Parental consent is not required for a minor who has been emancipated. An emancipated minor may give effective consent to treatment, and no other person’s consent is required. G.S. 90‐21.5(b).
Do I need parental consent to see a therapist?
Aug 01, 2011 · Finally, most states allow a minor to consent to evaluation and treatment of specific medical conditions without the consent of a parent, generally including mental health services, treatment for drug and alcohol addiction, pregnancy-related care, contraceptive services, and testing for and treatment of sexually transmitted diseases.
Why do I need parental consent?
In early 2017, the French supreme court (the Conseil d’Etat) considered an appeal relating to the care of a brain damaged infant, Marwa Bouchenafa. 19 In France, the Public Health code L1110-5 allows doctors to discontinue treatment without parental consent if they believe it would be of “no use, disproportionate, or only serving to artificially maintain life without other effect”. 20 Marwa …
What legal age can you be treated without parental consent?
A minor is a person who is under the legal age of full legal rights and responsibilities. CDC assessed the statutes and regulations (laws) addressing a minor’s legal right to provide informed consent to receive STD and/or HIV services without the consent, knowledge, or involvement of a parent or guardian, in each of the 50 states and the District of Columbia (jurisdictions).
How do you write a medical consent form?
Children and young people. People aged 16 or over are entitled to consent to their own treatment. This can only be overruled in exceptional circumstances. Like adults, young people (aged 16 or 17) are presumed to have sufficient capacity to decide on their own medical treatment, unless there's significant evidence to suggest otherwise. Children under the age of 16 can consent to …
When can doctors override parents?
If the child's parents are not acting in the best interest of their welfare, the state can override parental decisions. At the end of the day, the child's life is the primary concern. A parent can face loss of custody or criminal charges for failing to provide the necessary medical care for their child.Jul 25, 2017
Do parents have the right to make medical decisions?
Parents have the responsibility and authority to make medical decisions on behalf of their children. This includes the right to refuse or discontinue treatments, even those that may be life-sustaining. However, parental decision-making should be guided by the best interests of the child.
What if parents disagree on medical treatment?
If your child's legal custodian refuses a life-saving or life-improving medication, surgery, vaccine, or other medical procedure and you disagree, you can petition the court for intervention.
What do you do when your parents refuse medical care?
Try asking another family member or friend to reach out to your parent to express concern about the medical problem, encourage them to go to the doctor, and ask if they'd offer to take your parent to the doctor. If your parent is living in a senior community, there may be on-site nurses who can check in on them.
What are some examples of where consent is not required to care for a minor?
Some examples where consent is not required to care for a minor can include: Emergency circumstances – The child will likely die before the healthcare provider can consult parents or seek court intervention if the parents are withholding consent. The child is in foster care – The doctor can perform treatment, but must notify ...
When is implied consent invoked?
Implied Consent. Implied consent to medical treatment is invoked when a child’s parent or legal guardian is not available to give consent, especially if the child has life-threatening injuries. In that situation, the law presumes consent would be granted by the parent or legal guardian. Some examples of this include:
Can a doctor perform treatment for a child in foster care?
The child is in foster care – The doctor can perform treatment, but must notify the person who is authorized to consent to medical care for the child no later than the second business day after treatment. Suspicion of child abuse – The is scary, but true. If the physician has reasonable grounds to believe the child’s physical or mental condition is ...
Can a doctor tell if a child is serious?
The child’s condition is serious, but doctors cannot tell how serious without running tests. The parents are unavailable. Consent Not Required. Unlike implied consent, a physician can make the call to provide treatment to a child even if the parents or legal guardians refuse to give consent.
Is consent required for child abuse?
Suspicion of child abuse – The is scary, but true. If the physician has reasonable grounds to believe the child’s physical or mental condition is due to abuse or neglect, consent for treatment is not required. It is important to note that the State can consent to medical treatment for a child and has a wide range of power to limit parental freedom ...
INTRODUCTION
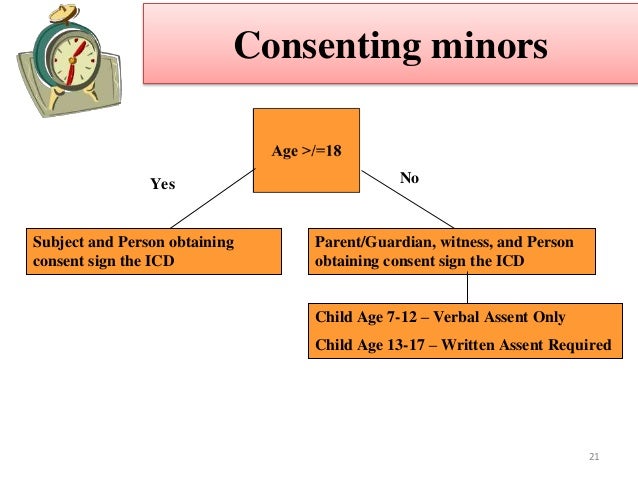
Minors (persons under the age of legal consent as defined by state law) often require care in the prehospital environment and present to emergency departments (EDs) with medical concerns. Parental consent generally is required for the medical evaluation and treatment of minor children.
EVALUATION AND TREATMENT OF THE UNACCOMPANIED MINOR
If a parent or legal guardian is present or available, the health care professional treating the child should make every reasonable effort to obtain and document informed consent. Children occasionally present to the ED unaccompanied by a parent or legal guardian.
EMANCIPATION AND THE MATURE MINOR DOCTRINE
There are 3 situations in which a minor, rather than his or her parents, has the legal authority to make decisions regarding his or her health care: emancipation; the mature minor exception; and exceptions based on specific medical conditions.
CONSENT FOR NONURGENT PEDIATRIC CARE OF CHILDREN ACCOMPANIED BY SOMEONE WHO IS NOT AUTHORIZED TO PROVIDE LEGAL CONSENT
Health care professionals should refrain from providing nonurgent testing and treatment to children who present to medical facilities unaccompanied by a custodial parent or legal guardian.
REFUSALS OF CONSENT FOR EMERGENT EVALUATION AND TREATMENT
A particularly challenging situation occurs when the health care professional is faced with a legal guardian who refuses to give permission for treatment of a child in situations in which such treatment is considered essential to the child's well-being.
INFORMED CONSENT AND THE LANGUAGE BARRIER
If a language barrier exists, informed consent for medical treatment should, when clinical circumstances permit, be obtained through a trained medical interpreter.
CONSENT AND CONFIDENTIALITY
State statutes that allow the consent of a minor do not all guarantee an adolescent protection from parental disclosure. However, some states explicitly require either confidentiality or parental notification.
What is the age limit for a minor to consent to their own health care in Indiana?
INDIANA. Ind. Code § 16-36-1-3. A minor may consent to the minor’s own health care if the minor is: (i) At least 14 years of age; (ii) Not dependent on a parent for support; (iii) Living apart from the minor’s parents or from an individual in loco parentis; and. (iv) Managing the minor’s own affairs. KANSAS.
What is the law in North Dakota for unaccompanied minors?
SB 2265 (2021) An unaccompanied homeless minor 14 years of age or older may consent to, contract for, and receive medical, dental, or behavioral health examinations, care, or treatment without permission, authority, or consent of a parent or guardian.
What is the code for a minor in Montana?
MONTANA. Mont. Code § 41-1-402. A minor who professes to be or is found to be separated from the minor’s parent, parents, or legal guardian for whatever reason and is providing self-support by whatever means may consent to the provision of health services and to control access to protected health care information.
How old do you have to be to get medical care in Alaska?
Any minor who is 14 years of age or older, or has graduated from high school, or is married, or having been married is divorced or is pregnant may give effective consent to any legally authorized medical, dental, health or mental health services for himself or herself, and the consent of no other person shall be necessary. ALASKA.
Is consent necessary for medical care in Arkansas?
The consent of the parent, or parents, of such a person is not necessary in order to authorize hospital, medical and surgical care. ARKANSAS. Ark. Code § 20-9-602 (7) Any one of the following persons may consent, either orally or otherwise, to any surgical or medical treatment or procedure not prohibited by law that is suggested, recommended, ...
Can a minor give consent to a dentist?
A minor living apart from his or her parents and who is managing his or her own financial affairs, regardless of the source or extent of income, may give consent for medical or dental services. ARIZONA. Ariz. Rev. Stat. § 44-132.
Can a minor get dental care without parental consent?
Medical, dental and health services may be rendered to minors of any age without the consent of a parent or legal guardian when, in the physician’s judgment, an attempt to secure consent would result in delay of treatment which would increase the risk to the minor’s life or health. RHODE ISLAND.
What is the law that allows a minor to give consent to HIV testing?
Laws that explicitly allow a minor to give informed consent to HIV testing, treatment, and/or prophylaxis, including pre-exposure prophylaxis (PrEP), or. Laws that allow a minor to give informed consent to general health care, services, or procedures. As of 2020, all jurisdictions have laws that explicitly allow a minor of a particular age ...
Can a minor give consent to HIV treatment?
Jurisdictions have different types of laws, and the age at which the minor has the legal right to provide informed consent to receive STD or HIV services varies by jurisdiction: Laws that explicitly allow a minor to give informed consent to receive STD diagnosis and treatment, and/or prevention. Laws that explicitly allow a minor ...
What age can you consent to medical treatment?
Assessing capacity. Children and young people. People aged 16 or over are entitled to consent to their own treatment. This can only be overruled in exceptional circumstances. Like adults, young people (aged 16 or 17) are presumed to have sufficient capacity to decide on their own medical treatment, unless there's significant evidence ...
How many parents do you need to give consent to a doctor?
By law, healthcare professionals only need 1 person with parental responsibility to give consent for them to provide treatment. In cases where 1 parent disagrees with the treatment, doctors are often unwilling to go against their wishes and will try to gain agreement.
What happens if a young person refuses treatment?
If a young person refuses treatment, which may lead to their death or a severe permanent injury, their decision can be overruled by the Court of Protection. This is the legal body that oversees the operation of the Mental Capacity Act (2005).
Who can consent for a child?
Otherwise, someone with parental responsibility can consent for them. This could be: the child's mother or father. the child's legally appointed guardian. a person with a residence order concerning the child. a local authority designated to care for the child.
What is parental responsibility?
Parental responsibility. A person with parental responsibility must have the capacity to give consent. If a parent refuses to give consent to a particular treatment, this decision can be overruled by the courts if treatment is thought to be in the best interests of the child.
When is parental consent required?
Parental consent is required if the health care involves any serious risks or if it may cause grave and permanent effects to the child. In British Columbia 10, minors 11 may consent to health care if they understand the nature and consequences of the health care, as well as the reasonably foreseeable benefits and risks.
What are the two conditions for consent to medical treatment?
Two general requirements and conditions for obtaining consent to medical treatment are that the patient must have capacity for the treatment decision and that the consent must be informed. According to the common law, capacity is the ability to appreciate the nature, purpose and consequences of the proposed treatment.
What is the infants act?
10 Infants Act, RSBC 1996, c 223. 11 In British Columbia, the legislation defines a person under the age of majority as an “infant” instead of a “minor”. 12 Medical Consent of Minors Act, SNB 1987, c M-6.1. 13 The inherent jurisdiction of the courts to make decisions concerning people who are not able to take care of themselves.
What is the determining factor in medical treatment?
The determining factor is whether the person is capable. A person is capable if he or she is able to understand the information that is relevant to making the decision about the proposed medical treatment and is able to appreciate the reasonably foreseeable consequences of a decision or lack of a decision.
What is child welfare law?
All provinces and territories have enacted child welfare legislation which overrules the common law, allowing a court to override the consent or decision of a minor in certain circumstances. Such circumstances often relate to the well-being of the minor or the court determining that the minor is in need of “protection”.
What is a minor in Canada?
A minor is an individual under the age of majority. The age of majority varies among the provinces and territories. In provinces 3 where there is no consent and capacity legislation the common law governs. On the issues of minors and consent to medical treatment, the Supreme Court of Canada has endorsed the “mature minor” doctrine 4.
What is informed consent?
Informed consent requires that the patient has been advised of the material risks and benefits of the proposed medical treatment and the alternatives. The failure of a health care professional to obtain consent, or to obtain informed consent, exposes the health care provider to liability 2. The process of obtaining consent for a patient who is ...
What is the right to consent to medical treatment?
Adults with capacity have a right to decide what happens to their own bodies. This means that they have the right to consent to treatment, refuse to consent to treatment for any reason, or withdraw their consent, even if refusal or withdrawal of treatment is likely to lead to serious injury or death. These principles are reflected in the law that governs consent to medical treatment. As a general rule, no operation, procedure or treatment may be undertaken without prior consent from the patient or, if the patient lacks capacity, from the patient’s substituted decision maker.
Why is consent not required?
Consent is generally not required where the patient lacks capacity and immediate treatment is necessary to save a person’s life or prevent serious injury to their health. Treatment in this context extends to all actions reasonably required to provide the treatment, such as restraint. Treatment (other than Special Medical Treatment) can also be provided without consent to alleviate significant pain and distress. However, treatment cannot be provided without consent in an emergency if providing the treatment would be contrary to a valid prior refusal of treatment, such as an ACD.
What are some examples of treatment programs?
Antineoplastic agents (for example, chemotherapy) and the administration of blood products to patients with haemophilia are examples of a treatment program. Wound therapy dressing changes could also be considered a treatment program.
What is the NSW Health Policy Directive?
NSW Health Policy Directive Aboriginal and Torres Strait Islander Origin – recording of Information of Patients and Clients (PD2012_042) outlines the requirements for collecting and recording accurate information on whether clients of NSW Health services are Aboriginal and/or Torres Strait Islander. If the patient identifies as Aboriginal and/or Torres Strait Islander, they should be offered the services of an Aboriginal Hospital Liaison Ocer or Aboriginal Health Worker where available.
What is electronic medical records?
Some electronic medical records programs have capability to capture the patient’s consent to a proposed treatment or procedure. It is important to remember that the elements or four criteria of a valid consent must be met regardless of the method used to capture consent.
What is the role of a health practitioner in a new procedure?
Where a Health Practitioner is proposing a new or novel procedure, such as a procedure using a new technology or device, the Health Practitioner must inform the patient that the procedure or treatment is new to their practice and provide the patient with details of their previous (potentially limited) experience with the procedure or treatment as part of the consent process. This discussion should be documented in the Health Record. The discussions should include:
How long does it take to get a consent form for septoplasty?
He is classified as urgency category 3 – surgery recommended within 365 days. When the patient is admitted to hospital for the surgery, 14 months have passed since the date that the consent form was signed. However, as the patient’s health has not changed in that time, and there have been no changes in the way that the surgery will be performed, the consent form is still valid. Even so, the patient’s consent should still be re-confirmed verbally by the operating surgeon immediately prior to the surgery.