In addition, the basal heart rate of these patients was significantly higher compared to the control group (81/min vs. 73/min). After administration of 2 and 4 micrograms/kg of atropine the patients of the control group showed a 5% resp. 4% decrease in heart rate. 26% of these patients developed conduction disturbvances.
Full Answer
What effect does atropine have on heart rate?
The use of atropine in cardiovascular disorders is mainly in the management of patients with bradycardia. Atropine increases the heart rate and improves the atrioventricular conduction by blocking the parasympathetic influences on the heart.
Why does atropine slow down the heart ratw?
When atropine is introduced to heart cells, it blocks them from being activated by acetylcholine released from the vagus nerve. In the medical setting, atropine is most commonly used to block the effects of too much vagal stimulation. In other words, administering atropine helps counteract an abnormally slow heart rate.
How can low dose atropine decrease heart rate?
One of the effects of atropine on the heart, the slowing of the heart rate at low dosages, occurs through central vagal stimulation. The parasympathetic vagus nerve serves to lower the heart rate. Atropine allows the sympathetic nerve to increase its dominance over the parasympathetic.
Does atropine raise blood pressure?
Most cases occurred shortly after atropine, i.e. before anaesthesia. Heart rate increased significantly in both groups, more so after atropine (up to 60%), and remained elevated. In both groups blood pressure fell after the induction of anaesthesia but was close to control during surgery.

How much does atropine increase heart rate?
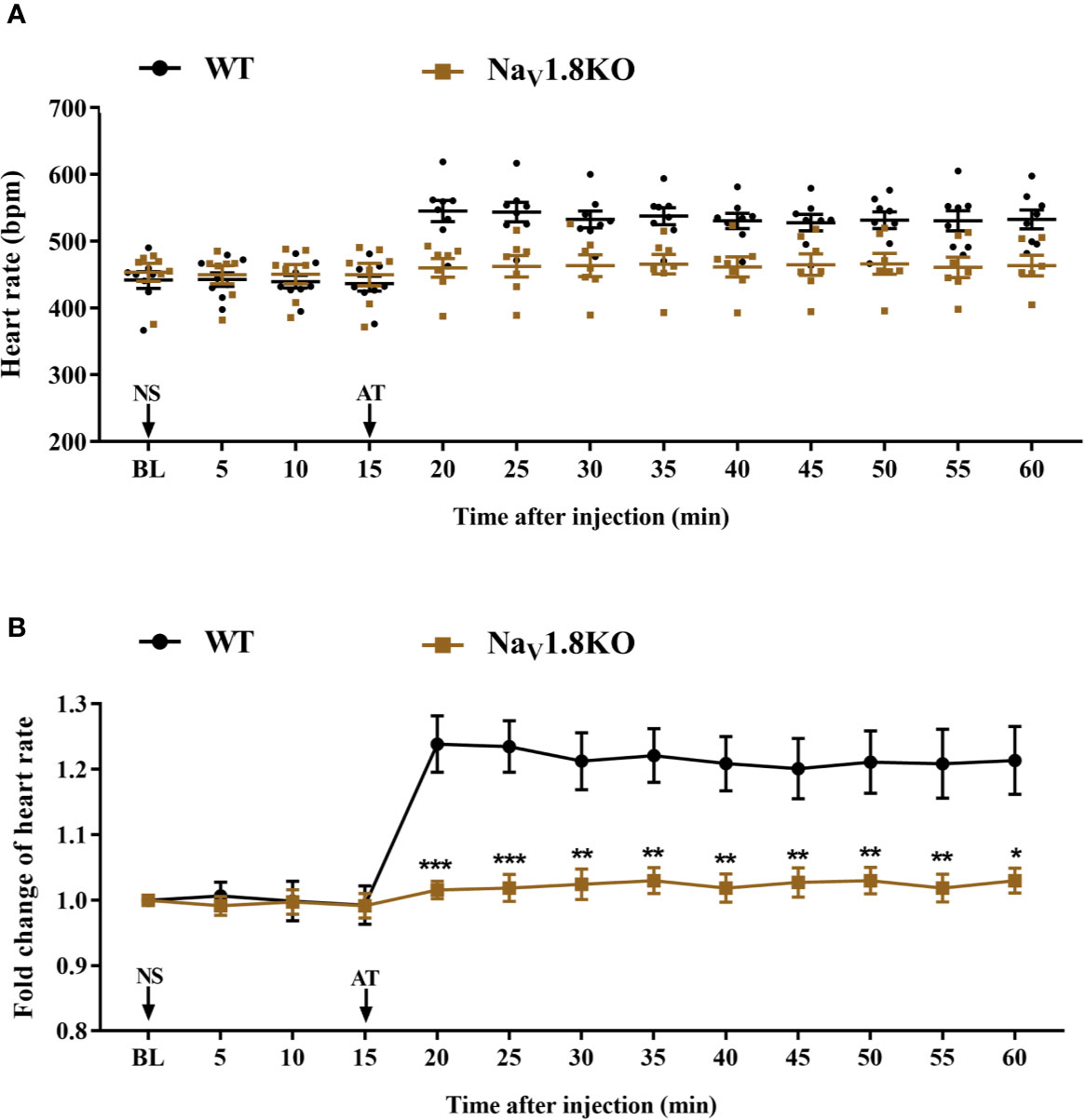
We studied the effect of atropine on heart rate in explanted perfused mouse hearts (ex vivo Langendorff preparation) which lack any nervous innervation. As expected, a low dose of ISO increased the basal heart rate by ~10%.
Does atropine cause decrease heart rate?
Low-dose atropine slows heart rate but does not change overall levels of MSNA. High-dose atropine causes a decrease in MSNA and tachycardia.
Does atropine increase heart rate and blood pressure?
of atropine was given intravenously (I.V.) TO 123 ANESTHETIZED PATIENTS. Increases in heart rate were seen in 109 patients (88 percent), while 7 patients (5.7 percent) had no change. A mean increase in systolic arterial blood pressure of 14 mm.
How long does atropine last for bradycardia?
The recommended atropine dose for bradycardia is 0.5 mg IV every 3 to 5 minutes to a maximum total dose of 3 mg. Doses of atropine sulfate of <0.5 mg may paradoxically result in further slowing of the heart rate.
When does atropine stop?
Atropine should be avoided with bradycardia caused by hypothermia and, in most cases, it will not be effective for Mobitz type II/Second-degree block type 2 or complete heart block.
Does atropine increase cardiac output?
Two milligrams of atropine given intravenously increased the cardiac output, the mean arterial pressure, and the heart rate and lowered the central venous pressure, stroke output, and peripheral resistance.
Why atropine causes initial bradycardia?
Background: Low-dose atropine causes bradycardia either by acting on the sinoatrial node or by its effects on central muscarinic receptors increasing vagal activity.
Does atropine cause hypotension?
Atropine blocked the pressor responses to norepinephrine and shifted the dose-response curve for norepinephrine to the right to a similar extent in spontaneously hypertensive and Wistar-Kyoto rats. Thus, atropine acts as a competitive antagonist of norepinephrine and this action underlies its hypotensive effect.
What are the side effects of atropine?
These include dryness of the mouth, blurred vision, dry eyes, photophobia, confusion, headache, dizziness, fatigue, tachycardia, palpitations, flushing, urinary hesitance or retention, constipation, abdominal pain, abdominal distention, nausea, vomiting, loss of libido, and impotency.
What is the best treatment for low heart rate?
Bradycardia treatment may include lifestyle changes, medication changes or an implanted device called a pacemaker. If an underlying health problem, such as thyroid disease or sleep apnea, is causing the slow heart rate, treatment of that condition might correct bradycardia.
When does bradycardia require a pacemaker?
Your doctor may recommend a temporary pacemaker when you have a slow heartbeat (bradycardia) after a heart attack, surgery or medication overdose but your heartbeat is otherwise expected to recover. A pacemaker may be implanted permanently to correct a chronic slow or irregular heartbeat or to help treat heart failure.
Why does atropine worsen heart block?
Since the actions of atropine are to block the binding of acetylcholine to muscarinic receptors, thereby (a) reducing vagal input at the SA node, and (b) increasing conduction velocity through the AV node, the thought is that atropine would be a poor choice for reducing oxygen demand in heart-block therapy when an MI ...
Does atropine help with bradycardia?
The use of atropine in cardiovascular disorders is mainly in the management of patients with bradycardia. Atropine increases the heart rate and improves the atrioventricular conduction by blocking the parasympathetic influences on the heart. Recent observations that atropine in low doses results in ….
Does atropine increase heart rate?
Atropine increases the heart rate and improves the atrioventricular conduction by blocking the parasympathetic influences on the heart. Recent observations that atropine in low doses results in paradoxical effects at the sinoatrial node (vagotonic) and the atrioventricular node (vagolytic) have lead to a concern for its safety in patients ...
How does atropine help with tachycardia?
Atropine reduces excretion in the mouth, respiratory passages, relieves spasms and the constriction of the respiratory passages. Atropine can also diminish the paralysis of respiration resulting from the actions of toxic agents on the central nervous system prior to surgery. Atropine-induced parasympathetic is especially useful on the heart, where tachycardia develops due to paralysis of vagal control. Small doses of atropine slow down the heart rate before characteristic tachycardia develops. It is also used to treat spasms in the intestines, stomach, and other organs. It can also be used as an anticholinergicby blocking the effects of acetylcholinein the stomach, intestines, nervous system, urinary tract, certain glands, and other tissues.
What are the side effects of atropine?
A suggested mnemonic for remembering the systemic activity and side effects of atropine is hot as a hare, red as a beet, dry as a bone, blind as a bat, mad as a hatter.8 More significant cases of systemic atropine poisoning can cause drowsiness, central nervous depression, circulatory collapse with respiratory failure and death.8 Whilst atropine-related deaths are rare, due to the high metabolic excretion rate, a dose of as little 10mg can be fatal: or the oral ingestion of 20 drops of a 1% atropine solution.8 A case of this occurring in America8 highlights that whilst the safety profile of the eye drop is good, medication should be stored safely, properly and far out of the reach of children.
How does atropine work?
Atropine works by poisoning the vagus nerve, thereby;removing parasympathetic inputs to the heart. ;This works beautifully for vagally-mediated bradycardia . ;However, it fails for bradycardias caused by other mechanisms . ;Overall, atropine is completely effective in only 28% of patients with symptomatic bradycardia .
What is atropine used for?
Specific Drugs and Therapeutic Indications Atropine is a muscarinic receptor antagonist that is used to inhibit the effects of excessive vagal activation on the heart, which is manifested as sinus bradycardia and AV nodal block.
Does atropine cause sinus bradycardia?
Atropine is a muscarinic receptor antagonist that is used to inhibit the effects of excessive vagal activation on the heart, which is manifested as sinus bradycardia and AV nodal block. Therefore, atropine can temporarily revert sinus bradycardia to normal sinus rhythm and reverse AV nodal blocks by removing vagal influences.
How to treat unstable symptomatic bradycardia?
There are three ways to treat unstable symptomatic bradycardia: increase the blood pressure by increasing fluid volume in the cardiovascular system, constricting peripheral blood vessels to push blood toward vital organs, or increased heart rate. The most successful treatment uses a combination of all three.
Is atropine effective for Mobitz II?
In your AHA provider manual, you will see it stated in the bradycardia section that atropine is not effective for Mobitz II and complete heart block. I have had a number of people ask why it is not effective. Read below for the explanation.
What is atropine used for?
Atropine, which is on the WHO List of Essential Medicines, is a non-selective muscarinic receptor inhibitor used to treat acute sinus node dysfunction associated with bradycardia, complete atrio ventricular block, and organophosphate and beta-blocker poisoning. Therefore, atropine is widely used for resuscitation and emergency cardiovascular care4as well as for critical care intubation in neonates and to decrease salivation prior to some surgeries5. In the heart, atropine blocks the inhibitory effect of ACh on heart rate and contractility, potentially also leading to tachyarrhythmias6. These and other prominent effects of atropine have been exclusively attributed to its antagonism at muscarinic receptors7,8. However, paradoxical actions of this drug on cardiovascular system and a plethora of side-effects ranging from anticholinergic up to less well-explicable nausea and paradoxical bradycardia seem to rely on more than one classical mechanism of action6.
Is PDE4 inhibitory or inotropic?
PDE4 inhibition is involved in atropine induced positive inotropic and chronotropic effects in vitroand in vivo
Does atropine increase contractile force?
Myocardial cAMP augmentation should not only lead to an increase in heart rate but also to increased contractile force. Sarcomere shortening measurements in isolated ventricular cardiomyocytes showed that atropine also enhanced the positive inotropic effect of ISO (Fig. 3f,g). This experiments support the concept that even in absence of parasympathetic innervation in isolated cardiomyocytes or explanted hearts, atropine increases cAMP levels and cardiac contractility by inhibiting PDEs.
Does atropine inhibit PDE4?
Atropine inhibits PDE4 activity. (a) Single-cell FRET analysis of PDE4 inhibition in HEK293A cells expressing the Epac1-camps-PDE4 sensor. Cells were prestimulated with 1 µM ISO for 3 min before adding atropine (10 nM) and rolipram (10 µM) to pre-elevate intracellular cAMP levels. (b) Quantification of the data shown in aas a % change of the FRET ratio in response to atropine along with maximal effects measured by these sensors with respective inhibitors, mean ± s.e.m. (n = 6). Atropine inhibits cAMP-PDE activity in cardiomyocyte lysates (c) and recombinant PDE4D3 from transfected HEK293 cells (d), as measured by a classical in vitroPDE assay (n = 3–5). The basal PDE activity is represented by the “IBMX” bar in cor “PDE4” bar (rolipram-sensitive activity of PDE4D3 transfected minus vector-transfected control [Co] cell lysates, a representative immunoblot for PDE4D3 is shown) in (d.) *p < 0.05 compared to basal PDE activity by one-way ANOVA. (e) Preincubation of cardiomyocytes with 10 µM rolipram prevents the atropine (10 nM) mediated increase of cAMP after ISO stimulation (3 nM to avoid sensor saturation by rolipram). Representative experiment (n = 6), data analysis is in f. (g) preincubation of cells with 30 µM 8-MMX to block PDE1 (n = 6), 100 nM of the PDE2 inhibitor BAY 60–7550 (n = 6) or 10 µM of the PDE3 inhibitor cilostamide (n = 7) under the same experimental conditions (except for 100 nM ISO used to prestimulate cAMP levels) did not abolish the effect of atropine. *p < 0.05, **p < 0.01, n.s. – not significant by paired t-test.
Does atropine increase cAMP?
Here, we use various in vitroand in vivotechniques to test the hypothesis that atropine can inhibit the activity of cAMP hydrolysing phosphodiesterases (PDEs), thereby increasing intracellular cAMP levels. We found that atropine, independently of its effect on muscarinic receptors, can inhibit PDE4 activity, leading to augmented cardiac contractility after β-adrenergic stimulation. This new receptor-independent mechanism may explain many of the pharmacological actions and side-effects of this classical cardiovascular drug.
Does atropine block muscarinic receptors?
In summary, we show that the clinically relevant drug atropine does not only block muscarinic receptors but also directly inhibits the enzymatic activity of PDEs, in particular the cAMP-specific PDE4. This new mechanism accounts for increased cAMP levels in cardiomyocytes which might play a crucial role in mediating various side-effects of atropine, especially arrhythmogenesis. We show that PDE inhibition by atropine promotes an increase in intracellular cAMP, which in turn leads to an elevated heart rate and increased contractility. This effect of atropine is clearly independent of M1/2/3-muscarinic receptors and does not involve its classical anticholinergic activity. The atropine-mediated increase in contractility by PDE4 inhibition is predicted to be especially important under adrenergic stress, which occurs either due to increased endogenous catecholamine levels in heart failure8, severe infections, myocardial infarction or during diagnostic procedures such as the dobutamine atropine stress echocardiography in a perioperative setting30. Since the stimulatory effect of atropine on cAMP production is only observed under catecholamine stress, it can be expected that therapeutically used β-blockers might effectively counteract atropine-induced arrhythmias associated with PDE inhibition.