How does the urethral sphincter control micturition?
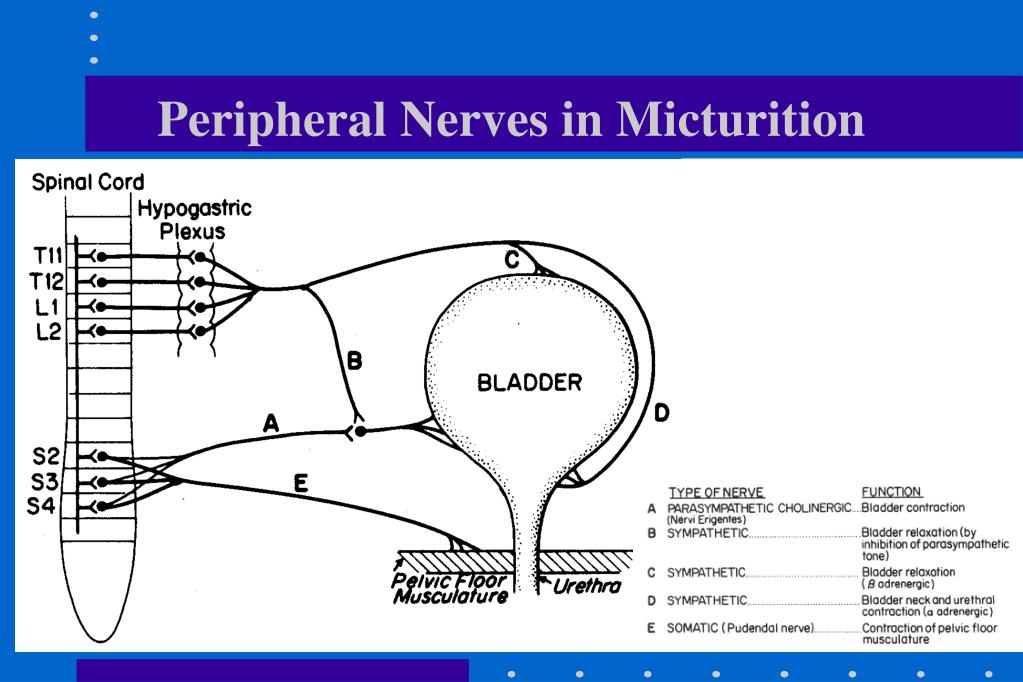
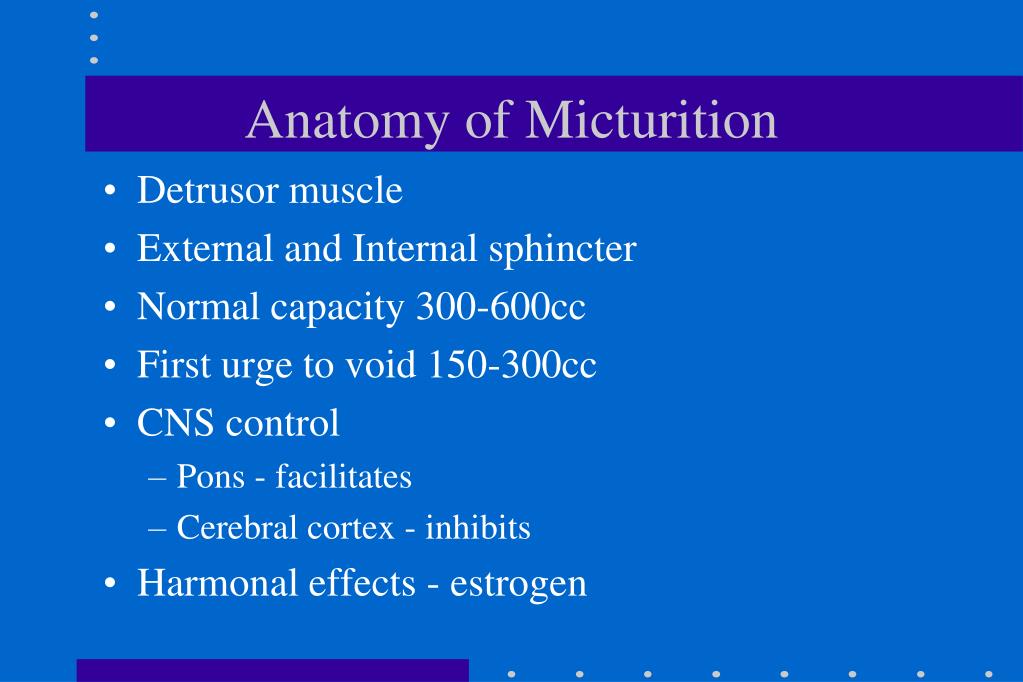
The urethral sphincter can be used to control micturition. Voiding urine begins with voluntary relaxation of the external sphincter muscle of the bladder. Parasympathetic impulses induce contractions of the bladder and relaxation of the internal sphincter [18].
What are the two muscles that surround the urethral sphincter?
ANATOMY OF THE URETHRAL SPHINCTER Within the deep perineal pouch, a group of muscle fibers surround the urethra and form the urethral sphincter [5]. Two muscles as urethral sphincters are used to control the exit of urine in the urinary bladder through the urethra. The two muscles are the internal and EUS. IUS
What does the urethrovaginal sphincter do?
The urethrovaginal sphincter (M. sphincter urethrovaginalis) is a thin, flat, and broad muscle. This muscle intermingles ventrally with the compressor urethral muscle. These muscle fibers begin on the ventral side of the urethra to extend dorsally along the lateral wall of the urethra.
How do you relax a tight sphincter muscle?
Using Simple Relaxation Techniques Practice deep breathing while focusing on your sphincter muscles. Meditate to get rid of stress and release the tension in your muscles. Massage your lower stomach with your fingers. Prop your feet up in a seated position to relax your pelvic muscles. Use your finger to relax your sphincter if nothing else works.
What causes relaxation of the internal urethral sphincter?
FUNCTION OF THE URETHRAL SPHINCTER Voiding urine begins with voluntary relaxation of the external sphincter muscle of the bladder. Parasympathetic impulses induce contractions of the bladder and relaxation of the internal sphincter [18].
How do you relax the urethral sphincter?
To perform, squeeze your pelvic floor muscles — as if you're trying to stop your stream of urine — for three seconds. Relax for a count of three and repeat several times. Your doctor might recommend that you do a set of these exercises three or four times a day, lying down, sitting and standing.
What drug can be used to help relax the urinary sphincter?
Mirabegron (Myrbetriq) Mirabegron is a medication approved to treat certain types of urinary incontinence. It relaxes the bladder muscle and can increase the amount of urine your bladder can hold.
What activates the internal urethral sphincter?
When the bladder is full of urine, stretch receptors in the bladder wall trigger the micturition reflex. The detrusor muscle that surrounds the bladder contracts. The internal urethral sphincter relaxes, allowing for urine to pass out of the bladder into the urethra. Both of these reactions are involuntary.
How do you strengthen your internal urethral sphincter?
How to perform kegel exercisesSit on the toilet and start to urinate.Try to stop the flow of urine midstream by contracting your pelvic floor muscles.Repeat this action several times until you become familiar with the feel of contracting the correct group of muscles. ... This method of contraction is a kegel exercise.
What system inhibits the internal urethral sphincter?
Parasympathetic nervous systemParasympathetic nervous system ACTIVATES urination via: - Detrusor muscle activation - Internal urethral sphincter inhibition.
What can I take instead of oxybutynin?
Other medications prescribed for overactive bladder include darifenacin (Enablex), fesoterodine (Toviaz), mirabegron (Myrbetriq), solifenacin (Vesicare), tolterodine (Detrol), and trospium (Sanctura).
Which is better oxybutynin or Myrbetriq?
Ditropan (oxybutynin) is good treatment for overactive bladder, but has more side-effects like dry mouth and constipation than other medicines that work similarly. Myrbetriq (mirabegron) helps you to have better control over your urination.
What is the best medication for urinary retention?
A combination of a 5-alpha-reductase inhibitor and an alpha-blocker, such as finasteride and doxazosin or dutasteride and tamsulosin, may work better than an individual medicine alone. Antibiotics link treat infections that may cause urinary retention, such as urinary tract infections and prostatitis.
How do you activate an artificial sphincter?
To use the sphincter, compress (squeeze) the pump so that fluid is diverted from the urethral cuff to the balloon. This action enables the sphincter to relax, which in turn, enables you to urinate. The cuff re-inflates on its own in three to five minutes.
Can a damaged urinary sphincter be repaired?
Conclusions: The use of modified ventral onlay graft urethroplasty, using particular non-aggressive steps, is a suitable surgical technique for repair of sphincter urethral stricture in patients who underwent BPH transurethral surgery, using different procedures (TURP, HOLEP, TUIP).
What type of muscle makes up the internal urethral sphincter?
smooth muscleThe internal sphincter muscle of urethra: located at the bladder's inferior end and the urethra's proximal end at the junction of the urethra with the urinary bladder. The internal sphincter is a continuation of the detrusor muscle and is made of smooth muscle, therefore it is under involuntary or autonomic control.
What is the term for the inner sphincter?
Inner sphincter: The term 'overactive bladder' is used to describe dis synergy of the bladder muscle -not contracting in coordinated fashion; this leads to loss of reg ... Read More
What is contraction in the sphincter?
A muscle contraction: When muscles contract they shorten. In the sphincter, the muscles are laid in a circular fashion around the opening that passes urine at the base of t ... Read More
Which part of the body carries urine out of the body?
Neurologically: The urinary or urethral sphincter encircles the lower part of the bladder and the tubing (urethra) that carries the urine out of the body. It is compo ... Read More
Do alpha blockers relax the prostate?
Both: Alpha blockers relax the smooth muscle component of the prostate (as opposed to the glandular part). They also relax the INTERNAL urinary sphincter at ... Read More. 1 doctor agrees. 0. 0 comment.
What is the urethral sphincter?
The urethral sphincter is made up of a number of muscular components which act together to control micturition and maintain urinary continence. The internal urethral sphincter is a poorly developed circular bundle of smooth muscle fibers situated around the proximal end of the urethra, at the neck of the bladder.
What are the two sphincters that control the flow of urine?
In simple terms we can divide this complex into two urethral sphincters; an internal urethral sp hincter and an external ureth ral sphincter. The internal ureth ral sphincter is located at the junction ...
What is the female external urethral sphincter?
The innermost part, the female external urethral sphincter proper, consists of circular muscle fibers located around the proximal two thirds of the female urethra.
What is the difference between a male and female urethral sphincter?
The male external urethral sphincter, sometimes called the rhabdosphincter muscle, is situated just inferior to the prostate.
Which muscle is closely related to the puborectalis?
In females, the striated muscle of the external urethral sphincter is closely related to the puborectalis component of the levator ani muscle, while inferiorly it blends with the smooth muscle of the urethra and vagina. Male urinary bladder.
Which muscle is closely related to the urethral sphincter?
The external urethral sphincter is closely related to the levator ani, deep transverse perineal and rectourethral muscles. The puboperineal component of the levator ani muscle, forms an open circle around the external sphincter creating a hiatus at the ventral aspect.
Where is the external urethral sphincter located?
The external urethral sphincter is located distal to the internal urethral sphincter, in the deep perineal pouch. Its skeletal muscle fibers arise from the ischial rami, inferior pubic rami and adjacent fascia, extending to surround the middle-lower, membranous, part of the urethra.
What is the urethrovaginal sphincter?
The urethrovaginal sphincter (M. sphincter urethrovaginalis) is a thin, flat, and broad muscle [26]. This muscle intermingles ventrally with the compressor urethral muscle [26]. These muscle fibers begin on the ventral side of the urethra to extend dorsally along the lateral wall of the urethra [19].
Which nervous system relaxes the internal sphincter muscle during micturition?
The sympathetic nervous system maintains tonic contractions of the internal urethral muscle [18]. However, the parasympathetic nervous system relaxes the internal sphincter muscle during micturition [18]. The IUS is made of a layer of smooth muscle, which is surrounded by layers of striated muscle [19,20].
How is urine prevented?
Urination is prevented by the voluntary motor innervation of the EUS muscle. The striated sphincter is innervated by the pudendal nerve from the S2 to S4 nerve roots [28,29]. The neurons that innervate the urethral sphincter originate in the cord, in an area termed Onuf's nucleus [30].
What causes urinary incontinence?
Especially, insufficient strength of the pelvic floor muscles including the urethral sphincter muscles causes urinary incontinence (UI). Thus, it is most important to understand the main mechanism causing UI and the relationship of UI with the urethral sphincter. Functionally and anatomically, the urethral sphincter is made up ...
What is the deep pouch in the pelvic diaphragm?
This deep pouch refers to the region between the PM and the pelvic diaphragm. In both men and women, where the urethra passes through the deep pouch, it is surrounded by skeletal muscles called the EUS [23]. The EUS is a secondary sphincter to control the flow of urine through the urethra.
How far does the urethra go from the bladder to the external urinary tract?
The urethra passes from the bladder to the external urinary meatus for a distance of about 4 cm [12]. Although in females the urethra is used only for urinating, the relationship of the urethra with the vagina is functionally important to the muscular pelvic floor after vaginal delivery of a baby [13].
Which muscle is responsible for controlling micturition?
The urethral sphincter can be used to control micturition. Voiding urine begins with voluntary relaxation of the external sphincter muscle of the bladder. Parasympathetic impulses induce contractions of the bladder and relaxation of the internal sphincter [18].
How to relax sphincter muscles?
1. Practice deep breathing while focusing on your sphincter muscles. Breathe in slowly and deeply for about 4 seconds, then exhale slowly for another 4 seconds. As you do this, concentrate on how your sphincter muscles feel. As you feel the other muscles in your body relax, allow your sphincter to relax as well.
How to get rid of sphincter pain?
Apply lubrication to your index finger, then insert your finger into your anus. Move your finger around in a circular motion until your sphincter muscles relax. This process may take a few minutes, but as long as you're using lubrication, it shouldn't be too painful. [4]
Why is my sphincter tight?
If you've suffered from constipation or tight sphincter muscles for 2 weeks or longer , it may be due to a broader medical condition. Your doctor might be able to tell you what's making it difficult for you to relax your sphincter and what you may need to do in order to fix it.
How to practice deep breathing?
To practice deep breathing, try inhaling deeply to a count of 4, then exhaling slowly for another count of 4. Often, it’s easier to release your muscles after tightening them, so squeeze your sphincter muscles as if you’re trying to not pass gas. Then, slowly release the muscles as you practice your deep breathing.
Where is the sphincter located?
Your sphincter muscles are located around your anus and are vitally important to the defecation process. However, if you're stressed or have an underlying medical condition, it may be hard for you to relax these muscles during a bowel movement. Luckily, there are several techniques you can use to help relax your sphincter.
How long does it take to see improvement in a sphincter?
It's often used to strengthen the rectal sphincter, but can also be used to teach you how to relax your sphincter. It usually takes about 3 sessions with a specialist to start seeing improvement in your symptoms.
How to clear your mind and expel tension?
For best results, meditate in a quiet, distraction-free environment. This will make it easier for you to clear your mind and expel the tension in your body. Don't be discouraged if meditation doesn't work the first time you try it. You may need to practice it a few times.
Abstract
This study evaluates the diagnostic value of poorly relaxed external sphincter (PRES) in men with voiding dysfunction. We analyzed clinical and video-urodynamic characteristics to identify predictive factors of PRES in patients with lower urinary tract symptoms (LUTS) refractory to α-1 adrenoceptor blocker (α-blocker) therapy.
1 INTRODUCTION
Lower urinary tract symptoms (LUTS) are bothersome symptoms that increase with age in both men and women, 1 and approximately 20% of middle aged–elderly men have LUTS severe enough to interfere with quality of life. 2 LUTS are composed of both voiding and storage symptoms.
2 METHODS
All consecutive male patients with LUTS refractory to α-blocker treatment for at least 1 month in a single tertiary medical center between 1997 and 2013 were included in this study. A total of 3379 patients were enrolled.
3 RESULTS
Of the 3379 men included in the study who completed the video-urodynamic studies, 2078 were diagnosed with voiding dysfunction based on video-urodynamic studies. Another 138 (138/2216, 6.2%) had LUTS with normal video-urodynamic results and served as the healthy control group for comparison.
4 DISCUSSION
In the present study, BPO remained the most common cause of voiding dysfunction in middle aged–elderly men with LUTS. Moreover, the prevalence of BND and PRES is increased in the α-blocker-refractory group.
5 CONCLUSION
In this study, we established a simple scale to predict PRES in the office setting using clinical symptoms and examinations that can be done without invasive urodynamic studies. The scale is composed of three parameters: voided volume, TPV, and urgency/UUI symptoms.