There is no Procedure / Treatment Refusal Acknowledgement form for Minors. Where a parent or guardian is refusing treatment on behalf of a Minor, the Health Practitioner must consider the risk of significant harm arising from the refusal of treatment and the obligations under the Children and Young Persons (Care and Protection) Act 1998. The refusal and steps taken to try to reach agreement about treatment should be documented in the Health Record. Refer to sections 8.4 and 8.5 of this Consent Manual for further guidance.
Full Answer
Can a minor refuse to go to the Doctor?
Aug 09, 2017 · Factors to consider when facing treatment refusals include whether ongoing medical care is needed for a chronic illness vs. providing a one-time treatment; the child’s age and maturity; whether the parents and child agree; likelihood of cure with treatment; likelihood of an adverse event with or without treatment; and reason for refusal, explained Dr. Friedman Ross.
What happens if a hospital refuses to treat a patient?
Illinois allows a mature minor to refuse medical treat-ment, unless that decision threatens the child’s health or welfare; Virginia (the only state to address this issue though legislation) permits a minor 14 years or older to refuse, with parental acquiescence, medical treatment, even when the minor suffers from a life threatening disease.
Can a parent refuse to treat a child?
Apr 08, 2022 · If the child’s parent or legal guardian is unavailable or refuses to agree, the child can still receive inpatient treatment. If the child is under the age of 14, they can petition the court for inpatient admission. If they’re 14 or older, they or someone acting on their behalf can petition the court for inpatient admission.
When should you refuse medical treatment?
WHEN A MINOR MAY CONSENT. While the law has traditionally considered minors to be incompetent to give consent for medical treatment, most states now have statutes that give minors the right to consent to treatment in specific situations. 2 Examples of these are as follows: Court-ordered emancipation.

What can you do if someone refuses medical treatment?
What to Do if Your Loved One Refuses to See a DoctorBe transparent and direct. ... Convince them that it's their idea. ... Make it a "double-checkup" ... Make the rest of the day as enjoyable as possible. ... Get someone who is an authority figure to help.Sep 23, 2015
What are the situations in which a minor is able to refuse treatment and transport for him or herself?
In many states, a minor is allowed to refuse treatment when the parent or guardian is not immediately present. But, the child must have the maturity and intelligence to make an informed choice.Mar 31, 1999
Should minors be able to make medical decisions?
It is essential for minors to participate in medical decision making for treatment and research to the best of their ability, and they must understand that they can refuse without any recrimination. 7 They must also be well aware of what is being asked of them and what will be done to them.
Do doctors violate the children's rights if they do not provide treatment according to the parent's denial to treat the child?
Under the law, children are entitled to protection and appropriate medical treatment despite their parents' religious views. Most states require parents to provide a reasonable degree of medical care for their children. Otherwise, they may face legal consequences, regardless of their religious beliefs.Jan 29, 2021
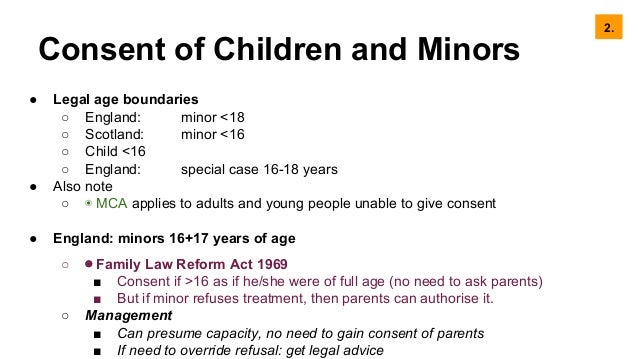
Can 16 and 17 year olds refuse medical treatment?
A young person aged 16-18 cannot refuse treatment if it has been agreed by a person with Parental Responsibility or the Court and it is in their best interests. Therefore, they do not have the same status as adults.May 24, 2021
What are a few examples of when a patient can refuse treatment?
Patients may refuse treatments for many reasons, including financial concerns, fear, misinformation, and personal values and beliefs. Exploring these reasons with the patient may reveal a solution or a different approach.May 24, 2016
Can a 13 year old make their own decisions?
Legally, children can make their own decisions when they reach the age of majority, which is 18 years of age.Oct 28, 2019
Can a 12 year old give consent to medical treatment?
Children under the age of 16 can consent to their own treatment if they're believed to have enough intelligence, competence and understanding to fully appreciate what's involved in their treatment. This is known as being Gillick competent.
Can a 12 year old make their own decisions?
“In some instances, kids 12 and above are developmentally ready to make their own medical decisions, like for vaccines or receiving recommended healthcare treatments where there are harmful consequences if they do not receive them,” she told Healthline.Jun 27, 2019
Can a minor refuse medical treatment in California?
In California, a minor is defined as a person under the age of 18 years. Generally, minors may not consent for medical diagnosis or treatment.
When can a parent parents refuse medical treatment for a child?
The age of majority is 18 years. There is no stipulated age of consent for treatment. Every person (including minors) capable (i.e., able to understand relevant information and reasonably foresee consequences) may give or refuse consent to treatment.Apr 12, 2018
What if parents disagree on medical treatment?
If your child's legal custodian refuses a life-saving or life-improving medication, surgery, vaccine, or other medical procedure and you disagree, you can petition the court for intervention.
What is the right to consent for a minor?
The right to consent by mature minors applies not only to routine care or minor procedures, but most importantly to vital decisions about end-of-life care, resuscitation status, and institution of palliative care [5]. A rough rule of “7s” has evolved as a guide to whether assent or informed consent should be sought from minor patients both in ...
Who is Dr McKinney?
McKinney is following several decades of best practices in caring for older children and adolescents in his “seek [ing] the assent of young patients prior to any invasive exam.”
How old is Micah McKinney's sister?
Dr. McKinney is working in the emergency department when an ambulance arrives with a frantic 12-year-old- girl, Micah, and her 8-year-old sister, Gracie. The paramedic quickly reports that the girls were home alone when Gracie found Micah sitting on the bathroom floor screaming and “covered in blood.” No one has yet been able to contact the girls’ parents. Micah is so frantic that she is unable to give Dr. McKinney any medical history.
What is the EMTALA?
Under federal law, the Emergency Medical Treatment and Active Labor Act (EMTALA) mandates initial evaluation (a medical screening exam) and treatment for all patients presenting to an emergency department with an emergency medical condition. Neither parental nor patient consent or assent is needed for such care.
What is the right of decision making?
Adults with decision-making capacity have a long-recognized and legally protected right to make decisions about their bodies and health, stemming from interest in their autonomy and bodily integrity . This is emphasized by famous cases like Cruzan v.
Who is Valarie Blake?
Valarie Blake, JD, MA is a senior research associate for the American Medical Association Council on Ethical and Judicial Affairs in Chicago. Ms. Blake completed the Cleveland Fellowship in Advanced Bioethics, received her law degree with a certificate in health law and concentrations in bioethics and global health from the University of Pittsburgh School of Law, and obtained a master’s degree in bioethics from Case Western Reserve University. Her research focuses on ethical and legal issues in assisted reproductive technology and reproductive tissue transplants, as well as regulatory issues in research ethics.
Can Jehovah's Witnesses refuse blood transfusions?
The right to refuse life-saving therapies on religious grounds is also strongly defined, most notably the refusal of blood transfusions by Jehovah’s Witnesses [3]. Whether the same rights apply to minors (typically defined as younger than 18, though the definition varies by state) is more complex.
What is the right to refuse medical treatment?
The right to refuse treatment extends to all medical treatment including but not limited to ventilation, cardio-pulmonary resuscitation (CPR), dialysis, antibiotics and artificial feeding and hydration. Treating a person who has validly refused treatment could constitute an assault or battery.
How old is Li?
Li is a 25-year-old who has requested that the hospital cease her life-sustaining treatment including the withdrawal of ventilation. This is expected to lead to Li’s death. Li has been ventilated for over five years but has recently been experiencing frequent and severe respiratory distress and is now unable to leave a hospital environment. Li has been assessed by several specialist Medical Practitioners as having capacity and as having arrived at the decision to refuse treatment in a deliberate and seemingly rational fashion and without any coercion. She has also recorded her wish in writing and provided it to her treating medical team. Li is an adult who has been assessed by appropriate specialists as having capacity to make the decision to refuse life-sustaining treatment and is therefore entitled to do so.
What is an ACD?
Advance Care Directives (ACDs) are a document recording decisions or value statements that describe the person’s future preferences for receiving or refusing specific types of medical treatments. ACDs are to be used when the person loses capacity. An ACD is a type of advance planning tool that may only be completed by a person with decision-making capacity. It is recommended that an ACD be signed by the person.
Do patients with mental illness have the same rights as other patients?
In general, patients experiencing mental ill-health have the same rights with regard to making decisions about end of life care and Advance Care Planning as any other patient. However, the validity of the ACD may be called into question where:
Do medical practitioners have to provide treatment?
Medical Practitioners and other Health Practitioners are under no obligation to provide treatments that in their reasonable opinion are futile, that is, treatment that is unreasonable, offering negligible prospect of benefit to the patient.
Can an ACD be overridden?
Where there is a known, available, and valid ACD, it cannot be overrid den in an emergency. The patient must only receive treatment that is consistent with the ACD. If a patient presents with an ACD or other document that refuses treatment, a copy of the document should be made and placed on the patient’s Health Record.
When Can a Hospital Be Liable for Refusing to Admit or Treat Patients?
As discussed above, there are certain situations where a hospital can be held liable for refusing to admit or treat patients, such as if the hospital is denying treatment based on discriminatory reasons.
Does it Matter Who Refuses to Provide Treatment?
It is important to keep in mind that it matters who the party was that refused a patient treatment. For one, the person refusing to provide medical treatment to the patient must be someone who is employed by the hospital. In addition, that person must also possess the authority to decide which patients can or cannot receive treatment.
Is the Reason for Refusing to Admit or Treat a Patient Important?
In some cases, it may be important to understand the reason as to why a hospital refused to admit or denied treatment to a patient.
How Can a Lawyer Help Me?
If you have suffered further injuries or illness due to being denied admittance or treatment by a hospital, then you should consider contacting a local personal injury lawyer for advice.
What are the rights of a patient who refuses treatment?
In addition, there are some patients who do not have the legal ability to say no to treatment. Most of these patients cannot refuse medical treatment, even if it is a non-life-threatening illness or injury: 1 Altered mental status: Patients may not have the right to refuse treatment if they have an altered mental status due to alcohol and drugs, brain injury, or psychiatric illness. 6 2 Children: A parent or guardian cannot refuse life-sustaining treatment or deny medical care from a child. This includes those with religious beliefs that discourage certain medical treatments. Parents cannot invoke their right to religious freedom to refuse treatment for a child. 7 3 A threat to the community: A patient's refusal of medical treatment cannot pose a threat to the community. Communicable diseases, for instance, would require treatment or isolation to prevent the spread to the general public. A mentally ill patient who poses a physical threat to himself or others is another example.
What is the meaning of refusing treatment at the end of life?
Choosing to refuse treatment at the end of life addresses life-extending or life-saving treatment. The 1991 passage of the federal Patient Self-Determination Act (PSDA) guaranteed that Americans could choose to refuse life-sustaining treatment at the end of life. 9
What is a threat to the community?
A threat to the community: A patient's refusal of medical treatment cannot pose a threat to the community. Communicable diseases, for instance, would require treatment or isolation to prevent the spread to the general public. A mentally ill patient who poses a physical threat to himself or others is another example.
How can a patient's wishes be honored?
Another way for a patient's wishes to be honored is for the patient to have a medical power of attorney. This designates a person to make decisions on behalf of the patient in the event they are mentally incompetent or incapable of making the decision for themselves.
Can a parent refuse treatment?
Children: A parent or guardian cannot refuse life-sustaining treatment or deny medical care from a child. This includes those with religious beliefs that discourage certain medical treatments. Parents cannot invoke their right to religious freedom to refuse treatment for a child. 7 . A threat to the community: A patient's refusal ...
Who is Shereen Lehman?
Shereen Lehman, MS, is a healthcare journalist and fact checker. She has co-authored two books for the popular Dummies Series (as Shereen Jegtvig). Patients often face decisions on whether or not to put themselves through medical treatment. A recommended treatment might only provide comfort or it may speed healing.
Does palliative care extend life?
Palliative care focuses on relieving pain at the end of life but does not help extend life. Before you decide against receiving treatment at the end of your life, be sure you've followed steps to help you to make that informed decision. 10 .
Why can't a doctor treat a patient?
A doctor can refuse to treat a patient because: The doctor’s practice is not accepting new patients. The doctor doesn’t have a working relationship with your health insurance company. The doctor chooses not to treat patients with the illness or injury you suffer from. You can’t pay for the costs of treatment.
What happened to patients who couldn't pay?
Before the enactment of civil and patient’s rights laws, patients who couldn’t pay were often refused treatment or transferred (“dumped”) at public hospitals even when they were in no condition to be moved.
How many people end up in the emergency room every year?
Nearly 137 million people of all ages end up at a hospital emergency room every year. ¹. Federal law requires Medicare-approved hospitals to provide emergency medical treatment to anyone who needs it, even when the person doesn’t have health insurance. Roughly 15 percent of American adults do not have health care coverage.
When should a hospital release you?
Once you’ve been evaluated by a physician, including having any appropriate medical tests, the hospital should not release you until your condition is stable. For example, a woman in active labor cannot be released until the baby has been born and the mother’s condition is stable.
Who sued Providence Hospital?
The family of Marie Moses-Irons sued Providence Hospital and Dr. Paul Lessem for negligence in violation of EMTALA. The lawsuit alleges the hospital was negligent in releasing Moses-Irons’ husband Howard, who murdered his wife ten days after he was released from the hospital.
What is an emergency medical condition?
EMTALA defines an emergency medical condition as one that occurred suddenly, with symptoms such as severe pain, psychiatric disturbance, or symptoms of substance abuse, where lack of emergency care could result in: placing the health of the individual (or unborn child) in serious jeopardy.
Can a private doctor dismiss you?
A private doctor is not subject to the provisions of EMTALA and can dismiss you as a patient at any time, for just about any reason other than discrimination, without fear of liability.