Medication
Mar 25, 2021 · Diabetic Ketoacidosis. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated right away. Diabetic ketoacidosis (DKA) is a serious complication of diabetes that can be life-threatening. DKA is most common among people with type 1 diabetes. People with type 2 diabetes can also develop DKA.
Therapy
May 01, 2003 · Administering hypertonic dextrose (1 litre 10% dextrose + 40 units insulin at 250 ml/h) rather than isotonic dextrose (1 litre 5% dextrose + 10 units insulin at 250 ml/h) may accelerate the clearance of ketone bodies but also causes a rise in [glucose] without an additional improvement in blood pH or bicarbonate. 8 Insulin Type of insulin
Self-care
Jun 30, 2014 · early investigations assessing optimal insulin doses and administration route in the treatment of dka demonstrated that subcutaneous delivery of regular insulin is effective but inferior to the intravenous insulin infusion. 13 the approval of rapid-acting insulin analogs (aspart, glulisine, and lispro) offered new paradigms in the management of …
Nutrition
Jan 11, 2018 · Other study shows people with diabetes prefer combination of insulin aspart and FlexPen® by more than eight-to-one over other rapid-acting insulin and pen delivery device New Orleans, LA June 14, 2003 — Treatment of diabetic ketoacidosis with the rapid-acting human insulin analog insulin aspart (rDNA origin) injection (brand name, NovoLog®), instead of with …
How dangerous is ketoacidosis?
Dec 31, 2017 · Background Rapid-acting insulin analogues (artificial insulin such as insulin lispro, insulin aspart, or insulin glulisine) act more quickly than regular human insulin. In people with a specific type of life-threatening diabetic coma due to uncontrolled diabetes, called diabetic ketoacidosis, prompt administration of intravenous regular insulin is standard therapy.
How to diagnosis diabetic ketoacidosis?
May 04, 2013 · Subcutaneous lispro and IV regular insulin treatments are equally effective and safe for the treatment of mild and moderate DKA in adult patients; Ersoz et al. The International Journal of Clinical Practice Mar 2006. Click Image to Enlarge Click Image to Enlarge PREV NEXT
What are symptoms of ketoacidosis if you have diabetes?
May 20, 2021 · the most recent guidelines from the american diabetes association recommend administration of a bolus of iv insulin (0.1 u/kg) prior to starting a continuous iv insulin infusion, although it should be noted that these guidelines have not been updated since 2009 and the use of insulin bolus in adult patients with dka has become controversial in …
Do I have to treat diabetic ketoacidosis?
Aug 01, 2004 · The mainstay in the treatment of DKA involves the administration of regular insulin via continuous intravenous (IV) infusion or by frequent subcutaneous (SC) or intramuscular (IM) injections ( 3, 4, 5 ).

What type of insulin is used for ketoacidosis?
The mainstay in the treatment of DKA involves the continuous intravenous (IV) infusion of regular insulin or the frequent subcutaneous (SC) injections of regular or rapid-acting insulin analogs.
What is the emergency treatment of diabetic ketoacidosis?
If you're diagnosed with diabetic ketoacidosis, you might be treated in the emergency room or admitted to the hospital. Treatment usually involves: Fluid replacement. You'll receive fluids — either by mouth or through a vein — until you're rehydrated.Nov 11, 2020
Which insulin is given in emergency?
Critically ill patients may be given insulin, with a loading dose of regular insulin (0.1 units/kg body weight to a maximum of 10 units), followed by an infusion of regular insulin (0.1 units/kg body weight/hour, to a maximum of 10 units/hour)15,16.Mar 1, 2014
How much insulin do you give for ketoacidosis?
A mix of 24 units of regular insulin in 60 mL of isotonic sodium chloride solution usually is infused at a rate of 15 mL/h (6 U/h) until the blood glucose level drops to less than 180 mg/dL; the rate of infusion then decreases to 5-7.5 mL/h (2-3 U/h) until the ketoacidotic state abates.Jan 19, 2021
Why is regular insulin used for diabetic ketoacidosis?
Insulin administration is essential in DKA treatment because it promotes glucose utilization by peripheral tissues, diminishes glycogenolysis and gluconeogenesis, and suppresses ketogenesis. Intravenous infusion is a preferred route of insulin delivery in patients with DKA.Jun 30, 2014
What is glucagon emergency kit used for?
At home, school or work, the Glucagon Emergency Kit is convenient and simple to use. This injection is administered under the skin to quickly treat patients with diabetes who experience unexpected episodes of severe hypoglycemia. In the event of a severe hypoglycemic episode, you will be unable to treat yourself.
When should emergency insulin be given?
If their ketones are high, they should call their doctor. If they have serious signs, take them to the emergency room or urgent care right away....The person may have:Not injected enough insulin, or needs more than usual.Not eaten enough food.Had an insulin reaction (low blood sugar) while they were sleeping.Nov 6, 2020
What medication is used for emergency hyperglycemia?
Glucagon—a hormone that raises blood sugar levels—is used to treat severe hypoglycemia. Glucose is taken as a spray into the nose or an injection administered under the skin. If you use insulin or a sulfonylurea to manage your diabetes, it's a good idea to keep a glucagon kit with you in case of emergencies.
How to prevent DKA?
Prevent DKA. DKA is a serious condition, but you can take steps to help prevent it: Check your blood sugar often, especially if you’re sick. Keep your blood sugar levels in your target range as much as possible. Take medicines as prescribed, even if you feel fine.
What causes DKA in diabetics?
Missing insulin shots, a clogged insulin pump, or the wrong insulin dose. Other causes of DKA include: Heart attack or stroke. Physical injury, such as from a car accident. Alcohol or drug use. Certain medicines, such as some diuretics (water pills) and corticosteroids (used to treat inflammation in the body).
What is a DKA?
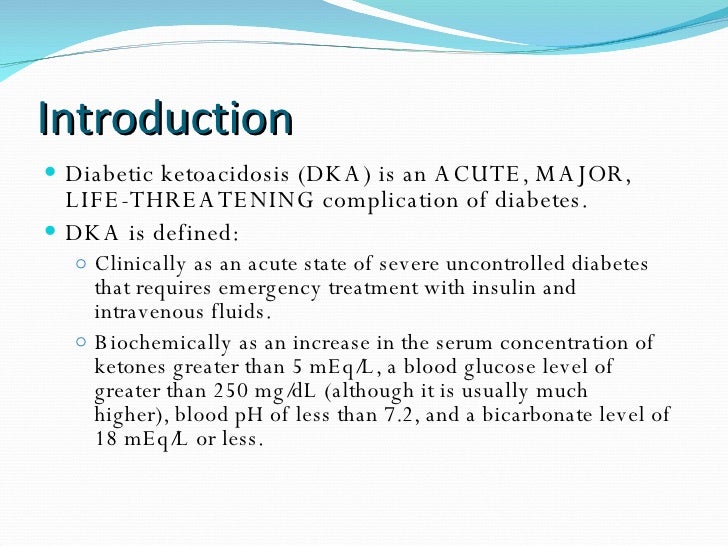
Diabetic ketoacidosis (DKA) is a serious complication of diabetes that can be life-threatening. DKA is most common among people with type 1 diabetes. People with type 2 diabetes can also develop DKA. DKA develops when your body doesn’t have enough insulin to allow blood sugar into your cells for use as energy.
What to do if your ketones are high?
Call your doctor if your ketones are moderate or high. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately. Go to the emergency room or call 911 right away if you can’t get in touch with your doctor and are experiencing any of the following:
What happens when you have too many ketones?
When too many ketones are produced too fast, they can build up to dangerous levels in your body. Read on to learn more about DKA, how you can prevent DKA, and how to treat it if needed.
What is the most common electrolyte derangement that occurs during the treatment of DKA?
Significant hypokalaemia is the most common life threatening electrolyte derangement that occurs during the treatment of DKA. Intravenous potassium replacement will be required after insulin is given as potassium will move into cells. Potassium replacement should not be started before insulin treatment; extracellular levels may otherwise rise dangerously high. Potassium replacement should be given as soon as insulin and fluid are started and the [K] level is known to be below the upper limit of the reference range. Regimens for potassium supplementation have not been formally evaluated. One suitable regimen for potassium replacement has been proposed 10:
What are the symptoms of insulin resistance?
Polyuria, polydipsia, and weakness are usually present. Nausea, vomiting, or abdominal pain may predominate. If the patient is already being treated with insulin, there may be a history of reduced or omitted insulin.
Is DKA the first presentation of diabetes?
DKA may be the first presentation of diabetes. Insulin error (with or without intercurrent illness) is the most common precipitating factor, accounting for nearly two thirds of cases (excluding those where DKA was the first presentation of diabetes mellitus). 2
Is DKA a clinical diagnosis?
There are no specific clinical signs that confirm or refute the diagnosis of DKA. The diagnosis is comparatively straight forward where there is a clear history that the patient has diabetes but can cause serious diagnostic difficulty where the patient is unconscious or DKA is the first presentation of diabetes (a past history of diabetes mellitus will be absent in 1 in 10 patients). The possibility of DKA (or other metabolic acidosis) should be considered whenever assessing a patient who presents with “hyperventilation” 4 and it is always essential to measure the blood glucose early in the resuscitation of any unconscious patient.
Is DKA a life threatening disease?
DKA is a complex life threatening problem and the management should not be left to inexperienced staff. There should be early consultation between A&E staff and specialist diabetes teams. Patients with DKA need four things;
Does bicarbonate help with acidosis?
Severe acidosis has adverse effects on many organs, especially the brain and the heart. It may, therefore, seem appealing to give bicarbonate as treatment for the metabolic acidosis that occurs in DKA. There is no evidence to support this. Studies (not RCTs) have failed to find evidence of faster biochemical recovery with bicarbonate treatment even in severely patients. 11–14 One prospective study found no metabolic benefits from bicarbonate administration and that bicarbonate (1 litre 150 mM sodium bicarbonate over one hour) delayed the fall in total ketone bodies and lactate levels. 15
Does phosphate affect DKA?
Phosphate levels are affected in DKA in much the same way as potassium (that is, extracellular shift but depleted total body levels). A small study found that the addition of phosphate to standard treatment did not reduce the time taken to reach recovery indices of bicarbonate, pH, or glucose. 16 Differences in magnesium and 2,3DPG levels and in P50 (the Pa o2 at which haemoglobin is 50% saturated) were not statistically significant. In another study phosphate supplementation (15 or 45 mmol) did not affect the rate of correction of [glucose], [bicarbonate] or pH. 17
What are the therapeutic goals of DKA?
The therapeutic goals of DKA management include optimization of 1) volume status; 2) hyperglycemia and ketoacidosis; 3) electrolyte abnormalities; and 4) potential precipitating factors. The majority of patients with DKA present to the emergency room. Therefore, emergency physicians should initiate the management of hyperglycemic crisis while a physical examination is performed, basic metabolic parameters are obtained, and final diagnosis is made. Several important steps should be followed in the early stages of DKA management: 1 collect blood for metabolic profile before initiation of intravenous fluids; 2 infuse 1 L of 0.9% sodium chloride over 1 hour after drawing initial blood samples; 3 ensure potassium level of >3.3 mEq/L before initiation of insulin therapy (supplement potassium intravenously if needed); 4 initiate insulin therapy only when steps 1–3 are executed.
Can DKA cause hypokalemia?
A “normal” plasma potassium concentration still indicates that total body potassium stores are severely diminished, and the institution of insulin therapy and correction of hyperglycemia will result in hypokalemia.
Is ketoacidosis a type 1 or 2 diabetes?
Diabetic ketoacidosis (DKA) is a rare yet potentially fatal hyperglycemic crisis that can occur in patients with both type 1 and 2 diabetes mellitus. Due to its increasing incidence and economic impact related to the treatment and associated morbidity, effective management and prevention is key. Elements of management include making ...
What is a diabetic ketoacidosis?
Diabetic ketoacidosis (DKA) is a life-threatening condition that develops when cells in the body are unable to get the sugar (glucose) they need for energy because there is not enough insulin. When the sugar cannot get into the cells, it stays in the blood.
What is DKA in diabetes?
Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus. [1] Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion, and occasionally loss of consciousness. [1] A person's breath may develop a specific smell. [1] Onset of symptoms is usually rapid. [1] In some cases people may not realize they previously had diabetes. [1] DKA happens most often in those with type 1 diabetes, but can also occur in those with other types of diabetes under certain circumstances. [1] Triggers may include infection, not taking insulin correctly, stroke, and certain medications such as steroids. [1] DKA results from a shortage of insulin; in response the body switches to burning fatty acids which produces acidic ketone bodies. [3] DKA is typically diagnosed when testing finds high blood sugar, low blood pH, and ketoacids in either the blood or urine. [1] The primary treatment of DKA is with intravenous fluids and insulin. [1] Depending on the severity, insulin may be given intravenously or by injection under the skin. [3] Usually potassium is also needed to prevent the development of low blood potassium. [1] Throughout treatment blood sugar and potassium levels should be regularly checked. [1] Antibiotics may be required in those with an underlying infection. [6] In those with severely low blood pH, sodium bicarbonate may be given; however, its use is of unclear benefit and typically not recommended. [1] [6] Rates of DKA vary around the world. [5] In the United Kingdom, about 4% of people with type 1 diabetes develop DKA each year, while in Malaysia the condition affects about 25% a year. [1] [5] DKA was first described in 1886 and, until the introduction of insulin therapy in the 1920s, it was almost univ Continue reading >>
What is a DKA?
Tweet Diabetic ketoacidosis (DKA) is a dangerous complication faced by people with diabetes which happens when the body starts running out of insulin. DKA is most commonly associated with type 1 diabetes, however, people with type 2 diabetes that produce very little of their own insulin may also be affected.
Can diabetics be treated with insulin?
Usually patients with diabetic ketoacidosis are admitted to the intensive care unit for continuous infusion of insulin; however, the development of rapid acting insulin analogues has made it possible to treat mild to moderate diabetic ketoacidosis with subcutaneous insulin.
Is ketoacidosis a complication of diabetes?
Abstract Background Diabetic ketoacidosis (DKA) is an acute, life-threatening complication of uncontrolled diabetes that mainly occurs in individuals with autoimmune type 1 diabetes, but it is not uncommon in some people with type 2 diabetes.
Can diabetic ketoacidosis be treated?
Diabetic ketoacidosis (DKA), although rare, can occur in these patients, even in the context of hyperinsulinemia, due to impaired insulin signaling. DKA can be extremely challenging to treat, and few clinicians are experienced or comfortable in using the high doses of insulin required.
Can you get ketoacidosis if you have type 1 diabetes?
People with type 1 diabetes are at risk for ketoacidosis, since their bodies don't make any insulin. Your ketones can also go up when you miss a meal, you're sick or stressed, or you have an insulin reaction. DKA can happen to people with type 2 diabetes, but it's rare.
What is the best treatment for DKA?
The use of intravenous fluid therapy with isotonic fluids to correct fluid deficits and acid-base and electrolyte imbalances is recommended. Many protocols for treatment of DKA exist but IV fluids and rapid-acting insulin (regular) must be administered first to quickly decrease hyperglycemia.
What is the risk of diabetic ketoacidosis?
Diabetic ketoacidosis occurs when the body cannot produce enough insulin. The signs and symptoms of diabetic ketoacidosis include Risk factors for diabetic ketoacidosis are type 1 diabetes, and missing insulin doses frequently, or being exposed to a stressor requiring higher insulin doses (infection, etc).
What are the risk factors for DKA?
Risk factors for DKA include new diagnosis of diabetes mellitus, insulin omission, infection, myocardial infarc Continue reading >>. Type 1 diabetes as common in adults as children, but many adults misdiagnosed. Diabetic emergencies: Warning signs and what to do.
What is the transition from IV to SQ insulin?
This review article suggests a stepwise approach to the transition in order to promote safety and euglycemia. Important components of the transition include evaluating the patient and clinical situation for appropriateness, recognizing factors that influence a safe transition, calculation of proper SQ insulin doses, and deciding the appropriate type of SQ insulin. This article addresses other clinical situations including the management of patients previously on insulin pumps and recommendations for patients requiring glucocorticoids and enteral tube feedings. The use of institutional and computerized protocols is discussed. Further research is needed regarding the transition management of subgroups of patients such as those with type 1 diabetes and end-stage renal disease. Introduction Intravenous (IV) insulin is used in the hospitalized patient to control blood sugars for patients with and without diabetes who may exhibit uncontrolled hyperglycemia or for those who need close glycemic attention. Common hospital uses for IV insulin include the perioperative setting, during the use of high-risk medications (such as corticosteroids), or during crises such as diabetic ketoacidosis (DKA) [1,2]. Other conditions such as hyperglycemic hyperosmolar state (HHS) and trauma frequently require IV insulin, as well as specific hospital units such as the cardiothoracic intensive care unit [3,4]. The correlation between hyperglycemia and poor inpatient outcomes has been well described in the literature [5,6]. The treatment of hyperglycemia using an IV Continue reading >>
Can diabetes cause DKA?
Infection, injury, a serious illness, missing doses of insulin shots, or surgery can lead to DKA in people with type 1 diabetes. People with type 2 diabetes can also develop DKA, but it is less common. It is usually triggered by uncontrolled blood sugar, missing doses of medicines, or a severe illness.
What is the condition called when you have high levels of ketones?
As fat is broken down, acids called ketones build up in the blood and urine. In high levels, ketones are poisonous. This condition is known as ketoacidosis. Diabetic ketoacidosis (DKA) is sometimes the first sign of type 1 diabetes in people who have not yet been diagnosed. It can also occur in someone who has already been diagnosed with type 1 diabetes. Infection, injury, a serious illness, missing doses of insulin shots, or surgery can lead to DKA in people with type 1 diabetes. People with type 2 diabetes can also develop DKA, but it is less common. It is usually triggered by uncontrolled blood sugar, missing doses of medicines, or a severe illness. Continue reading >>
What is DKA in diabetes?
Diabetic ketoacidosis (DKA) is a serious, life-threatening complication of diabetes mellitus . DKA is characterized by the triad of hyperglycemia, anion gap metabolic acidosis, and ketonemia. It is part of a spectrum of hyperglycemia on which lies hyperosmolar hyperglycemic state (HHS). Though the two are distinct entities, they do share some commonalities. DKA is caused by the reduced effect of insulin, either due to deficit or reduction of levels, with concomitant elevation of counter regulatory hormones (glucagon, catecholamines, cortisol, and growth hormones), generally due to a precipitating stress. Increased gluconeogenesis, glycogenolysis, and decreased glucose uptake by cells leads to hyperglycemia, while insulin deficiency leads to mobilization and oxidization of fatty acids leading to ketogenesis. Although DKA may be the initial manifestation of diabetes, it is typically precipitated by other factors. It is critical for a clinician to identify and treat these factors. Infection can be found in 40-50% of patients with hyperglycemic crisis, with urinary tract infection and pneumonia accounting for the majority of cases. DKA is a life-threatening medical emergency with a mortality rate just under 5% in individuals under 40 years of age, but with a more serious prognosis in the elderly, who have mortality rates over 20%. Deaths may also occur as a result of hypokalemia induced arrhythmias and cerebral edema (more common in children). II. Diagnostic confirmation: are you sure your patient has diabetic ketoacidosis? Although the diagnosis of DKA can be suspected on clinical grounds, confirmation is based on laboratory tests including potential hydrogen (pH) level, urinalysis, and basic metabolic profile. summarizes the biochemical criteria for the diagnosis and asse Continue reading >>
