Explore
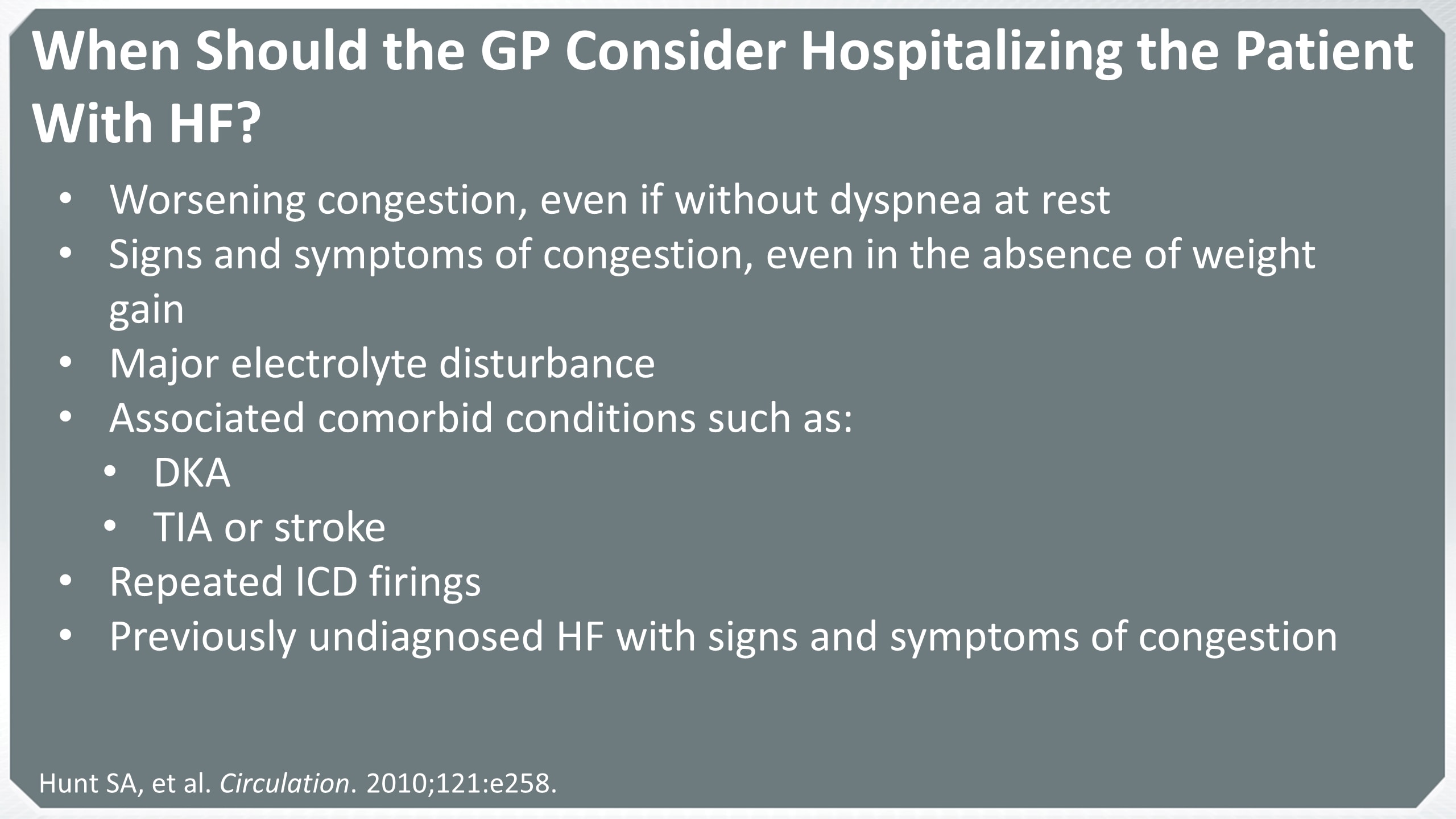
One of the ketone bodies formed (acetone) leaves the body via the lungs, giving the breath of the person with DKA a characteristic, fruity smell. This is how DKA can be detected. DKA can induce coma or even death if not treated immediately. Signs & symptoms of DKA:
What happens If DKA is not treated?
Diabetic Ketoacidosis (DKA) ... Stop IV fluids after 1st meal unless continued dehydration. a. If dehydration, remove dextrose from IV fluid, run NS at 1X maintenance General Guidelines for Meals Under 3 yrs of age – up to 30 gms 3-5 yrs of age – up to 30-45 gms
When to stop fluids DKA?
Management. Children and adolescents with DKA should be managed in a unit that has: Access to laboratory services for frequent and timely evaluation of biochemical variables; Experienced nursing staff trained in monitoring and management of DKA in children and adolescents
How to manage DKA?
Diabetic ketoacidosis is treated with fluids, electrolytes — such as sodium, potassium and chloride — and insulin. Perhaps surprisingly, the most common complications of diabetic ketoacidosis are related to this lifesaving treatment. Possible complications of the treatments.
How is DKA treated?
What is the most important treatment for DKA?
INSULIN THERAPY Modern management of diabetic ketoacidosis has emphasized the use of lower doses of insulin. This has been shown to be the most efficacious treatment in both children and adults with diabetic ketoacidosis.
What do you give a patient in DKA state?
Potassium, bicarbonate, and phosphate therapy If serum potassium decreases to <3.3 mEq/L during DKA treatment, insulin should be stopped and potassium administered intravenously. Small amounts of potassium (20–30 mEq/L) are routinely added to intravenous fluids when serum potassium is between 3.3 and 5.3 mmol/L.
How is DKA treated in ICU?
TREATMENT OPTIONS IN THE ED OR ICU The treatment of acute DKA includes restoration of fluid deficits in the first 24 to 36 h, electrolyte replacement and insulin therapy, which is administered slowly to decreased plasma glucose[23,24].
What IV fluids are given for DKA?
Normal saline (0.9% sodium chloride) is the most commonly used intravenous fluid in treating DKA, but it has a very high concentration of chloride and can lead to additional acid production when given in large volumes.
How to prevent DKA?
Prevent DKA. DKA is a serious condition, but you can take steps to help prevent it: Check your blood sugar often, especially if you’re sick. Keep your blood sugar levels in your target range as much as possible. Take medicines as prescribed, even if you feel fine.
What is DKA in diabetes?
DKA is most common among people with type 1 diabetes. People with type 2 diabetes can also develop DKA. DKA develops when your body doesn’t have enough insulin to allow blood sugar into your cells for use as energy. Instead, your liver breaks down fat for fuel, a process that produces acids called ketones. When too many ketones are produced too ...
What does DKA mean in Spanish?
Español (Spanish) minus. Related Pages. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated right away. Diabetic ketoacidosis (DKA) is a serious complication of diabetes that can be life-threatening. DKA is most common among people with type 1 diabetes.
What causes DKA in diabetics?
Missing insulin shots, a clogged insulin pump, or the wrong insulin dose. Other causes of DKA include: Heart attack or stroke. Physical injury, such as from a car accident. Alcohol or drug use. Certain medicines, such as some diuretics (water pills) and corticosteroids (used to treat inflammation in the body).
Can you test for ketones if you have DKA?
You should also test for ketones if you have any of the symptoms of DKA. Call your doctor if your ketones are moderate or high. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately.
What are the therapeutic goals of DKA?
The therapeutic goals of DKA management include optimization of 1) volume status; 2) hyperglycemia and ketoacidosis; 3) electrolyte abnormalities; and 4) potential precipitating factors. The majority of patients with DKA present to the emergency room. Therefore, emergency physicians should initiate the management of hyperglycemic crisis while a physical examination is performed, basic metabolic parameters are obtained, and final diagnosis is made. Several important steps should be followed in the early stages of DKA management: 1 collect blood for metabolic profile before initiation of intravenous fluids; 2 infuse 1 L of 0.9% sodium chloride over 1 hour after drawing initial blood samples; 3 ensure potassium level of >3.3 mEq/L before initiation of insulin therapy (supplement potassium intravenously if needed); 4 initiate insulin therapy only when steps 1–3 are executed.
Why is bicarbonate not indicated in mild and moderate forms of DKA?
Bicarbonate therapy is not indicated in mild and moderate forms of DKA because metabolic acidosis will correct with insulin therapy.3, 8The use of bicarbonate in severe DKA is controversial due to a lack of prospective randomized studies.
How many hospitalizations for diabetic ketoacidosis in 2009?
In 2009, there were 140,000 hospitalizations for diabetic ketoacidosis (DKA) with an average length of stay of 3.4 days.1The direct and indirect annual cost of DKA hospitalizations is 2.4 billion US dollars.
What is the name of the regimen that contains both long-acting and short-acting insulin?
The regimen containing both long-acting and short-acting insulin is called a basal-bolus insulin regimen; it provides physiological replacement of insulin. If a patient used insulin prior to admission, the same dose can be restarted in the hospital.
Is ketoacidosis a type 1 or 2 diabetes?
Diabetic ketoacidosis (DKA) is a rare yet potentially fatal hyperglycemic crisis that can occur in patients with both type 1 and 2 diabetes mellitus. Due to its increasing incidence and economic impact related to the treatment and associated morbidity, effective management and prevention is key. Elements of management include making ...
Can DKA cause hypokalemia?
A “normal” plasma potassium concentration still indicates that total body potassium stores are severely diminished, and the institution of insulin therapy and correction of hyperglycemia will result in hypokalemia.
What is the most common electrolyte derangement that occurs during the treatment of DKA?
Significant hypokalaemia is the most common life threatening electrolyte derangement that occurs during the treatment of DKA. Intravenous potassium replacement will be required after insulin is given as potassium will move into cells. Potassium replacement should not be started before insulin treatment; extracellular levels may otherwise rise dangerously high. Potassium replacement should be given as soon as insulin and fluid are started and the [K] level is known to be below the upper limit of the reference range. Regimens for potassium supplementation have not been formally evaluated. One suitable regimen for potassium replacement has been proposed 10:
Does phosphate affect DKA?
Phosphate levels are affected in DKA in much the same way as potassium (that is, extracellular shift but depleted total body levels). A small study found that the addition of phosphate to standard treatment did not reduce the time taken to reach recovery indices of bicarbonate, pH, or glucose. 16 Differences in magnesium and 2,3DPG levels and in P50 (the Pa o2 at which haemoglobin is 50% saturated) were not statistically significant. In another study phosphate supplementation (15 or 45 mmol) did not affect the rate of correction of [glucose], [bicarbonate] or pH. 17
Is diabetic ketoacidosis fatal?
Diabetic ketoacidosis (DKA) is a potentially fatal metabolic disorder presenting most weeks in most accident and emergency (A&E) departments. 1 The disorder can have significant mortality if misdiagnosed or mistreated. Numerous management strategies have been described. Our aim is to describe a regimen that is based, as far as possible, ...
Is DKA a life threatening disease?
DKA is a complex life threatening problem and the management should not be left to inexperienced staff. There should be early consultation between A&E staff and specialist diabetes teams. Patients with DKA need four things;
Is DKA a clinical diagnosis?
There are no specific clinical signs that confirm or refute the diagnosis of DKA. The diagnosis is comparatively straight forward where there is a clear history that the patient has diabetes but can cause serious diagnostic difficulty where the patient is unconscious or DKA is the first presentation of diabetes (a past history of diabetes mellitus will be absent in 1 in 10 patients). The possibility of DKA (or other metabolic acidosis) should be considered whenever assessing a patient who presents with “hyperventilation” 4 and it is always essential to measure the blood glucose early in the resuscitation of any unconscious patient.
Is DKA the first presentation of diabetes?
DKA may be the first presentation of diabetes. Insulin error (with or without intercurrent illness) is the most common precipitating factor, accounting for nearly two thirds of cases (excluding those where DKA was the first presentation of diabetes mellitus). 2
When do you need insulin?
You may need to take insulin until your blood sugar level becomes normal. Glucose may be needed when your blood sugar level begins to decrease. This is to prevent your blood sugar level from dropping too quickly while you are getting insulin. Potassium may be given if your blood levels of potassium are low.
How does a dietitian help you?
They will also teach you how to dispose of needles and syringes. About nutrition: A dietitian will help you make a meal plan to keep your blood sugar level steady. You will learn how food affects your blood sugar levels. You will also learn to keep track of sugar and starchy foods (carbohydrates). Do not skip meals.
Can DKA cause a coma?
This can cause abnormal heartbeats. Blood flow may be decreased and cause organ failure. Decreased blood flow to your brain may lead to seizures, swelling, or a coma. Treatment may cause your blood sugar level to become too low. Very low blood sugar levels may cause seizures, or you may become unconscious. Too much fluid replacement may cause trouble breathing or cerebral edema (water around the brain). DKA can be life-threatening.