When is bradycardia considered dangerous?
Feb 03, 2020 · In fact, in most people, bradycardia does not require treatment unless patients have symptoms that are clearly due to a slow heartbeat. The following are conditions that produce bradycardia that requires treatment: Cardiac arrhythmias resulting from sinus node dysfunction. Similarly, how do you treat bradycardia naturally?
When does bradycardia require treatment ACLS?
Severe or prolonged bradycardia can be treated in a few ways. For instance, if medication side effects are causing the slow heart rate, then the medication regimen can be adjusted or discontinued. In many cases, a pacemaker can regulate …
When does an elevated heart rate become dangerous?
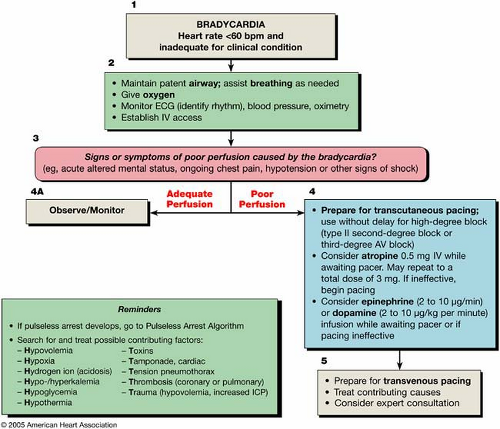
Aug 27, 2019 · When does bradycardia require treatment ACLS? Symptomatic bradycardia, heart rate typically <50 beats per minute with presence of symptoms, is identified and treated directed at the underlying cause. Maintain a patent airway with assisted breathing as necessary. What is the infusion rate for epinephrine in the bradycardia algorithm?
When does a fast heartbeat need treatment?
Sometimes bradycardia is a good thing and is the goal of treatment. If you need treatment, it will be based on the cause of the condition. If you have an electrical problem in your heart, you will need a pacemaker to keep your heart beating as it should.
What are the symptoms of bradycardia?
Symptoms of bradycardia include: Fatigue or feeling weak. Dizziness or lightheadedness. Confusion. Fainting (or near-fainting) spells. Shortness of breath. Difficulty when exercising.
What causes bradycardia in the heart?
Causes for bradycardia include: Problems with the sinoatrial (SA) node, sometimes called the heart’s natural pacemaker. Problems in the conduction pathways of the heart that don’t allow electrical impulses to pass properly from the atria to the ventricles.
What is the best heart rate for bradycardia?
In general, for adults, a resting heart rate of fewer than 60 beats per minute (BPM) qualifies as bradycardia. But there are exceptions. Your heart rate may fall below 60 BPM during deep sleep. And physically active adults (and athletes) often have a resting heart rate slower than 60 BPM. View an animation of bradycardia.
What is considered slow heart rate?
What’s considered too slow can depend on your age and physical condition. Elderly people, for example, are more prone to bradycardia. In general, for adults, a resting heart rate of fewer than 60 beats per minute (BPM) qualifies as bradycardia.
Can bradycardia be treated?
Borderline or occasional bradycardia may not require treatment. Severe or prolonged bradycardia can be treated in a few ways. For instance, if medication side effects are causing the slow heart rate, then the medication regimen can be adjusted or discontinued.
How to tell if you have bradycardia?
You may not have any symptoms of bradycardia. But if you do have a slow heart rate and any of these symptoms, call your doctor: 1 Syncope/passing out 2 Dizziness 3 Weakness 4 Confusion 5 Heart palpitations/fluttering 6 Feeling short of breath 7 Chest pain 8 Lack of energy
Why do you need a heart monitor?
You will keep track of any symptoms you have. Your doctor will match up the symptoms with the activity on the monitor to see if a heart rhythm problem is the cause and if your heart rate is related to your symptoms.
What does it mean when your heart beats slow?
Bradycardia means your heart rate is slow. This can be completely normal and desirable, but sometimes it can be an abnormal heart rhythm (arrhythmia). If you have bradycardia and you have certain symptoms along with the slow heart rate, then it means your heartbeat is too slow.
What is the purpose of a pacemaker?
A pacemakers is a small device that is placed under your skin to monitor your heart’s rate and rhythm.
Do you need to treat bradycardia?
If you have bradycardia but do not have any symptoms, or if the bradycardia doesn’t happen often or last long, you may not need treatment. Sometimes bradycardia is a good thing and is the goal of treatment. If you need treatment, it will be based on the cause of the condition.
What age is the most likely to develop bradycardia?
In fact, age is the most common risk factor for developing bradycardia. The condition is most common among men and women over age 65. Illness or other conditions also may prompt it. These other causes include: Heart attacks due to coronary artery disease. Bacterial infection in the blood that attacks the heart.
Why does bradycardia happen?
The most common cause for bradycardia is a malfunction in the heart’s natural pacemaker, the sinus node. It controls how quickly the top and bottom heart chambers pump blood through the body. Another cause is atrioventricular block ( AV Block ), in which the top and bottom chambers don’t communicate well and the heart rate drops as a result.
What are the symptoms of slow heart rate?
Consult your doctor if you are experiencing some of these symptoms and you have an associated slow heart rate: Lack of energy. Low stamina.
What happens if your heart rate drops to 30?
If your heart rate drops into the 30s, you might not get enough oxygen to your brain, making fainting, lightheadedness, and shortness of breath possible. Blood can also pool in your heart chambers, causing congestive heart failure.
Is bradycardia a problem?
A low heart rate, called bradycardia, occurs frequently in older adults, cardiologist Jose Baez-Escudero, MD, says. It’s not always a problem, but it does require treatment in some cases. “As people get older, there is occasional normal wear and tear on the electrical system of the heart,” he says.
Is a 60 heart rate good?
For most young people, highly trained athletes, and people who exercise regularly, a below-60 heart rate is normal and healthy. It is very possible to have a slow heart rate and experience no symptoms. However, if you have symptoms but ignore them, it can sometimes cause more serious problems.
Can a pacemaker be implanted to speed up heart rate?
If not, implanting a pacemaker via minimally invasive surgery is the only option to speed up your heart rate, Dr. Baez-Escudero says. He notes that bradycardia isn’t often an emergency, so doctors have time to choose the right treatment.
Perfect Timing
With your help, we’ll turn the tide on heart disease. Your donation brings vital education and research breakthroughs to life — and saves lives.
Symptoms of bradycardia
A heart rate that’s too slow can cause insufficient blood flow to the brain. Symptoms of bradycardia include:
Be inspired and stay informed
Heart Insight® e-news is our trusted, award-winning monthly publication for people living with heart disease, their families and caregivers.
What are the symptoms of bradycardia?
5. Common bradycardia symptoms include: syncope. presyncope. transient dizziness or lightheadedness. fatigue. dyspnea on exertion. heart failure symptoms.
What is bradycardia heart rate?
What is bradycardia? The National Institutes of Health defines bradycardia* as a heart rate <60 bpm in adults other than well-trained athletes. 9 The determination on whether or not treatment is necessary for bradycardic events is generally based on the presence of bradycardia symptoms. The clinical manifestations of bradycardia can vary widely from insidious symptoms to episodes of frank syncope. 5
What percentage of patients with sleep apnea have sinus bradycardia?
The prevalence of sinus bradycardia in patients with sleep apnea can be as high as 40%, with episodes of second- or third-degree AV block in up to 13% of patients. 8
What pharmacologic choice is given for heart pacing?
The two pharmacologic choices are dopamine 2 to 20 mcg/kg/min and/or epinephrine 2 to 10 mcg/min. 1.
When a patient is evaluated for symptomatic bradycardia, an in-depth history and physical is
When a patient is evaluated for symptomatic bradycardia, an in-depth history and physical is important, along with the identification of possible reversible causes. The following is a list of conditions associated with bradycardia and conduction disorders: 11
Can exercise be used to diagnose ischemia?
Exercise Testing. Although not routinely recommended for assessment of ischemia, exercise testing can be considered in patients with symptoms temporally related to exercise, asymptomatic second-degree AV block, or for suspected chronotropic incompetence. 11.
What is the goal of bradycardia therapy?
The goal of therapy for bradycardia or tachycardia is to rapidly identify and treat patients who are hemodynamically unstable. Pacing or drugs, or both, may be used to control symptomatic bradycardia. Cardioversion or drugs, or both, may be used to control symptomatic tachycardia.
What is the first step in the management of tachycardia?
The first step in the management of any tachycardia is to determine if the patient’s condition is stable or unstable (Box 3). An unstable patient with wide-complex tachycardia is presumed to have VT, and immediate cardioversion is performed (Box 4 and see above).
What is irregular narrow complex tachycardia?
An irregular narrow-complex or wide-complex tachycardia is most likely atrial fibrillation with an uncontrolled ventricular response. Other diagnostic possibilities include MAT. We recommend a 12-lead ECG and expert consultation if the patient is stable.
How are tachyarrhythmias classified?
Classification of Tachyarrhythmias. The tachycardias can be classified in several ways based on the appearance of the QRS complex. Professionals at the ACLS level should be able to recognize and differentiate between sinus tachycardia, narrow-complex supraventricular tachycardia (SVT), and wide-complex tachycardia.
What is sinus tachycardia?
Sinus tachycardia is common and usually results from a physiologic stimulus, such as fever, anemia, or shock. Sinus tachycardia occurs when the sinus node discharge rate is >100 times per minute in response to a variety of stimuli or sympathomimetic agents. No specific drug treatment is required.
How long does it take to give adenosine?
Give adenosine rapidly over 1 to 3 seconds through a large (eg, antecubital) vein followed by a 20-mL saline flush and elevation of the arm. If the rate does not convert within 1 to 2 minutes, give a 12-mg bolus. Give a second 12-mg bolus if the rate fails to convert within 1 to 2 minutes after the first 12-mg bolus.
Is a slow heart rate normal?
A slow heart rate may be physiologically normal for some patients, and heart rates >60 beats per minute may be in adequate for others. This bradycardia algorithm focuses on management of clinically significant bradycardia (ie, bradycardia that is inadequate for clinical condition).
