Hypokalemia iscommon during the treatment of diabetic ketoacidosis(DKA); however, severe hypokalemiaat presentation prior to insulin treatment isexceedingly uncommon. After insulin treatment isinitiated, potassium shifts intracellularly andserum levels decline. Also, do you have hyperkalemia with DKA?
How is hyperkalemia treated in diabetic ketoacidosis (DKA)?
Rapid hemodialysis along with intensive insulin therapy can improve hyperkalemia, while fluid infusions may worsen heart failure in patients with ketoacidosis who routinely require hemodialysis. Background Diabetic ketoacidosis (DKA) is a very common endocrinology emergency.
Is hypokalemia associated with severe diabetic ketoacidosis?
Profound Hypokalemia Associated With Severe Diabetic Ketoacidosis Go to: Abstract Hypokalemia is common during the treatment of diabetic ketoacidosis (DKA); however, severe hypokalemia at presentation prior to insulin treatment is exceedingly uncommon.
Should potassium be given orally or intravenously for hypokalemia?
Whether oral or intravenous potassium will be administered, this should be decided according the severity of the hypokalemia. It is important to remember that every 1 mEq/L decrease in serum potassium, represents a potassium deficit of approximately 200–400 mEq.
How does DKA cause hyperglycemia?
These hormonal alterations in DKA and HHS lead to increased hepatic and renal glucose production and impaired glucose utilization in peripheral tissues, which result in hyperglycemia and parallel changes in osmolality of the extracellular space (12,13).
Does DKA have hypokalemia or hyperkalemia?
DKA is a well-known cause of hypokalemia caused by osmotic diuresis leading to a total body potassium deficiency of 3 to 6 mEq/kg. At presentation, potassium levels are typically “normal” due to the extracellular shift of potassium (K+) from insulin deficiency and acidosis.
Do you treat hyperkalemia in DKA?
Although DKA may present with hypokalemia, rapid hemodialysis may be necessary to resolve severe hyperkalemia in a patient with renal failure.
Do DKA patients have hyperkalemia?
Abstract. Patients with diabetic ketoacidosis tend to have somewhat elevated serum K+ concentrations despite decreased body K+ content. The hyperkalemia was previously attributed mainly to acidemia.
How is hypokalemia treated in DKA?
Potassium replacement should be started with initial fluid replacement if potassium levels are normal or low. Add 20-40 mEq/L of potassium chloride to each liter of fluid once the potassium level is less than 5.5 mEq/L. Potassium can be given as follows: two thirds as KCl, one third as KPO4.
What is the most appropriate treatment for DKA?
Insulin therapy. Insulin reverses the processes that cause diabetic ketoacidosis. In addition to fluids and electrolytes, you'll receive insulin therapy — usually through a vein.
Why does DKA need potassium?
Replacement of potassium in intravenous fluids is the standard of care in treatment of DKA to prevent the potential consequences of hypokalemia including cardiac arrhythmias and respiratory failure.
Does insulin cause hypokalemia or hyperkalemia?
Insulin therapy lowers K+ concentration driving K+ into cells (both directly and indirectly by reversing hyperglycemia). Therefore, insulin therapy may cause severe hypokalemia, particularly in patients with a normal or low serum K+ concentration at presentation.
Does acidosis cause hypokalemia?
Although there are exceptions,72 these patients generally have hypokalemia caused by renal K+ wasting during chronic acidosis, which is corrected by base administration.
Why is there hyperkalemia in acidosis?
Thus, these results identify that hyperkalemia can be the direct cause of metabolic acidosis from its effects on multiple components of renal ammonia metabolism. The first major finding in these studies is that hyperkalemia itself causes reversible metabolic acidosis by inhibiting ammonia excretion.
When should you treat hyperkalemia?
If the hyperkalemia is severe (potassium >7.0 mEq/L) or if the patient is symptomatic, begin treatment before diagnostic investigation of the underlying cause. Individualize treatment in accordance with the patient's presentation, potassium level, and electrocardiographic findings.
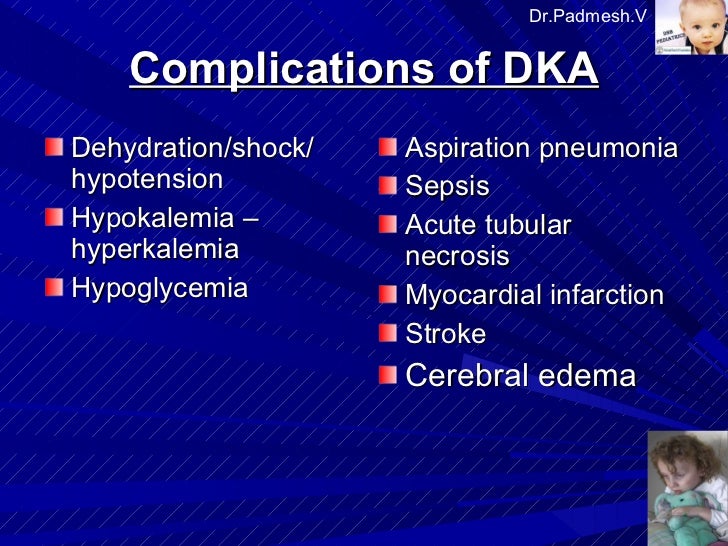
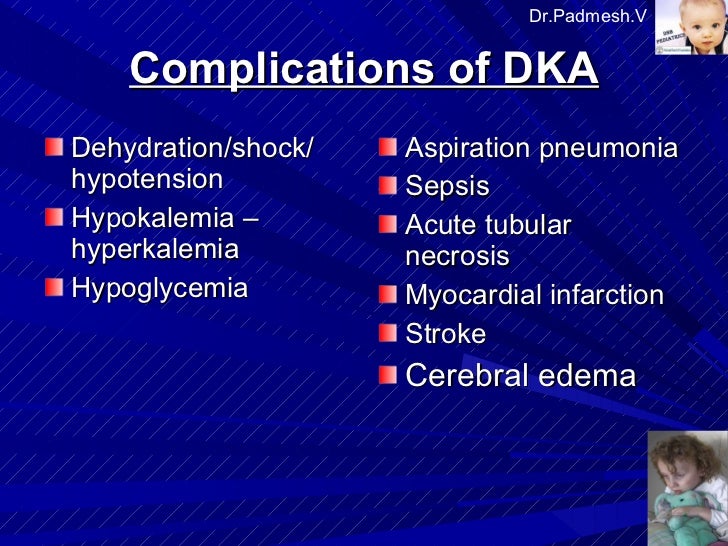
What is DKA and how is it treated?
Diabetic ketoacidosis is treated with fluids, electrolytes — such as sodium, potassium and chloride — and insulin. Perhaps surprisingly, the most common complications of diabetic ketoacidosis are related to this lifesaving treatment.
When do you give potassium DKA?
About two-thirds of patients will develop hypokalemia in the course of treatment for DKA. Potassium repletion should commence once the serum potassium falls below 5.3 mEq/L if patients have normal renal function. Twenty to 30 mEq of potassium may be supplemented to each liter of fluids.
How do we treat hyperkalemia?
Drugs used in the treatment of hyperkalemia include the following:Calcium (either gluconate or chloride): Reduces the risk of ventricular fibrillation caused by hyperkalemia.Insulin administered with glucose: Facilitates the uptake of glucose into the cell, which results in an intracellular shift of potassium.More items...•
Why is hyperkalemia associated with acidosis?
Conclusions Hyperkalemia decreases proximal tubule ammonia generation and collecting duct ammonia transport, leading to impaired ammonia excretion that causes metabolic acidosis.
Does insulin cause hypokalemia or hyperkalemia?
Insulin therapy lowers K+ concentration driving K+ into cells (both directly and indirectly by reversing hyperglycemia). Therefore, insulin therapy may cause severe hypokalemia, particularly in patients with a normal or low serum K+ concentration at presentation.
How is Hypernatremia treated in DKA?
Treating the DKA more aggressively than the hypernatremia itself, choosing a hypoosmolar fluid, and switching to D5-0.45% saline, when glucose has decreased, are some of the vital considerations for the management of hypernatremia in DKA.