have persistent moderate to severe positive, or disorganisation, or negative symptoms together with poor social and work function over a prolonged ...
Why do schizophrenics resist treatment?
Key Takeaways. Many people with schizophrenia suffer from anosognosia, which means they don't understand that they're sick—and, therefore, may not understand the need for treatment. Antipsychotic medication can cause side effects such as major weight gain, muscle spasms, and reduced sexual drive.
What is the treatment for treatment-resistant schizophrenia?
Clozapine remains the first-line medication for treatment-refractory psychotic symptoms. In cases of partial response, the combination with SGAs such as sulpiride, amisulpride, aripiprazole, ziprasidone and risperidone is justified in order to supplement its antidopaminergic properties.
Is treatment-resistant schizophrenia a diagnosis?
Treatment-resistant schizophrenia (TRS) affects ~30% of people with a diagnosis of schizophrenia. TRS is defined as nonresponse to at least two trials of antipsychotic medication of adequate dose and duration,2 at which point, the antipsychotic clozapine is indicated.
Why do schizophrenics refuse medication?
The single most significant reason why individuals with schizophrenia and bipolar disorder fail to take their medication is because of their lack of awareness of their illness (anosognosia). Other important reasons are concurrent alcohol or drug abuse; costs; and a poor relationship between psychiatrist and patient.
What percent of schizophrenia is treatment-resistant?
Response to antipsychotic therapy is highly variable, and it is not currently possible to predict those patients who will or will not respond to antipsychotic medication. Furthermore, a high percentage of patients, approximately 30%, are classified as treatment-resistant (treatment-resistant schizophrenia; TRS).
What does resistant to treatment mean?
In personality disorders, treatment resistance is often mentioned, but in the sense of resistance to entering or to pursuing psychotherapy. What is supposed to be an inadequate response differs from disorder to disorder and is sometimes defined differently in a first step treatment versus a treatment resistant patient.
Why is clozapine used for treatment resistant schizophrenia?
Clozapine is also indicated in patients with schizophrenia who show severe, untreatable adverse neurological reactions to other antipsychotics, including second-generation antipsychotics. Treatment with clozapine decreases overall mortality in schizophrenia, in part by reducing suicidality.
What do you mean by refractory schizophrenia?
Treatment resistance is typically characterized by the failure of symptoms to remit after more than 2 antipsychotic trials of adequate duration (at least 6 weeks), although it has been suggested that the definition include the continuation of symptoms after one medication fails to achieve satisfactory remission.
Is treatment-resistant schizophrenia categorically distinct from treatment responsive schizophrenia?
The identified studies indicate that treatment-resistance may be differentiated by abnormalities in brain glutamate concentrations not seen in treatment-responsive patients; as with the dopamine findings, this again suggests a categorical difference rather than one of severity.
Which of the following drug is indicated in refractory schizophrenia?
Abstract. Objective: Clozapine remains the only medication indicated for refractory schizophrenia. As new antipsychotic drugs become available, their efficacy compared to clozapine, particularly in moderately ill patients, is of great clinical interest.
What is EPS diagnosis?
Extrapyramidal symptoms (EPS) are symptoms that develop in our body's neurological system that cause involuntary or uncontrolled movements. Those symptoms may be in a variety of locations in the body including the trunk, arms, legs, feet, neck, mouth, and eyes.
How do you convince a schizophrenic to take medication?
Articles On Caring for Someone With Schizophrenia Ask them about their fears, concerns, and complaints -- and listen without judging. Make decisions about medications together, along with your loved one's doctor. Work to build and keep trust, so they feel safe to let you know how they are really doing.
What happens when antipsychotics don't work?
If you are taking an antipsychotic which you feel is not working, or if the side effects are difficult to live with, then you should discuss this with your GP or psychiatrist. You should not stop taking antipsychotics suddenly. Your antipsychotics can interact with other medications.
What is treatment-resistant schizoaffective disorder?
Introduction. Treatment-resistant schizophrenia (TRS) has been defined as the persistence of symptoms despite ≥2 trials of antipsychotic medications of adequate dose and duration with documented adherence. 1,2. TRS occurs in up to 34% of patients with schizophrenia. 3,4,5.
How do people with schizophrenia want to be treated?
8 Ways to Help Someone Live Well With SchizophreniaEncourage Them to Schedule Regular Doctor's Appointments. ... Remind Them to Keep Taking Their Medications and Talk to Their Doctors About Any Concerns. ... Help Them Avoid Alcohol and Illicit Drugs. ... Help Them Reduce Their Stress. ... Help Them Maintain a Healthy Weight.More items...•
Why is schizophrenia not responding to treatment?
8 A large number of patients have schizophrenia that does not respond because pharmacological, psychological, and psychosocial treatments are inadequate.
How long does chronicity last in schizophrenia?
In contrast with treatment-resistant schizophrenia, chronicity is associated with a favorable response to drug treatment, in which schizophrenic features are largely under control for 6 months or longer or there is partial recovery to the premorbid level of functioning. 4,5.
How long does it take to treat schizophrenia with clozapine?
Typical antipsychotics can be used for 4 to 6 weeks to screen for treatment-resistant schizophrenia, after which treatment with clozapine may be considered.
When should clozapine be used?
Clozapine should be used only when it is confirmed that patients have treatment-resistant schizophrenia and their condition fails to respond to atypical antipsychotics or typical antipsychotics. The same rule applies in identifying clozapine-resistant schizophrenia.
How many antipsychotics should be tried for schizophrenia?
As shown in the Figure, at least 2 antipsychotic drugs should be tried at adequate dosage and for an adequate period, and various factors that interfere with adherence should be ruled out before making a diagnosis of treatment-resistant schizophrenia.
How many people have schizophrenia?
It is estimated that between 20% and 60% of patients have schizophrenia that is resistant to treatment. 1,2
Is schizophrenia a chronic disorder?
Chronicity has often been confused with treatment-resistant schizophrenia. Schizophrenia is a chronic disorder that progresses to various levels of clinical deterioration without sustained remission or full recovery. In contrast with treatment-resistant schizophrenia, chronicity is associated with a favorable response to drug treatment, ...
What is the best treatment for TRS?
Treatment Alternatives for TRS. Despite recent controversy, clozapine for TRS remains the most established treatment option. However, if an individual is unable to tolerate or is refusing clozapine, high-dose monotherapy with an alternative antipsychotic can be considered. High-dose olanzapine, at a dosage of 30-40 mg/d, ...
Is Clozapine good for schizophrenia?
Glutamate Hypothesis of Schizophrenia. An explanation for clozapine’s superior efficacy may rest with the glutama te hypothesis of schizophrenia. In individuals with schizophrenia, there is an increase in striatal presynaptic dopamine synthesis capacity.
Is topiramate good for psychopathology?
Topiramate was also found to be effective for positive and negative symptoms, as well as general psychopathology, but is not recommended due to a higher discontinuation rate. With lamotrigine, after removal of 2 outliers, there was no significant difference between lamotrigine augmentation and clozapine monotherapy. 16. ...
Is clozapine good for TRS?
Conclusion. For individuals with TRS, clozapine should be considered. Some evidence supports high-dose olanzapine for TRS. Due to the varied symptom presentation of TRS, individual symptoms should be specifically addressed rather than utilizing a "one size fits all" approach.
What is schizophrenia?
Schizophrenia is a severe mental disorder characterized by positive, negative, and cognitive symptoms ( 1 ). The treatment of schizophrenia was revolutionized by the introduction of chlorpromazine in the 1950s ( 2 ).
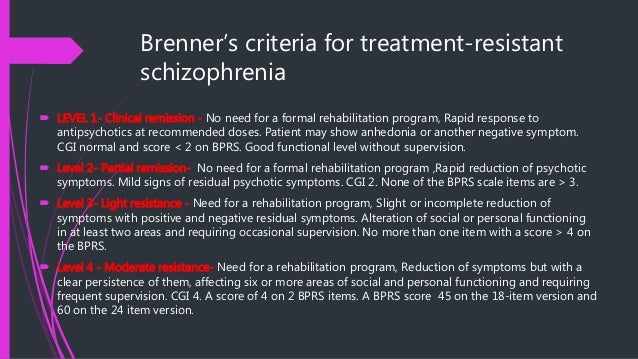
What are the criteria for treatment resistance?
First, the criteria must encompass a core definition of treatment resistance that captures the worldwide understanding of the concept. Second, the criteria must be applicable across a range of study designs, from longitudinal clinical trials to experimental medicine studies to cross-sectional mechanistic investigations. Third, the criteria must identify a group of patients who are clearly distinct from those whose illness is not treatment resistant. Finally, the criteria must be practical, so that they can be used in a wide range of settings but still be rigorous.
What is the failure of at least two adequate treatment episodes with different antipsychotic drugs?
Failure of at least two adequate treatment episodes with different antipsychotic drugs, each meeting the above criteria, is required to establish treatment resistance. In some clinical guidelines it is recommended that these trials include different types of antipsychotics (such as first- and second-generation drugs) ( Table 1 ). However, given the overlap in side effects, efficacy, and receptor profiles among currently available non-clozapine antipsychotics, the consensus was that the current data do not delineate distinct categories of non-clozapine antipsychotics ( 11, 55 ). There was some disagreement about this conclusion among the working group members, as olanzapine, risperidone, and amisulpride show consistent, although small, advantages in meta-analyses of efficacy ( 56 ). However, consensus was reached that, when considering this from a practical perspective as well, specifying particular drugs would limit generalizability, not least because a given drug may not be readily available in some settings (for example, amisulpride in the United States). In view of this, a requirement to use particular categories or drugs (apart from clozapine) is not currently recommended. Of course, particular drugs may be stipulated in a given study when there is a specific reason to focus on patients who have not responded to a certain drug or group of drugs. In practice, many patients will have tried a large number of different drugs ( 16 ). In view of this, the total number of failed adequate antipsychotic treatment trials, the drugs, and their dosage and route of administration should be ascertained and reported where possible. As mentioned above, a trial with a long-acting injectable antipsychotic would be optimal to establish treatment resistance not confounded by treatment nonadherence.
Why is nonadherence important in schizophrenia?
Because of difficulties with adhering to dosing schedules, lack of illness insight, side effect burden, cognitive impairment, and other factors , nonadherence is a significant problem in the treatment of schizophrenia and is often underrecognized ( 78 – 81 ). Nonadherence may be the single largest source of unrecognized error in studies of treatment resistance ( 78 ). Consequently, it is important to make strenuous efforts to determine adherence and to apply criteria to exclude poorly adherent subjects, who can represent false positive “pseudo-resistant” cases. While 100% adherence is rare even in clinical trial settings ( 82, 83 ), it is necessary to be close to this figure; otherwise, the study will be of nonadherence rather than of treatment resistance.
Is schizophrenia a clinical problem?
Treatment-resistant schizophrenia is a major clinical problem, and clinical guidelines throughout the world recommend specific treatments for affected individuals ( 5 – 7 ). A wide variety of criteria have been applied in research studies. As a consequence, clinical guidelines based on these studies use imprecise or inconsistent definitions that are likely to include patients with very different clinical characteristics from those of the patients included in the clinical trials on which the guidelines are based. Furthermore, the variation in criteria limits comparison of studies, complicates the interpretation of findings, and may contribute to the failure to replicate findings ( 12, 13 ).
Is treatment resistance a binary variable?
Treatment resistance is mostly treated as a binary variable as a study entry or treatment decision criterion in research and clinical practice . This is often necessary for research purposes and when making clinical decisions. Clinically, however, a continuum is apparent ( 41 ).
Is schizophrenia limited by treatment resistance?
Research and clinical translation in schizophrenia is limited by inconsistent definitions of treatment resistance and response. To address this issue, the authors evaluated current approaches and then developed consensus criteria and guidelines.
What is treatment resistant schizophrenia?
Patients with treatment-resistant schizophrenia can be broadly defined to include any persons with residual symptoms that cause distress or impairment despite several treatment at-tempts. Unfortunately, this definition may include most of our patients with schizophrenia.
Who submitted the supplement to Current PsyChiatry?
This supplement to Current PsyChiatry was submitted by Asante Communications, LLC; supported by educational grants from Eli Lilly and Company and Janssen, Division of Ortho-McNeil-Janssen Pharmaceuticals Inc; and administered by Ortho-McNeil-Janssen Scientific Affairs. It was peer reviewed by Current PsyChiatry.